Abstract
Purpose
Obesity is pandemic. Yet, the success of most weight loss programmes is poor. The aim of the study was to assess illness perception in overweight/obese people and its impact on bio-functional age (BFA) reflecting physical, mental, emotional and social functioning.
Methods
75 overweight/obese subjects from the cross-sectional Bern Cohort Study 2014 were included. Participants followed a validated “bio-functional status” test battery amended by the validated questionnaires Patiententheoriefragebogen (illness perception) and AD-EVA (eating and movement behaviour). BFA was calculated in subjects aged ≥ 35 years (n = 56).
Results
(1) Mental occupation with the cause of overweight/obesity was generally moderate to high, but decreasing with age. (2) The predominant theories for being overweight/obese were health behaviour (58.7%) and psychosocial factors (33.3%). (3) Overweight/obese people with psychosocial theories on illness causes were more likely to have emotional or disinhibited eating patterns. (4) Cognitive control of eating patterns increased with age in both sexes. (5) Overweight/obese people were still bio-functionally younger than their chronological age (8.6 ± 0.8 year equivalents), although (6) quality of life was below average and (7) the risk for functional pro-aging was increased in those being especially mentally occupied with causes for overweight/obesity (r = 0.38, p < 0.001) and those having psychosocial (r = 0.32, p < 0.05) or naturalistic theories (r = 0.47, p > 0.001).
Conclusions
Consciously perceived psychosocial stress was found to be a main factor to disturb health and promote unhealthy cognitive patterns regulating eating and moving habits. Thus, successful weight reduction programmes should integrate subjective illness perceptions to not only improve the therapeutic outcome, but also functioning (BFA).
Similar content being viewed by others
Introduction
Overweight and obesity have become a major global medical and economic issue. On one hand, overweight and obesity are associated with an increased risk for developing non-communicable diseases (NCD) such as cardiovascular and metabolic diseases, cancer and depression [1,2,3,4,5]. On the other hand, there is some evidence for bio-functional pro-aging being positively correlated to body fat percentage [6].
Despite great efforts to combat this epidemic, so far, no single therapeutic method or preventive campaign has delivered convincing results. There is evidence from other medical conditions such as cardiovascular diseases that the patient’s perception of the disease has a crucial impact on the therapeutic outcome [7]. When being faced with a health threat such as the onset of certain symptoms or a new diagnosis, individuals will actively build cognitive models of the threat that will determine how they respond [7]. Accordingly, the disease may be considered as consequence of a certain way of living or as a starting point of a re-orientation [8] which may trigger specific treatment expectations. Knowing the patient’s illness perception is crucial for the treating physician as it influences treatment adherence and ultimately treatment outcome [8, 9]. Prior studies in overweight and obese patients have shown the importance of cognitive concepts for evaluation, counselling, prevention and treatment [10]. Accordingly, distinct cognitive patterns such as restraint eating, disinhibition, emotional eating, enjoyment, craving and addiction regulate eating and movement behaviour [11]. Yet, the perceived illness causes have never been assessed for overweight and obesity.
The Bern Cohort Study 2014 (BeCS-14) is a single-centre, cross-sectional, observational, non-interventional, non-randomized trial, which assessed a defined best and least health status across all non-paediatric and non-geriatric age stages (i.e. 18–65 years) [12]. The assessment tools applied were based on a complex Active and Healthy Aging (AHA) assessment model incorporating the International Classification of Functioning, Disability and Health (ICF) classification and concept [13, 14].
The aim of the present analysis was to (1) assess illness perceptions in the BeCS-14 subcohort of overweight and obese subjects, (2) analyse the association between illness perception and cognitive patterns that regulate eating and movement behaviour, and (3) evaluate if illness perceptions have an impact on bio-functional age in overweight and obese people.
Materials and methods
Study design
The study design has been described in detail before [12]. Briefly, BeCS-14 is a single-centre, cross-sectional, observational, non-interventional, non-randomized trial in German speaking men and women aged 18–65 years. Exclusion criteria were pregnancy, acute diseases (e.g. fever, acute pain syndrome), and illiteracy. Recruitment was performed between 2012-03-04 and 2014-07-04 at the Department of Obstetrics and Gynecology, Inselspital University Bern, Switzerland. All participants followed a standardised battery of assessments consisting of a personal and family history [the whole questionnaire addressing the personal and family history is available via the corresponding author (P. Stute)], bio-functional status (BFS), bio-functional age (BFA), and validated questionnaires for depression and anxiety (HADS) [15], health-related quality of life (SF-36) [16] and chronic stress (TICS) [17], respectively. Subsequently, participants were asked to take part in additional assessments (four non-randomized subgroups) of which one subgroup (“nutrition”) comprised overweight and obese [Body Mass Index (BMI) ≥ 25 kg/m2] participants only. They were asked to answer the validated questionnaires AD-EVA [18] addressing eating and movement behaviour as well as PATEF [19] addressing patient’s illness perception. The study protocol was approved by the Cantonal Ethics Committee Bern (Ref.-Nr. KEK-BE: 023112), and written informed consent was obtained from each participant.
