Abstract
Objective
To evaluate hearing results and outcome using two different surgical techniques (microdrill and CO2 Laser fenestration) in the treatment of conductive hearing loss in patients with otosclerosis.
Study design
Retrospective audiometric database and chart review from January 2005 until December 2016.
Setting
Two tertiary referral hospitals
Materials and methods
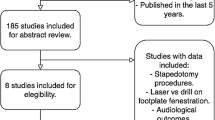
Seven-hundred forty-two primary stapedotomy have been reviewed retrospectively in two referral hospitals. This multicenter study compared 424 patients operated for otosclerosis with microdrill technique and 318 patients operated with CO2 laser assisted stapedotomy. Preoperative and postoperative audiological assessment (following the recommendations of the Committee on Hearing and Equilibrium) were compared between the two groups at least 6 weeks and at 1 year or more. Measure of overclosure and hearing damage have been analyzed and compared between the groups.
Results
There were no statistically significant differences in demographic data between the two groups and no statistically significant difference in hearing outcome between the two groups. CO2 Laser with 0.4 piston showed slightly better results to close the air–bone gap postoperatively to ≤ 10 dB (84% as compared with the 80% of patients operated with microdrill technique). Patients operated with microdrill technique and 0.6 piston have less damage to hearing at 4 kHz.
Conclusion
The use of CO2 laser seems associated with better postoperative air–bone gap closure. However, it carries more risk of hearing damage at 4 kHz at it is the case for the microdrill at 1 kHz. In general, postoperative hearing outcome using these two surgical techniques is comparable.
Similar content being viewed by others
References
Menger DJ, Tange RA (2003) The aetiology of otosclerosis: a review of the literature. Clin Otolaryngol Allied Sci 28(2):112–120
Nazarian R, McElveen JT Jr, Eshraghi AA (2018) History of Otosclerosis and stapes surgery. Otolaryngol Clin N Am 51(2):275–290
Mudry A (2006) Adam Politzer (1835–1920) and the description of otosclerosis. Otol Neurotol 27(2):276–281
Chole RA, McKenna M (2001) Pathophysiology of otosclerosis. Otol Neurotol 22(2):249–257
Holmgren G (1992) The surgery of otosclerosis. 1937. Ann Otol Rhinol Laryngol 101(7):546–555
Sourdille M (1937) New technique in the surgical treatment of severe and progressive deafness from otosclerosis. Bull N Y Acad Med 13(12):673–691
Lempert J (1938) Improvement of hearing in cases of otosclerosis: a new, one stage surgical technic. Arch Otolaryngol 28(1):42–97
Shea JJ Jr (1958) Fenestration of the oval window. Ann Otol Rhinol Laryngol 67(4):932–951
Palva T (1987) Argon laser in otosclerosis surgery. Acta Otolaryngol 104(1–2):153–157
Perkins RC (1980) Laser stepedotomy for otosclerosis. Laryngoscope 90(2):228–240
Barbara M, Lazzarino AI, Murè C, Macrì C, Volpini L, Monini S (2011) Laser versus drill-assisted stapedotomy for the treatment of otosclerosis: a randomized-controlled trial. Int Adv Otol 7:283–288
Wegner I, Kamalski DM, Tange RA, Vincent R, Stegeman I, van der Heijden GJ, Grolman W (2014) Laser versus conventional fenestration in stapedotomy for otosclerosis: a systematic review. Laryngoscope 124(7):1687–1693
Just T, Guder E, Pau HW (2012) Effect of the stapedotomy technique on early post-operative hearing results-preliminary results. Auris Nasus Larynx 39(4):383–386
Brase C, Keil I, Schwitulla J, Mantsopoulos K, Schmid M, Iro H, Hornung J (2013) Bone conduction after stapes surgery: comparison of CO2 laser and manual perforation. Otol Neurotol 34(5):821–826
Cuda D, Murri A, Mochi P, Solenghi T, Tinelli N (2009) Microdrill, CO2-laser, and piezoelectric stapedotomy: a comparative study. Otol Neurotol 30(8):1111–1115
American Academy of Otolaryngology-Head and Neck Surgery Foundation, Inc. (1995) Committee on Hearing and Equilibrium guidelines for the evaluation of results of treatment of conductive hearing loss. Otolaryngol Head Neck Surg 113(3):186–187
Watson GJ, da Cruz M (2018) Reporting in stapes surgery: are we following the guidelines? J Laryngol Otol 132(6):479–485
Ren DD, Chi FL (2008) Experimental study on thermic effects, morphology and function of guinea pig cochlea: acomparison between the erbium:yttrium-aluminum-garnet laser and carbon dioxide laser. Lasers Surg Med 40(6):407–414
Loewenthal M, Jowett N, Busch CJ, Knecht R, Dalchow CV (2015) A comparison of hearing results following stapedotomy under local versus general anesthesia. Eur Arch Otorhinolaryngol 272(9):2121–2127
Markou K, Goudakos J (2009) An overview of the etiology of otosclerosis. Eur Arch Otorhinolaryngol 266(1):25–35
Kishimoto M, Ueda H, Uchida Y, Sone M (2015) Factors affecting postoperative outcome in otosclerosis patients: predictive role of audiological and clinical features. Auris Nasus Larynx 42(5):369–373
aWengen DF, Pfaltz CR, Uyar Y (1992) The influence of age on the results of stapedectomy. Eur Arch Otorhinolaryngol 249(1):1–4
Mann WJ, Amedee RG, Fuerst G, Tabb HG (1996) Hearing loss as a complication of stapes surgery. Otolaryngol Head Neck Surg 115(4):324–328
Pavillon-Maisonnier C, Faure F, Plouin-Gaudon I, Truy E (2007) Labyrinthitis, or inflammatory pseudotumor after stapedectomy. Ann Otolaryngol Chir Cervicofac 124(6):322–325
Bernardeschi D, De Seta D, Canu G, Russo FY, Ferrary E, Lahlou G, Sterkers O (2018) Does the diameter of the stapes prosthesis really matter? A prospective clinical study. Laryngoscope 128(8):1922–1926. https://doi.org/10.1002/lary.27021 (Epub 2017 Nov 24)
Wegner I, Eldaebes MM, Landry TG, Grolman W, Bance ML (2016) The effect of piston diameter in stapedotomy for otosclerosis: a temporal bone model. Otol Neurotol 37(10):1497–1502
Dhooge I, Desmedt S, Maly T, Loose D, Van Hoecke H (2018) Long-term hearing results of stapedotomy: analysis of factors affecting outcome. Eur Arch Otorhinolaryngol 275(5):1111–1119
Somers T, Vercruysse JP, Zarowski A, Verstreken M, Schatteman I, Offeciers FE (2007) Transient depression of inner ear function after stapedotomy: skeeter versus CO(2) laser technique. Adv Otorhinolaryngol 65:267–272
Acknowledgements
We thank Pierre Pradat (Hôpital de la Croix Rousse, Hospices Civils de Lyon) for help in statistical analysis, and Philip Robinson (DRCI, Hospices Civils de Lyon) for help in manuscript preparation.
Funding
The authors declare that no funding was received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Altamami, N.M., Huyghues des Etages, G., Fieux, M. et al. Is one of these two techniques: CO2 laser versus microdrill assisted stapedotomy results in better post-operative hearing outcome?. Eur Arch Otorhinolaryngol 276, 1907–1913 (2019). https://doi.org/10.1007/s00405-019-05415-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00405-019-05415-7