Abstract
Purpose
The purpose was to investigate, in a large cohort, how hysterectomy technique influences the incidence of subsequent pelvic organ prolapse (POP) repair among women hysterectomized for benign conditions.
Methods
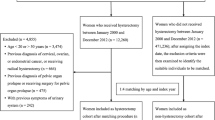
From the Danish National Patient Registry, we collected data on all hysterectomies on benign indications, and all POP operations performed in Denmark from January 1, 1977 to June 10, 2016. We excluded patients with prior POP repair. We analyzed the incidence of POP surgery by cumulative incidence curves and hazard ratio (HR) for women with and without POP diagnoses or concomitant POP repair at hysterectomy.
Results
In all, 178,282 women underwent hysterectomy in the study period and were included in the cohort. When examining the crude HR for the risk of POP repair after hysterectomy, vaginal hysterectomy (VH) had a threefold rise in HR compared to total abdominal hysterectomy (TAH). When restricting the analyses to women without POP at time of hysterectomy, the HR for VH decreased to 1.25. The same tendency was noticed when stratifying by compartment. In the subgroup of women without POP at hysterectomy, we found that supravaginal abdominal hysterectomy had a small increase in risk compared to TAH. Laparoscopic hysterectomy had the same risk of POP as TAH.
Conclusions
Overall, we found only small differences in risk of POP repair between the different hysterectomy techniques after restricting the analyses to women without POP at hysterectomy.


Similar content being viewed by others
References
Løwenstein E, Ottesen B, Gimbel H (2015) Incidence and lifetime risk of pelvic organ prolapse surgery in Denmark from 1977 to 2009. Int Urogynecol J 26:49–55. doi:10.1007/s00192-014-2413-y
Lykke R, Blaakær J, Ottesen B, Gimbel H (2013) Hysterectomy in Denmark 1977–2011: changes in rate, indications, and hospitalization. Eur J Obstet Gynecol Reprod Biol. doi:10.1016/j.ejogrb.2013.09.011
Chow D, Rodriguez LV (2013) Epidemiology and prevalence of pelvic organ prolapse. Curr Opin Urol 23:293–298. doi:10.1097/MOU.0b013e3283619ed0
Altman D, Falconer C, Cnattingius S, Granath F (2008) Pelvic organ prolapse surgery following hysterectomy on benign indications. Am J Obstet Gynecol 198:572.e1–572.e6. doi:10.1016/j.ajog.2008.01.012
Shalom DF, Lin SN, O’Shaughnessy D et al (2012) Effect of prior hysterectomy on the anterior and posterior vaginal compartments of women presenting with pelvic organ prolapse. Int J Gynecol Obstet 119:274–276. doi:10.1016/j.ijgo.2012.06.014
Blandon RE, Bharucha AE, Melton LJ 3rd et al (2007) Incidence of pelvic floor repair after hysterectomy: a population-based cohort study. Am J Obstet Gynecol 197:664.e1–664.e7. doi:10.1016/j.ajog.2007.08.064
Dallenbach P, Kaelin-Gambirasio I, Dubuisson JB, Boulvain M (2007) Risk factors for pelvic organ prolapse repair after hysterectomy. Obstet Gynecol 110:625–632. doi:10.1097/01.AOG.0000278567.37925.4e
Dallenbach P, Kaelin-Gambirasio I, Jacob S et al (2008) Incidence rate and risk factors for vaginal vault prolapse repair after hysterectomy. Int Urogynecol J 19:1623–1629. doi:10.1007/s00192-008-0718-4
Andersen LL, Alling Møller LM, Gimbel HM (2015) Objective comparison of subtotal vs. total abdominal hysterectomy regarding pelvic organ prolapse and urinary incontinence: a randomized controlled trial with 14-year follow-up. Eur J Obstet Gynecol Reprod Biol 193:40–45. doi:10.1016/j.ejogrb.2015.06.033
Persson P, Brynhildsen J, Kjolhede P, HMSG Sweden in S-E (2013) Pelvic organ prolapse after subtotal and total hysterectomy: a long-term follow-up of an open randomised controlled multicentre study. BJOG 120:1556–1565. doi:10.1111/1471-0528.12399
Lidegaard O, Hammerum MS (2002) The National Patient Registry as a tool for continuous production and quality control. Ugeskr Laeger 164:4420–4423
Ottesen M (2009) Validity of the registration and reporting of vaginal prolapse surgery. Ugeskr Laeger 171:404–408
Lykke R, Blaakær J, Ottesen B, Gimbel H (2015) Pelvic organ prolapse (POP) surgery among Danish women hysterectomized for benign conditions: age at hysterectomy, age at subsequent POP operation, and risk of POP after hysterectomy. Int Urogynecol J 26:527–532. doi:10.1007/s00192-014-2490-y
Lykke R, Blaakær J, Ottesen B, Gimbel H (2016) Age at hysterectomy as a predictor for subsequent pelvic organ prolapse repair. Int Urogynecol J 27:751–755. doi:10.1007/s00192-015-2881-8
Author information
Authors and Affiliations
Contributions
RL: project development, data collection, data analysis, and manuscript writing. EL: data collection and manuscript editing. JB: project development and manuscript editing. HG: project development, data collection, data analysis, and manuscript writing.
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
404_2017_4470_MOESM1_ESM.eps
Figure 3: Plot showing the adjusted cumulative incidence of pelvic organ prolapse (POP) repair in the anterior compartment for each of the four hysterectomy types for women without POP at hysterectomy (EPS 1100 kb)
404_2017_4470_MOESM2_ESM.eps
Figure 4: Plot showing the adjusted cumulative incidence of pelvic organ prolapse (POP) repair in the apical compartment for each of the four hysterectomy types for women without POP at hysterectomy (EPS 1545 kb)
404_2017_4470_MOESM3_ESM.eps
Figure 5: Plot showing the adjusted cumulative incidence of pelvic organ prolapse (POP) repair in the posterior compartment for each of the four hysterectomy types for women without POP at hysterectomy (EPS 1100 kb)
Rights and permissions
About this article
Cite this article
Lykke, R., Løwenstein, E., Blaakær, J. et al. Hysterectomy technique and risk of pelvic organ prolapse repair: a Danish nationwide cohort study. Arch Gynecol Obstet 296, 527–531 (2017). https://doi.org/10.1007/s00404-017-4470-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00404-017-4470-1