Assessment procedures
Bio-functional status (BFS) and bio-functional age (BFA)
The BFS is a generic, age- and sex-specific test battery comprising holistic characteristics from physical (systolic and diastolic blood pressure, resting heart rate, pulse rate difference, performance time, performance pulse index, vital capacity FVC, body cell and fat mass, decayed/missing/filled teeth, vision, hearing acuity, psychomotor activity, test motivation, viseomotor coordination ability) mental–emotional (optical reaction time, pursuing reaction time, verbal reaction time, cognitive reaction time, cognitive switching capability, ability to concentrate, strategic thinking, orientation capability, memory performance, change over capability) and social areas (social resonance/stress exposition, self-control/stress disposition, social dominance, social power, physical well-being, emotional well-being, sense of coherence, social activity) (objectivity 0.96, reliability 0.93, females age validity: total age correlation 85.2%; total age commonality in the main factor 76.3%). It fits into a complex theoretical model incorporating the ICF and AHA concept [20,21,22], respectively, and is commercially available via Vital Services (http://www.microsoft.com/en-us/store/apps/biofunktionaler-status/9wzdncrd38qr). The single values of the BFS test battery were scaled and differentiated for chronological age (CA) and sex. Their summation makes up the so-called Bio-functional Age Index BFAI (BFAI = Σ (B-X/B-L)n/n). The BFAI is a relative measure compared to a reference population, out of which norm charts were developed. By definition, the reference population’s BFAI is identical with its CA. A BFAI of an individual may be transformed into BFA (years) by means of gerontologic aging tables. This BFA (years) relates to the mean value of a certain CA. The BFA is based on a sex-specific regression and factor analysis of functional age [20,21,22,23] (for transformation from BFS to BFA and gerontologic table see supplementary file 1).
Patiententheoriefragebogen (PATEF)
Patiententheoriefragebogen is a validated questionnaire addressing patient’s illness perception [3]. It contains 46 items covering five scales of which 18 are considered to be psychosocial (PS) and 18 naturalistic (NT), respectively [health behaviour (HB) scale (n = 10), PS external (n = 8) and internal (n = 10) scale, NT external (n = 8) and internal (n = 10) scale]. Each item is rated on a five-point rating scale (0 = certainly not to 4 = very likely). Based on norm charts, raw values are converted into age (</≥ 45 years) and sex-validated Stanine values [S values (1–9)] [24]. The overall score (OS) is a measure for the intensity of mental occupation with the illness cause (S < 4 corresponds to no thoughts or theory not covered by PATEF, respectively; S = 4–6 and no single scale with S > 6 corresponds to mental occupation with illness cause, but indecisive about the cause; S > 6 corresponds to high mental occupation; 1–3 single scales with S > 6 correspond to punched-out theory (already defined theory); 4–5 single scales with S ≥ 5 correspond to diffuse theory). The general single scales (GSS) is a measure for the main direction of perceived illness cause that is naturalistic (NT), psychosocial (PS) and health behaviour (HB, α = 0.93, r = 0.7), respectively, which can be grouped into six categories: (1) PS and NT with S = 1/2/3 correspond to rejection of PS and NT; (2) PS and NT with S = 4/5/6 correspond to PS and NT unremarkable, (3) PS and NT with S = 7/8/9 correspond to PS and NT are considered to be very likely, (4) PS with S > 6 and NT with S ≤ 6 correspond to clear focus on PS, (5) NT with S > 6 and PS with S ≤ 6 correspond to clear focus on NT, and (6) HB with S > 6 corresponds to HB and is considered to be very likely. The category external or internal attribution of illness cause represents the single-scale PSE (psychosocial external, α = 0.87, r = 0.79, PSE S > 6 corresponds to high risk for helplessness and depression), PSI (psychosocial internal, α = 0.93, r = 0.73, PSI S > 9 corresponds to very high indication of dissatisfaction, low self-esteem, even possible indication for needed psychotherapy), naturalistic external (NTE, α = 0.81, r = 0.74, NTE S > 6 corresponds to highly fatalistic tendency), naturalistic internal (NTI, α = 0.72, r = 0.74, NTI S > 6 corresponds to highly possible passivity). The internal validity of the PATEF is good; correlations between PSI&PSE r = 0.8, PSE&NTI r = 0.7, HB&PSI = 0.6 are highly significant. The external validity has been proofed in studies of myocardial infarction, headache and back pain [8, 24], where good accordance of the PATEF scales and therapy expectations, fear of relapses and therapy outcome have been found. So far, PATEF has not been validated in English. Additionally, we calculated correlations between PATEF and TICS [25] and HADS [15], respectively.
