Abstract
Purpose
In this study, a bidirectional mendelian randomization was applied to evaluate the association of smoking and alcohol consumption with 11 otolaryngological diseases.
Methods
A total of 85,22,34 and 7 single nucleotide polymorphisms were used as instrumental variables for smoking initiation, cigarettes per day, alcoholic drinks per week and alcohol consumption, respectively. Genetic associations with 11 common otolaryngological diseases were obtained from the UK Biobank and FinnGen dataset. IVW, weighted median, MR-Egger, MR-PRESSO and leave-one-out method were used in this analysis.
Results
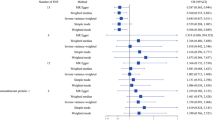
Smoking initiation increased the risk of vocal cord and larynx diseases (OR 1.002; 95% CI 1.001–1.004; P = 4 × 10–4), head and neck cancer (OR 1.001; 95% CI 0.999–1.003; P = 0.027), thyroid cancer (OR 1.538; 95% CI 1.006–2.351; P = 0.047) and sleep apnoea (OR 1.286; 95% CI 1.099–1.506; P = 0.002). Cigarettes per day was associated with chronic sinusitis (OR 1.152; 95% CI 1.002–1.324; P = 0.046), chronic rhinitis and pharyngitis (OR 1.200; 95% CI 1.033–1.393; P = 0.017), vocal cord and larynx diseases (OR 1.001; 95% CI 0.999–1.002; P = 0.021) and head and neck cancer (OR 1.001; 95% CI 0.999–1.003; P = 0.017). Alcoholic drinks per week only was significantly associated with the risk of head and neck cancer (OR 1.003; 95% CI 1.001–1.006; P = 0.014). However, there was no evidence to support that genetically predicted alcohol consumption increased the risk of otolaryngological diseases. Reverse MR also did not find outcomes effect on exposures.
Conclusion
This study shows that smoking and heavy alcohol consumption promote the occurrence of some otolaryngological diseases indicating that lifestyle modification might be beneficial in preventing otolaryngological diseases.

Similar content being viewed by others
Data availability
All data used to support the findings of this study are available from the corresponding author upon request.
References
Lugg ST, Scott A, Parekh D et al (2022) Cigarette smoke exposure and alveolar macrophages: mechanisms for lung disease. Thorax 771:94–101
Messner B, Bernhard D (2014) Smoking and cardiovascular disease: mechanisms of endothelial dysfunction and early atherogenesis. Arterioscler Thromb Vasc Biol 343:509–515
Rumgay H, Murphy N, Ferrari P et al (2021) Alcohol and cancer: epidemiology and biological mechanisms. Nutrients 13(9):3173
Hisinger-Mölkänen H, Piirilä P, Haahtela T et al (2018) Smoking, environmental tobacco smoke and occupational irritants increase the risk of chronic rhinitis. World Allergy Organ J 111:6
Christensen DN, Franks ZG, McCrary HC et al (2018) A systematic review of the association between cigarette smoke exposure and chronic rhinosinusitis. Otolaryngol Head Neck Surg 1585:801–816
Hsu WY, Chiu NY, Chang CC et al (2019) The association between cigarette smoking and obstructive sleep apnea. Tob Induc Dis 17:27
Chang CP, Siwakoti B, Sapkota A et al (2020) Tobacco smoking, chewing habits, alcohol drinking and the risk of head and neck cancer in Nepal. Int J Cancer 1473:866–875
Wan JY, Cataby C, Liem A et al (2020) Evidence for gene-smoking interactions for hearing loss and deafness in Japanese American families. Hear Res 387:107875
Yeo Y, Shin DW, Han K et al (2022) Smoking, alcohol consumption, and the risk of thyroid cancer: a population-based Korean cohort study of 10 million people. Thyroid 324:440–448
Di Credico G, Polesel J, Dal Maso L et al (2020) Alcohol drinking and head and neck cancer risk: the joint effect of intensity and duration. Br J Cancer 1239:1456–1463
Simou E, Britton J, Leonardi-Bee J (2018) Alcohol and the risk of sleep apnoea: a systematic review and meta-analysis. Sleep Med 42:38–46
Qian P, Zhao Z, Liu S et al (2023) Alcohol as a risk factor for hearing loss: a systematic review and meta-analysis. PLoS ONE 181:e0280641
Connor A, Emdin AVK, Kathiresan S (2017) Mendelian randomization. JAMA 31819:1925–1926
Skrivankova VW, Richmond RC, Woolf BAR et al (2021) Strengthening the reporting of observational studies in epidemiology using mendelian randomization: the STROBE-MR statement. JAMA 32616:1614–1621
Davies NM, Holmes MV, Davey Smith G (2018) Reading Mendelian randomisation studies: a guide, glossary, and checklist for clinicians. BMJ 362:k601
Hemani G, Zheng J, Elsworth B et al (2018) The MR-Base platform supports systematic causal inference across the human phenome. Elife https://doi.org/10.7554/eLife.34408
Burgess S, Thompson SG (2011) Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol 403:755–764
Burgess S, Butterworth A, Thompson SG (2013) Mendelian randomization analysis with multiple genetic variants using summarized data. Genet Epidemiol 377:658–665
