Abstract
Objective
To comprehensively compare the perioperative data and clinical outcomes of natural pressure drainage (NAPD) and negative pressure drainage (NEPD) following transforaminal lumbar interbody fusion (TLIF) for the treatment of lumbar degeneration disease.
Methods
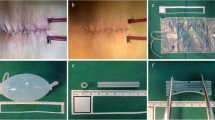
Between January 2021 and December 2021, 203 patients in our hospital who underwent single- or two-segment TLIF were assigned to the NAPD group (112 patients) or the NEPD group (91 patients) based on different postoperative drainage methods. Between the two groups, comparisons were made regarding the demographics, intraoperative and postoperative data, patient-reported outcomes, and complications.
Results
The NAPD group experienced less overall drainage and fewer postoperative drainage days (157.89 vs. 318.49 ml/249.54 vs. 589.43 ml, 2.00 vs. 2.67 days/2.04 vs. 2.74 days, P < 0.001) than the NEPD group. The NAPD group has a higher rate of overall hidden blood loss (HBL) than the NEPD group (63.98% vs. 51.90%/65.80% vs. 48.11%, P < 0.001); HBL, however, did not significantly differ between the two groups (P > 0.05). In two-segment surgery, the postoperative hemoglobin (HGB) levels were higher in the NAPD group (99.67 vs. 92.69 g/L, P < 0.05), but there was no difference in single-segment surgery (P > 0.05). Regardless of whether single- or two-segment surgery was performed, the NAPD group had a lower HGB level loss (18.81% vs. 21.63%/26.35% vs. 32.08%, P < 0.05). There was no discernible difference between the two groups in the visual analog scale (VAS) scores for symptomatic epidural hematoma, postoperative body temperature, low back and leg pain, or incision infection (P > 0.05).
Conclusion
NAPD did not increase postoperative complications but did significantly reduce postoperative drainage volume and the risk of anemia. We show that, when compared to NEPD, NAPD may be a better option for patients following TLIF.



Similar content being viewed by others
References
Zhou W, Li LJ, Tan J (2010) Treatment of degenerative lumbar spondylolisthesis by transforaminal lumbar interbody fusion with microendoscopic surgery. Zhongguo Gu Shang 23(4):251–253
Griessenauer CJ, Raborn J, Foreman P, Shoja MM, Loukas M, Tubbs RS (2015) Venous drainage of the spine and spinal cord: a comprehensive review of its history, embryology, anatomy, physiology, and pathology. Clin Anat 28(1):75–87. https://doi.org/10.1002/ca.22354
Herrick DB, Tanenbaum JE, Mankarious M, Vallabh S, Fleischman E, Kurra S, Burke SM, Roguski M, Mroz TE, Lavelle WF, Florman JE, Riesenburger RI (2018) The relationship between surgical site drains and reoperation for wound-related complications following posterior cervical spine surgery: a multicenter retrospective study. J Neurosurg Spine 29(6):628–634. https://doi.org/10.3171/2018.5.SPINE171313
Kotil K (2016) Closed drainage versus non-drainage for single-level lumbar disc surgery: relationship between epidural hematoma and fibrosis. Asian Spine J 10(6):1072–1078. https://doi.org/10.4184/asj.2016.10.6.1072
Mirzai H, Eminoglu M, Orguc S (2006) Are drains useful for lumbar disc surgery? A prospective, randomized clinical study. J Spinal Disord Tech 19(3):171–177. https://doi.org/10.1097/01.bsd.0000190560.20872.a7
Nadler SB, Hidalgo JH, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224–232
Gross JB (1983) Estimating allowable blood loss: corrected for dilution. Anesthesiology 58(3):277–280. https://doi.org/10.1097/00000542-198303000-00016
Heller GZ, Manuguerra M, Chow R (2016) How to analyze the visual analogue scale: myths, truths and clinical relevance. Scand J Pain 13:67–75. https://doi.org/10.1016/j.sjpain.2016.06.012
Huang Y, Yin J, Sun Z, Song S, Zhuang Y, Liu X, Du S, Rui Y (2020) Percutaneous endoscopic lumbar discectomy for LDH via a transforaminal approach versus an interlaminar approach: a meta-analysis. Orthopade 49(4):338–349. https://doi.org/10.1007/s00132-019-03710-z
von Eckardstein KL, Dohmes JE, Rohde V (2016) Use of closed suction devices and other drains in spinal surgery: results of an online, Germany-wide questionnaire. Eur Spine J 25(3):708–715. https://doi.org/10.1007/s00586-015-3790-8