Interdisciplinary test system for the diagnostic and evaluation of adiposity and other with eating and movement behaviour influenceable diseases (AD-EVA)
AD-EVA is a validated questionnaire addressing eating and movement behaviour [10]. It contains 83 items covering nine scales of which five have been analysed for this study: (1) salutogenic behaviour scale (overall scale, 30 items, α = 0.91, r = 0.87) with subscales covering sports (7 items, α = 0.91, r = 0.84), the cognitive pattern “middle control” (11 items, α = 0.85, r = 0.86), enjoyment ability (6 items, α = 0.69, r = 0.89) and the ability of implementing suggestions (6 items, α = 0.71, r = 0.87), (2) pathogenic eating scale covering cognitive patterns as “cognitive control” (10 items, α = 0.94, r = 0.92), “disinhibition” (11 items, α = 0.9, r = 0.9) and “emotional eating” (8 items, α = 0.87, r = 0.89), (3) handling of food scale (11 items, α = 0.9, r = 0.85) covering the cognitive patterns of “craving” and “addiction”, (4) quality-of-life scale (5 items, α = 0.75, r = 0.81), and (5) the movement motivation scale (overall score 8 items, α = 0.71, r = 0.91) with the subscales “fun and satisfaction” (6 items, α = 0.7, r = 0.92) and “aesthetics” (2 items, α = 0.64, r = 0.9), respectively. Standardisation: raw values adjusted to a normal distribution produced comparable T values and percentage ranks on the basis of norm charts differentiating between age, sex, BMI and education [10]. T values have a range between 20 and 80, percentage ranks 0–100. T values < 30/> 70 are considered extreme, 30 to < 40 as under average, 40 to < 60 as average and 60 to < 70 as over average [10]. The equivalent percentage ranks allow a more concise interpretation of the T values [10].
Statistics
The statistical analysis was performed with SPSS version 22. The descriptive statistics contained the calculation of the median, mean, range (min–max), standard deviation and for ordinal parameters the percentages. Correlation statistics was done by Pearson’s bivariate test statistics with a level of significance of 5% (two-sided) or 2.5% (one-sided). Missing values of the BFS were replaced by average values of the reference population [12]. No missing values were found in the AD-EVA and PATEF test batteries.
Results
Characteristics of the cohort (Table 1)
Age, social and job status
In total, 75 subjects (77.3% female, 22.7% male) of the BeCS-14 cohort were overweight or obese, respectively, and therefore, further analysed by the questionnaires PATEF and AD-EVA (see Table 1). Mean age was 46.3 ± 12.6 years, mean BMI 29.32 ± 3.64 kg/m2 and mean fat mass 34.1 ± 9.4%, respectively. 62.7% of participants were overweight (BMI 25–29.9) and 35.9% obese [29.3% obesity I (BMI 30–34.9), 5.3% obesity II (BMI 35–39.9) and 1.3% obesity III (BMI ≥ 40)]. Of the 75 subjects included, 17.6% of men and 41.4% of women were obese. Two-thirds of recruited subjects were living in a partnership (61.3%). 41.3% of participants were childless, whereas one in three had at least two children (37.4%). The educational level differed strongly, as 28.0% were academic, 29.3% had a professional diploma or equivalent, 21.3% an apprenticeship, and 8% obligatory school only. Most participants (44%) worked in the social field, and one quarter (25.3%) in economy, administration or service, respectively. Executive positions were held by 26.7%, while the majority (56%) worked as employees. Job occupation was at least 50% in the majority (80%), and at least 90% in almost half of participants (49.3%). The monthly gross income was less than 5000 Swiss Francs for 45.3%. About half (48%) of participants reported going to work despite being sick, reflected in the low numbers of sick days.
Life style
About one quarter (25.3%) reported regular alcohol consumption at least twice a week (22.4% of women, 58.8% of men). 26.7% had at least one drink per day. In contrast, the majority of participants were never-smokers (50.7%) or former smokers (32%; 29.3% of women, 47.1% of men), respectively. Physical activity (till sweating) varied strongly ranging from almost no workout (33.3%; 36.2% of women, 29.4% of men) to high activity levels (> 2/week) in 17.3%. 82.3% slept 6–7 h a night. Sleep quality during the last 4 weeks was good in 61 participants (69.3%).
Personal and family history
The prevalence of being disease free was 50.7% (n = 38). Life-threatening events were reported by five participants (myocardial infarction n = 0; stroke n = 1; pulmonary embolism n = 4). The prevalence of a positive family history varied and was 42.7% for cancer, 46.7% for cardiovascular disease (myocardial infarction 28%, stroke 25.3%, pulmonary embolism 13.3%), 44% metabolic disorder (dyslipidemia 29.3%, diabetes mellitus 24%) and osteoporosis (8%).
Medications
In the BeCS-14 cohort, 52 participants reported use of any kind of medication (n = 75 reports). The major medication groups were dietary supplements (n = 12), sexual steroids for contraception (n = 7) or menopausal hormone therapy (n = 11), psychotropic medication (n = 14), analgetics (n = 10) and antihypertensives (n = 11).