Bowden J, Davey Smith G, Haycock PC et al (2016) Consistent estimation in Mendelian randomization with some invalid instruments using a weighted median estimator. Genet Epidemiol 404:304–314
Bowden J, Davey Smith G, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 442:512–525
Cohen JF, Chalumeau M, Cohen R et al (2015) Cochran’s Q test was useful to assess heterogeneity in likelihood ratios in studies of diagnostic accuracy. J Clin Epidemiol 683:299–306
Bowden J, Spiller W, Del Greco MF et al (2018) Improving the visualization, interpretation and analysis of two-sample summary data Mendelian randomization via the Radial plot and Radial regression. Int J Epidemiol 474:1264–1278
Verbanck M, Chen CY, Neale B et al (2018) Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet 505:693–698
Hutson K, Clark A, Hopkins C et al (2021) Evaluation of Smoking as a Modifying Factor in Chronic Rhinosinusitis. JAMA Otolaryngol Head Neck Surg 1472:159–165
Di Credico G, Edefonti V, Polesel J et al (2019) Joint effects of intensity and duration of cigarette smoking on the risk of head and neck cancer: a bivariate spline model approach. Oral Oncol 94:47–57
Cho A, Chang Y, Ahn J et al (2018) Cigarette smoking and thyroid cancer risk: a cohort study. Br J Cancer 1195:638–645
Zhang Z, Li G, Yu L et al (2023) Causal relationships between potential risk factors and chronic rhinosinusitis: a bidirectional two-sample Mendelian randomization study. Eur Arch Otorhinolaryngol 2806:2785–2793
Gormley M, Dudding T, Sanderson E et al (2020) A multivariable Mendelian randomization analysis investigating smoking and alcohol consumption in oral and oropharyngeal cancer. Nat Commun 111:6071
Hu H, Sasaki N, Ogasawara T et al (2019) Smoking, smoking cessation, and the risk of hearing loss: Japan epidemiology collaboration on occupational health study. Nicotine Tob Res 214:481–488
Tarhun YM (2020) The effect of passive smoking on the etiology of serous otitis media in children. Am J Otolaryngol 413:102398
Wang S, Qi L, Wei H et al (2022) Smoking behavior might affect allergic rhinitis and vasomotor rhinitis differently: a Mendelian randomization appraisal. World Allergy Organ J 152:100630
Marziliano A, Teckie S, Diefenbach MA (2020) Alcohol-related head and neck cancer: Summary of the literature. Head Neck 424:732–738
Koo HY, Han K, Shin DW et al (2021) Alcohol drinking pattern and risk of head and neck cancer: a nationwide cohort study. Int J Environ Res Public Health 18(21):11204
Denissoff A, Huusko T, Ventelä S et al (2022) Exposure to alcohol and overall survival in head and neck cancer: a regional cohort study. Head Neck 4410:2109–2117
Lomholt FK, Nielsen SF, Nordestgaard BG (2016) High alcohol consumption causes high IgE levels but not high risk of allergic disease. J Allergy Clin Immunol 1385:1404-1413.e1413
Skaaby T, Kilpeläinen TO, Taylor AE et al (2019) Association of alcohol consumption with allergic disease and asthma: a multi-centre Mendelian randomization analysis. Addiction 1142:216–225
Burgos-Sanchez C, Jones NN, Avillion M et al (2020) Impact of alcohol consumption on snoring and sleep apnea: a systematic review and meta-analysis. Otolaryngol Head Neck Surg 1636:1078–1086
Kolla BP, Foroughi M, Saeidifard F et al (2018) The impact of alcohol on breathing parameters during sleep: a systematic review and meta-analysis. Sleep Med Rev 42:59–67
De Schryver E, Derycke L, Campo P et al (2017) Alcohol hyper-responsiveness in chronic rhinosinusitis with nasal polyps. Clin Exp Allergy 472:245–253
Hong SH, Myung SK, Kim HS (2017) Alcohol intake and risk of thyroid cancer: a meta-analysis of observational studies. Cancer Res Treat 492:534–547
Sen A, Tsilidis KK, Allen NE et al (2015) Baseline and lifetime alcohol consumption and risk of differentiated thyroid carcinoma in the EPIC study. Br J Cancer 1135:840–847
Zong D, Liu X, Li J et al (2019) The role of cigarette smoke-induced epigenetic alterations in inflammation. Epigenetics Chromatin 121:65
de la Iglesia JV, Slebos RJC, Martin-Gomez L et al (2020) Effects of tobacco smoking on the tumor immune microenvironment in head and neck squamous cell carcinoma. Clin Cancer Res 266:1474–1485
Ferraguti G, Terracina S, Petrella C et al (2022) Alcohol and head and neck cancer: updates on the role of oxidative stress, genetic, epigenetics, oral microbiota, antioxidants, and alkylating agents. Antioxidants (Basel) 111:145
Rigotti NA, Kruse GR, Livingstone-Banks J et al (2022) Treatment of tobacco smoking: a review. JAMA 3276:566–577
Acknowledgements
We would like to express our gratitude to UK biobank dataset and Finngen study for sharing data. Thanks to all the peer reviewers for their opinions and suggestions.