Illness perception (PATEF, Table 2)
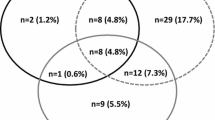
The prevalence of the various degrees of mental occupation with overweight/obesity and the preferred underlying patient’s theory on the causes of overweight/obesity is presented in Table 2. The median S values were 6 for OS, NT internal and PS external, 5 for NT and NT external, and 7 for HB, PS and PS internal, respectively. Intensity of mental occupation with the cause of overweight/obesity was high (S > 6) in 37.4%, moderate in 57.3% (S4–6) and low (S < 4) in 5.3% of participants. The focus (S > 6) of mental occupation with the underlying causes for overweight/obesity was (in descending frequency) HB (58.7%), PS internal (56%), PS (50.7%), PS external (34.7%), NT internal (24%), NT (18.6%), and NT external (12%), respectively. This finding indicates that many overweight and obese subjects not only consider their own health behaviour as a main cause of overweight/obesity, but also hold their inner personality, e.g. low self-esteem (PS internal), other people, e.g. family members (PS external), their disposition, e.g. genes and hormones (NT internal), or exposition, e.g. pollution (NT external), responsible for their illness. 41.3% of participants had a very clear idea of the underlying cause of overweight/obesity (punched-out theory) while 18.7% had more diffuse theories about the illness cause. Based on the individual percentage HB/PS/NT combination the main direction of perceived illness cause (HB, PS, NT) may be further categorized into six subgroups: 1) mainly HB 58.7% (HB S > 6), 2) clear focus on PS theories 33.3% (high PS with S > 6 and low NT with S ≤ 6), 3) clear focus on NT theories 1.3% (high NT with S > 6 and low PS with S ≤ 6), 4) simultaneous focus on PS and NT theories 17.3% (PS and NT with S = 7/8/9), 5) neutrality against PS and NT theories 33.3% (PS and NT with S = 4/5/6) and 6) rejection of PS and NT theories 2.67% (PS and NT with S = 1/2/3). When adjusting PATEF scores for BMI and fat mass, results did not change. The degree of mental occupation (OS) with the causes of overweight/obesity decreased with aging (r = − 0.26; p < 0.05). In the age group 20–34 years, 61.1% were highly mentally occupied with illness causes (OS S > 6), which was almost cut in half in the age group of 35–75 years (29.8%). When differentiating for sex, men (76.5%) were significantly more often convinced than women (50%) that their inner personality was highly responsible for overweight/obesity (PS internal S > 6 and age: r = 0.26; p < 0.05). Correlations were not affected when adjusting for BMI categories (distinction overweight/obesity). The intensity of mental occupation with the illness cause (PATEF: OS) correlated significantly positively with several subscales of HADS (anxiety, depression) and TICS (chronic worrying, social isolation, chronic stress, excessive demand, work dissatisfaction) (supplementary file 2).
Eating and movement behaviour (AD-EVA, Table 3)
The prevalence of various eating and movement behaviour patterns is presented in Table 3. Most patterns were within the normal range of the reference cohort (T values 40–< 60). The only exceptions were movement motivation overall (T value = 38), movement motivation fun and satisfaction (T value = 36) and quality of life (T value = 30) which were below average (T values 30–< 40). There were no above average (T values 60–< 70) or extreme patterns (T values < 30/> 70), respectively. The prevalence of at least one (out of three) pathogenic eating behaviour patterns was 45.3% (n = 34). In a next step, the impact of age and sex on eating and movement behaviour was assessed. As AD-EVA norm values are already adjusted for weight, further adjustment of the data for BMI is not indicated. Within the scale “salutogenic eating behaviour”, only the sub-category “suggestion implementing” (e.g. implementing eating and movement recommendations into daily life) showed a sex, but no age effect (r = − 0.42; p < 0.001). The mean T value was within the normal range for males (47.4 ± 7.4) and females (54.8 ± 6.8). However, the prevalence of men in the below average group (T value < 40) was higher (11.7%) than that of women (0%) while the opposite was true for the above average group (T value ≥ 60; men 0% and women 17.5%). Within the scale “pathogenic eating behaviour”, sex or age, respectively, had an impact on the sub-categories “emotional eating” (r = − 0.31; p < 0.001) and “cognitive control” (r = 0.31; p < 0.001). The mean T value for “emotional eating” (e.g. eating due to internal stimuli such as stress, depression) was within the normal range for males (48.7 ± 10.0) and females (55.6 ± 8.6). However, there were more women (32.8%) than men (11.8%) in the above average group (T value ≥ 60). The mean T value for “cognitive control” [high mental occupation with “not eating”, e.g. eating is only “allowed” at certain time points during the day which may lead to the opposite reaction (disinhibition) with eating attacks] was within the normal range for subjects aged 20–34 years (49.9 ± 8.7) and those aged 35–75 years (53.5 ± 7.9). However, older participants (23.2%) were more likely to be within the above average group (T value ≥ 60) than younger (15.8%) while the opposite was true for the below average group (T value < 40; 20–34 years: 10.5% and 35–75 years: 3.6%). Within the scale “movement motivation” only the sub-category “fun and satisfaction” (e.g. internal motivation for movement such as having fun, meeting friends) was affected by sex (r = − 0.31; p < 0.001), but not age. Interestingly, mean T values were below average (T value < 40) for both, men (32.8 ± 5.8) and women (39.3 ± 9.2). Moreover, even more men (94.1%) than women (67.2%) were in the below-average group. Handling of food and quality of life were not affected by age and sex.
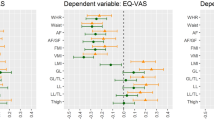
Impact of illness perception (PATEF) on eating and movement behaviour (AD-EVA) and vice versa
Correlation analysis of PATEF and AD-EVA categories is presented in Table 4. Only eating, but not movement behaviour was associated with certain illness perceptions, especially psychosocial theories. Salutogenic eating behaviour (sub-categories overall, middle control, sports) was significantly negatively correlated with the psychosocial scale (sub-categories overall, external, internal). Thus, overweight and obese people with prevalent feelings of helplessness, depression and dissatisfaction were less likely to sensibly manage their eating habit to maintain and support well-being and health. In other words, overweight and obese people with salutogenic eating behaviour were less likely to blame psychosocial factors and their health behaviour as being the cause for overweight/obesity. Pathogenic eating behaviour was significantly positively correlated with the psychosocial and health behaviour scale. Thus, overweight and obese people with low self-esteem were more likely to eat without control and due to emotions. To put it in another way, overweight and obese people with emotional eating patterns were more likely to report behavioural or psychosocial reasons for being overweight/obese. Similarly, individuals being easily disinhibited by food pictures or clues were more likely to have a behavioural or psychosocial internal illness perception. The handling of food significantly correlated with the psychosocial scale (sub-categories overall, external, internal) indicating that a person with high craving and addiction scores was more likely to present with psychosocial illness perception.
Bio-functional age (BFA)
For bio-functional age (BFA) calculation, age 35 is an accepted cut-off value [20]. In our cohort, 56 participants (75%) were above age 35. In this group, mean BFA was 44.0 ± 7.2 years and mean CA 52.9 ± 6.1 years (see Table 5). The mean difference between CA and BFA was 8.6 ± 0.8 years equivalents (which matches the findings of the complete BeCS-14 [12]). There was a significant correlation between BFA and CA (r = 0.34, p < 0.05) indicating a higher BFA was associated with a higher CA. Furthermore, a higher BFA was associated with functional pro-aging as there was a significant correlation between BFA and the CA-BFA difference (r = 0.642, p < 0.001). BFA also significantly correlated with sex (r = 0.33, p < 0.05), indicating that males were more likely to be functionally older. There was no association between BFA and BMI or fat mass, respectively.
Impact of illness perception (PATEF) and eating and movement behaviour (AD-EVA) on bio-functional age (BFA)
All theories of causes for overweight/obesity, but HB were significantly positively correlated with BFA and the CA-BFA difference (Table 5) indicating that bio-functionally younger individuals was less mentally occupied with the reasons for being overweight/obese. In other words, being mentally occupied with the causes of overweight/obesity was associated with pro-aging, that is being bio-functionally older. In particular, that was true for subjects with low self-esteem, depression, etc. (psychosocial theory), and those with fatalistic tendency or passive features (naturalistic theory). Interestingly, eating and movement behaviour (AD-EVA scores) was not associated with BFA.
Discussion
To our knowledge, this is the first study to investigate illness perception in overweight and obese people and its impact on bio-functional age. We found that (1) in overweight/obese people, mental occupation with the cause of overweight/obesity was generally moderate to high, but decreasing with age; (2) the predominant theories for being overweight/obese were health behaviour (58.7%) and psychosocial factors (33.3%); (3) overweight/obese people (especially women) with psychosocial theories on illness causes (e.g., depression, dissatisfaction, family and friends) were more likely to have emotional or disinhibited eating patterns; (4) cognitive control of eating patterns increased with age in both sexes; (5) in overweight/obese people movement motivation was decreased and less likely associated with fun; (6) overweight/obese people were still bio-functionally younger than their CA (8.6 ± 0.8 year equivalents), although (7) quality of life was below average and (8) the probability of functional pro-aging was increased in those being especially mentally occupied with the causes for overweight/obesity and in subjects with low self-esteem, depression, etc. (psychosocial theories), and those with a fatalistic tendency or passive features (naturalistic theories). However, (9) overweight/obese women seem to be willing to implement recommendations on eating and movement into their daily life.