Funding
This work was supported by funding from Tianjin Natural Science Foundation (number: 21JCYBJC00890) and Science and Technology Project of Tianjin Health Commission (Grant numbers: ZC20014).
Author information
Authors and Affiliations
Contributions
Conceptualization, XW, YB; data curation, XW, YB and GL; funding acquisition, HC; methodology, HC; software, XW, YB, GL and WW; supervision, HC; visualization, XW, YB; writing—original draft, XW; writing—review and editing, HC.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Ethics approval
The included studies have been approved by the appropriate institutional review boards and ethics committees and all participants have signed the informed consent.
Consent for publication
All of the authors have agreed to the submission and publication of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
405_2023_8246_MOESM1_ESM.docx
Supplementary Fig. 1 Scatter plots for single-nucleotide polymorphisms associated with smoking effect on Vocal cord and larynx diseases, Head and neck cancer, Thyroid cancer and Sleep apnoea (DOCX 740 KB)
405_2023_8246_MOESM2_ESM.docx
Supplementary Fig. 2. Scatter plots for single-nucleotide polymorphisms associated with cigarettes per day effect on chronic sinusitis, chronic rhinitis and pharyngitis, vocal cord and larynx diseases and head and neck cancer (DOCX 18 KB)
405_2023_8246_MOESM3_ESM.docx
Supplementary Fig. 3 Scatter plots for single-nucleotide polymorphisms associated with alcoholic drinks per week effect on Head and neck cancer (DOCX 396 KB)
405_2023_8246_MOESM4_ESM.docx
Supplementary file 1 The detailed summary of instrumental variables associated with smoking initiation, cigarettes per day, alcohol consumption and alcoholic drinks per week (DOCX 22 KB)
405_2023_8246_MOESM5_ESM.docx
Supplementary file 2 Palindromic sequences of smoking initiation, cigarettes per day and alcohol consumption (DOCX 23 KB)
405_2023_8246_MOESM6_ESM.docx
Supplementary file 3 Assessing the proportion of phenotypic variation (R2) and weak instrument bias (F statistics) (DOCX 16 KB)
405_2023_8246_MOESM7_ESM.docx
Supplementary file 4 The detailed summary of instrumental variables associated with vocal cord and larynx diseases (DOCX 79 KB)
405_2023_8246_MOESM8_ESM.docx
Supplementary file 5 Assessing the proportion of phenotypic variation (R2) and weak instrument bias (F statistics) in the reverse MR analysis (DOCX 694 KB)
405_2023_8246_MOESM10_ESM.docx
Supplementary file 7 MR leave-one-out sensitivity analysis for smoking initiation on vocal cord and larynx diseases, head and neck cancer, thyroid cancer and sleep apnoea (DOCX 156 KB)
405_2023_8246_MOESM11_ESM.docx
Supplementary file 8 The MR-PRESSO method of Smoking and drinking behaviours on several otolaryngological diseases (DOCX 34 KB)
405_2023_8246_MOESM12_ESM.docx
Supplementary file 9 MR leave-one-out sensitivity analysis for cigarettes per day on chronic sinusitis, chronic rhinitis and pharyngitis, head and neck cancer and vocal cord and larynx diseases (DOCX 16 KB)
405_2023_8246_MOESM14_ESM.docx
Supplementary file 11 MR leave-one-out sensitivity analysis for alcoholic drinks per week on head and neck cancer (DOCX 23 KB)
405_2023_8246_MOESM15_ESM.docx
Supplementary file 12 Mendelian randomisation results of several otolaryngological diseases on the smoking and drinking behaviours (DOCX 22 KB)
405_2023_8246_MOESM16_ESM.docx
ssSupplementary file 13 Leave-one-out sensitivity analysis for several otolaryngological diseases on smoking and drinking behaviours (DOCX 19 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, X., Bi, Y., Liu, G. et al. Smoking and alcohol consumption with the risk of 11 common otolaryngological diseases: a bidirectional Mendelian randomization. Eur Arch Otorhinolaryngol 280, 5615–5623 (2023). https://doi.org/10.1007/s00405-023-08246-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-023-08246-9