Distinct cognitive patterns have been shown to regulate eating and movement behaviour [11], some of which are assessed by the AD-EVA, e.g. “restraint eating” [26,27,28], “disinhibition” [29], “emotional eating”, “enjoyment”, “craving” and “addiction” [10], respectively. However, despite the epidemic burden of overweight and obesity and proven positive impact of professional support for changing illness perceptions on disease outcomes [30,31,32], patients’ theory on the causes of overweight/obesity has not been studied before. The pre-condition for a successful professional intervention in overweight/obese seems to be good as the awareness of and mental occupation with overweight/obesity was generally high and the perceived quality of life, below average. Interestingly, as psychosocial factors (PATEF subscales PS, PSI and PSE) did not correlate with the AD-EVA subscale “quality of life”, overweight/obesity itself rather than psychosocial issues seem to negatively affect quality of life. However, although health behaviour was considered as being the main reason for overweight/obesity, psychosocial and combined psychosocial and naturalistic causes were considered as being the second and third most important causes for overweight/obesity, respectively. Thus, weight loss programmes focusing on calories and exercise are unlikely to be successful in people that do not believe that their health behaviour is the main cause of overweight/obesity. As people with psychosocial illness perceptions tend to have low self-esteem, depression, inner restlessness and feelings of helplessness, psychotherapy should be part of their weight loss programme. Indeed, cognitive behavioural therapy in overweight and obesity has been shown to be successful manifold [33, 34]. However, due to our results, we believe that some further understanding of how illness perceptions on overweight/obesity affect cognitive patterns that regulate eating and movement behaviour and vice versa will be helpful for successful psychosocial interventions. Pathogenic eating behaviour such as emotional eating was predominantly found in females (32.8% of the women). Subjects having a tendency for being overwhelmed by emotions more likely consider their behaviour, e.g. excessively eating, and/or psychological stress as crucial for their overweight/obesity, respectively, which then reinforces overwhelming (negative) emotions and disinhibition implying that food clues (advertisement, smell) cannot be resisted—a vicious circle. Similarly, salutogenic eating behaviour also depended on psychosocial illness perception. The higher the psychosocial stress level of an individual, the lower was his/her ability to handle eating and moving behaviour in a salutogenic way, even if the subject was fully aware of this association. Similarly, middle control was low in overweight/obese subjects with behavioural and psychosocial illness perceptions, reflecting a less flexible, but more rigid cognitive control that is prone to eating attacks. A high cognitive control can lead to ignoring internal/external stimuli (such as low blood sugar level) which might end up in the opposite behaviour such as uncontrolled eating attacks [10]. Interestingly, cognitive control that is a restraint eating pattern increased with age. We suggest that it takes time to build up cognitive patterns such as restraint eating. Most weight loss programmes include recommendations on exercise. However, overweight/obese people might have difficulties to translate those “helpful” recommendations into daily life as we found that movement motivation was below average in our cohort. Specifically, exercising was not associated with fun and satisfaction, but possibly more with duty. This was particularly true for males. Men also were less approachable for eating suggestions, which may go along with lower age-dependent nutrition knowledge [35, 36].
Keeping in mind, that overweight/obesity was associated with below-than-average quality of life, we wanted to explore if overweight/obesity had an impact on an individual’s functioning, assessed by his/her bio-functional age. Indeed, subjects being highly mentally occupied with or believing in psychosocial and naturalistic causes for overweight/obesity were more likely to be functionally older than those with a behavioural illness perception. One might argue that subjects with higher BFA were also chronologically older increasing the risk of having “real” medical conditions that might support their naturalistic (internal) perception. However, in our cohort, the prevalence of severe medical conditions was low. Thus, we believe that “medically less compelling” reasons such as hormonal dysbalances might be preferentially blamed for being overweight/obesity. Similarly, individuals with higher BFA were more likely to have psychosocial perceptions of overweight/obesity. Indeed, BFA calculation is based on the bio-functional status, comprising 45 items of physical, mental, cognitive, emotional and social functions [12]. Thus, from the patient’s perspective, emotional and social strengths and resources assessed by the BFS/BFA were also perceived as being crucial for being/becoming overweight/obese, assessed by the PATEF. On the other hand, there were no correlations between BFA and AD-EVA indicating that bio-functional age(ing) was not affected by cognitive eating and movement patterns.
Our study has some limitations. The sample size was quite small and only 75% were aged above 35, and thus applicable for BFA calculation and there were few exclusion criteria (e.g. psychiatric disease was not a reason for exclusion). Sex was not equally distributed (77.3% women). As the PATEF is only applicable for diseases, we did not ask our BeCS-14 participants with normal weight to fill it in. Thus, we were not able to compare our results in overweight/obese subjects to those with normal weight. We could find some correlations between PATEF, AD-EVA and BFA. However, we did not find causal associations, but could only speculate on them. The advantage of our study is that illness perceptions have been analysed for the first time in overweight/obese people supporting the importance of cognitive interventions in weight loss programmes not only for weight reduction, but also for bio-functional age. Specifically, we could show that cognitive interventions should be even tailored to age and sex.
Conclusion
Overweight and obesity are risk factors for developing non-communicable diseases. However, despite the worldwide effort to reduce its prevalence, the numbers are continuously increasing. We showed that overweight/obese people were highly mentally occupied with the causes of overweight/obesity probably reducing their quality of life and increasing the risk of functional pro-aging. The predominant theories for being overweight/obese were health behaviour and psychosocial factors. Consciously perceived psychosocial stress was found to be a main factor to disturb health and promote unhealthy cognitive patterns regulating eating and moving habits. We are convinced that with integrating illness perception on overweight/obesity into weight loss programmes, chances for long-term success would increase. The physician/coach could then allocate an overweight/obese patient to an individually appropriate weight reduction programme—or to none at all if, e.g. illness perception was primarily naturalistic.
Abbreviations
- AD-EVA:
-
Interdisciplinary test system for the diagnostic and evaluation of adiposity and other with eating and movement behaviour influenceable diseases
- AHA:
-
Active and healthy aging
- BeCS-14:
-
Bern Cohort Study 2014
- BFA:
-
Bio-functional age
- BFS:
-
Bio-functional status
- BMI:
-
Body Mass Index
- CA:
-
Calendaric age
- CA-BFA:
-
Difference between calendaric and bio-functional age
- GSS:
-
General Single scale
- HADS:
-
Hospital Anxiety and Depression Scale
- HB:
-
Health Behavioural scale
- ICF:
-
International Classification of Functioning, Disability and Health
- NCD:
-
Non-communicable diseases
- NT:
-
Naturalistic scale
- NTE:
-
Naturalistic External scale
- NTI:
-
Naturalistic Internal scale
- OS:
-
Overall score
- PATEF:
-
Patiententheoriefragebogen
- PS:
-
Psychosocial scale
- PSE:
-
Psychosocial External scale
- PSI:
-
Psychosocial Internal scale
- SF-36:
-
Short Form Gesundheitsfragebogen
- TICS:
-
Trier Inventar zum chronischen Stress
References
Abate N, Chandalia M (2017) Risk of obesity-related cardiometabolic complications in special populations: a crisis in Asians. Gastroenterology 152(7):1647–1655
Arnold M, Jiang L, Stefanick M, Johnson K, Lane D, LeBlanc E, Prentice R, Rohan T, Snively B, Vitolins M, Zaslavsky O, Soerjomataram I, Anton-Culver H (2015) Duration of adulthood overweight, obesity, and caner risk in the women’s health initiative: a longitudinal study from the United States. PLoS Med 13(8):e1002081
Patel S, Ali M, Alam D, Yan L, Levitt N, Bernabe-Ortiz A, Checkley W, Wu Y, Irazola V, Gutierrez L, Rubinstein A, Shivashankar R, Li X, Miranda J, Chowdhury M, Siddiquee A, Gaziano T, Kadir M, Prabhakaran D (2016) Obesity and its relation with diabetes and hypertension. A cross-sectional study across 4 geographical regions. Glob Heart 11(1):71–79
Francoeur R (2016) Symptom profiles os subsyndromal depression in disease clusters of diabetes, excess weight, and progressive cerebrovascular conditions: a promising new type of finding from a reliable innovation to estimate exhaustively specified multiple indicators-multiple causes (MIMC) models. Diabetes Metab Syndr Obes 9:391–416
Bliddal M, Pottegard A, Kirkegaard H, Olsen J, Sorensen T, Nohr E (2016) Depressive symptoms in women’s midlife in relation to their body weight before, during and after childbearing years. Obes Sci Pract 2:415–425
Freude G, Jakob O, Martus P, Rose U, Seibt R (2010) Predictors of the discrepancy between calendar and biological age. Occup Med 60(1):21–28
Petrie KJ, Weinman J (2006) Why illness perceptions matter. Clin Med 6(6):536–539
Zenz H, Bischoff C, Hrabal V (1996) Patiententheoriefragebogen (PATEF). Hogrefe Verlag für Psychologie, Göttingen
Leventhal H, Nerenz DR, Steele DJ (1984) Illness representations and coping with health threats. Erlbaum, Hillsdale
Ardelt-Gattinger E, Meindl M (2010) AD-EVA. Interdisziplinäres Testsystem zur Diagnostik und Evaluation bei Adipositas und anderen durch Ess- und Bewegungsverhalten beeinflussbaren Krankheiten (Modul 1). Verlag Hans Huber, Hoegrefe AG, Bern
Ardelt-Gattinger E, Ring-Dimitriou S, Hofmann J, Paulmichl K, Zsoldos F, Weghuber D (2015) Geschlechtsunterschiede bei psychologischen, ernährungs- und sportwissenschaftlichen Einflussfaktoren auf Adipositas/Übergewicht bei Kindern und Jugendlichen in Österreich. Wien Med Wochenschr 166:111–116
Stute P, Bitterlich N, Bousquet J, Meissner F, von Wolf M, Poethig D (2017) Measuring Active and Healthy Ageing: applying a complex interdisciplinary assessment model incorporating ICF. J Nutr Health Aging 9:1002–1009
Viol M (2011) Bio-psychosocial aging—positioning of the vitality concept in the ICF. Bewegungstherapie und Gesundheitsreport 2(27):74–79
Grotkamp S, Cibis W, Nuechtern E, von Mittelstaedt G, Seger W (2012) Personal factors in the international classification of functioning, disability and health: prospective evidence. Aust J Rehabil Couns 18(1):1–24
Hamilton M (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23:56–62
Bullinger M, Kirchberger I, Ware J (1995) Der deutsche SF-36 Health Survey. Übersetzung und psychometrische Testung eines krankheitsübergreifenden Instrumentes zur Erfassung der gesundheitsbezogenen Lebensqualität. Zeitschrift fuer Gesundheitswissenschaften 1:21–36
Schulz P, Schlotz W, Becker P (2004) Trierer Inventar zum chronischen Stress (TICS). Hogrefe, Göttingen
Ardelt-Gattinger E, Meindl M (2010) AD-EVA. Interdisziplinäres Testsystem zur Diagnostik und Evaluation bei Adipositas und anderen durch Ess- und Bewegungsverhalten beeinflussbaren Krankheiten. Huber, Bern
Zenz H, Bischoff C, Hrabal V (1996) Patiententheorienfragebogen (PATEF). Handanweisung. Hogrefe, Göttingen
Poethig D (1984) Experimental development of a clinical diagnostic model objectifying bio-functional age(ing) of human beings. Habilitation thesis. German National Library, Leipzig
Ries W, Poethig D (1984) Chronological and biofunctional age—a new method to measure healthy aging. Exp Gerontol 19(3):211–216
Dean W (1988) Biological aging measurement: clinical applications. The German test bettery. University of Leipzig, The Center for Bio Gerontology Los Angeles, pp 175–187
Meissner-Poethig D, Michalak U (1997) Vitalität und ärztliche Intervention. Hippokrates Verlag, Stuttgart
Berth H, Balck F (2003) Psychologische Tests für Mediziner. Springer, Berlin
Schulz P, Schlotz W, Becker P (2004) Trierer Inventar zum chronischen Stress (TICS). Hogrefe, Göttingen
Hofmann J, Ardelt-Gattinger E, Paulmichl K, Weghuber D, Blechert J (2015) Dietary restraint and impulsivity modulate neural responses to food in adolescents with obesity and healthy adolescents. Obesity 23(11):2183–2189
Hendrikse JJ, Cachiar L, Kothe EJ, McPhie S, Skouteris H, Hayden MJ (2015) Attentional biases for food cues in overweight and individuals with obesity: a systematic review of the literature. Obes Rev 16(5):424–432
Price M, Higgs S, Lee M (2015) Self-reported eating traits: underlying components of food responsivity and dietary restriction are positively related to BMI. Appetite 95:203–210
French SA, Mitchell NR, Finlayson G, Blundell JE, Jeffery RW (2014) Questionnaire and laboratory measures of eating behaviour. Associations with energy intake and BMI in a community sample of working adults. Appetite 72:50–58
Princip M, Scholz M, Meister-Langraf R, Barth J, Schnyder U, Znoj H, Schmid J-P, Thayer J, von Känel R (2016) Can illness perceptions predict lower heart rate variability following acute myocardial infarction? Front Psychol 7:1801
Foxwell R, Morley C, Frizelle D (2013) Illness perception, mood and quality of life: a systematic review of coronary heart disease patients. J Psychosom Res 75(3):211–222
Tiemensma J, Gaab E, Voorhaar M, Asijee G, Kaptein AA (2016) Illness perception and coping determine quality of life in COPD patients. Int J COPD 11:2001–2007
Rodriguez-Hernandez H, Morales-Amaya U, Rosales-Valdez R, Rivera-Hinojosa F, Rodriguez-Moran M, Guerrero-Romero F (2009) Adding cognitive behavioural treatment to either low-carbohydrate or low-fat diets: differential short-term effects. Br J Nutr 102:1847–1853
Gade H, Hjelmesaeth J, Rosenvinge J, Friborg O (2014) Effectiveness of a cognitive behavioral therapy for dysfunctional eating among patients admitted for bariatric surgery: a randomized controlled trial. J Obes 2014:6
Rurik I (2006) Nutritional differences between elderly men and women. Primary care evaluation in Hungary. Ann Nutr Metab 50(1):45–50
Asakura K, Todoriki H, Sasaki S (2017) Relationship between nutrition knowledge and dietary intake among primary school children in Japan: combined effects of children’s and their guard’s knowledge. J Epidemiol 27:483–491
Acknowledgements
The authors would like to thank J. D. Wanner and D. Gafner, study nurses, for their administrative assistance during the study. Also, the authors are thankful to the medical students N. Ammann and M. Moser for conducting the assessments.
Funding
The study was supported by an unrestricted Grant by Merck Sharp & Dohme Corp. and Burgergemeinde Bern.
Author information
Authors and Affiliations
Contributions
Contributions to the manuscript are as follows: LM: statistical analysis with support of Dr. Bitterlich, writing the manuscript. NB: statistics. MW: discussion of results, advise on manuscript. FM: discussion of results, advise on manuscript. DP: discussion of results. PS: principle investigator, responsible for study idea, design, finances, supervision of doctoral student and finalizing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
L. Mathieu, P. Stute, M. von Wolff and N. Bitterlich declare to have no conflict of interest in context of this manuscript. F. Meissner is the managing director of Vital Services and D. Poethig is member of the scientific board of Vital Services, which provides the technology for BFS/BFA measuring. F. Meissner has no involvements that might raise the question of bias in the work reported or in the conclusions, implications, or opinions stated.
Electronic supplementary material
Below is the link to the electronic supplementary material.
404_2018_4827_MOESM2_ESM.pdf
Supplementary file 2: Supplementary table: Correlations of PATEF with HADS and TICS; only statistically significant correlations are shown (*p < 0.05/**p < 0.001) (PDF 66 kb)
Rights and permissions
About this article
Cite this article
Mathieu, L., Bitterlich, N., Meissner, F. et al. Illness perception in overweight and obesity and impact on bio-functional age. Arch Gynecol Obstet 298, 415–426 (2018). https://doi.org/10.1007/s00404-018-4827-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-018-4827-0