Sehat KR, Evans R, Newman JH (2000) How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee 7(3):151–155. https://doi.org/10.1016/s0968-0160(00)00047-8
Smorgick Y, Baker KC, Bachison CC, Herkowitz HN, Montgomery DM, Fischgrund JS (2013) Hidden blood loss during posterior spine fusion surgery. Spine J 13(8):877–881. https://doi.org/10.1016/j.spinee.2013.02.008
Yang Y, Zhang L, Liu B, Pang M, Xie P, Chen Z, Wu W, Feng F, Rong L (2017) Hidden and overall haemorrhage following minimally invasive and open transforaminal lumbar interbody fusion. J Orthop Traumatol 18(4):395–400. https://doi.org/10.1007/s10195-017-0464-9
Zhang H, Chen ZX, Sun ZM, Jiang C, Ni WF, Lin Y, Wu YS (2017) Comparison of the total and hidden blood loss in patients undergoing open and minimally invasive transforaminal lumbar interbody fusion. World Neurosurg 107:739–743. https://doi.org/10.1016/j.wneu.2017.08.113
Lei F, Li Z, He W, Tian X, Zheng L, Kang J, Feng D (2020) Hidden blood loss and the risk factors after posterior lumbar fusion surgery: a retrospective study. Med (Baltim) 99(19):e20103. https://doi.org/10.1097/MD.0000000000020103
Su QH, Zhu K, Li YC, Chen T, Zhang Y, Tan J, Guo S (2020) Choice and management of negative pressure drainage in anterior cervical surgery. World J Clin Cases 8(11):2201–2209. https://doi.org/10.12998/wjcc.v8.i11.2201
Bertalanffy H, Eggert HR (1989) Complications of anterior cervical discectomy without fusion in 450 consecutive patients. Acta Neurochir (Wien) 99(1–2):41–50. https://doi.org/10.1007/BF01407775
Walid MS, Abbara M, Tolaymat A, Davis JR, Waits KD, Robinson JS 3rd, Robinson JS Jr (2012) The role of drains in lumbar spine fusion. World Neurosurg 77(3–4):564–568. https://doi.org/10.1016/j.wneu.2011.05.058
Lo Bianco S, Cavallaro D, Okatyeva V, Buffone A, Cannizzaro MA (2015) Thyroidectomy: natural drainage or negative drainage? Experience with randomized single-center study. Ann Ital Chir 86(3):267–272
Woo SH, Kim JP, Park JJ, Shim HS, Lee SH, Lee HJ, Won SJ, Son HY, Kim RB, Son YI (2013) Comparison of natural drainage group and negative drainage groups after total thyroidectomy: prospective randomized controlled study. Yonsei Med J 54(1):204–208. https://doi.org/10.3349/ymj.2013.54.1.204
Miao K, Ni S, Zhou X, Xu N, Sun R, Zhuang C, Wang Y (2015) Hidden blood loss and its influential factors after total hip arthroplasty. J Orthop Surg Res 10:36. https://doi.org/10.1186/s13018-015-0185-9
Faris PM, Ritter MA, Keating EM, Valeri CR (1991) Unwashed filtered shed blood collected after knee and hip arthroplasties. A source of autologous red blood cells. J Bone Joint Surg Am 73(10):1580
Erskine JG, Fraser C, Simpson R, Protheroe K, Walker ID (1981) Blood loss with knee joint replacement. J R Coll Surg Edinb 26(5):295–297
Chen T, Chang H, Liu K, Shi M, Song C, Meng X (2020) Drainage after posterior single-level instrumented lumbar fusion: natural pressure vs negative pressure. Med (Baltim) 99(7):e19154. https://doi.org/10.1097/MD.0000000000019154
Saleh K, Olson M, Resig S, Bershadsky B, Kuskowski M, Gioe T, Robinson H, Schmidt R, McElfresh E (2002) Predictors of wound infection in hip and knee joint replacement: results from a 20 year surveillance program. J Orthop Res 20(3):506–515. https://doi.org/10.1016/S0736-0266(01)00153-X
Pennington Z, Lubelski D, Molina C, Westbroek EM, Ahmed AK, Sciubba DM (2019) Prolonged post-surgical drain retention increases risk for deep wound infection after spine surgery. World Neurosurg 130:e846–e853. https://doi.org/10.1016/j.wneu.2019.07.013
Rao SB, Vasquez G, Harrop J, Maltenfort M, Stein N, Kaliyadan G, Klibert F, Epstein R, Sharan A, Vaccaro A, Flomenberg P (2011) Risk factors for surgical site infections following spinal fusion procedures: a case-control study. Clin Infect Dis 53(7):686–692. https://doi.org/10.1093/cid/cir506
Sankar B, Ray P, Rai J (2004) Suction drain tip culture in orthopaedic surgery: a prospective study of 214 clean operations. Int Orthop 28(5):311–314. https://doi.org/10.1007/s00264-004-0561-2
Drinkwater CJ, Neil MJ (1995) Optimal timing of wound drain removal following total joint arthroplasty. J Arthroplasty 10(2):185–189. https://doi.org/10.1016/s0883-5403(05)80125-1
Foley KT, Holly LT, Schwender JD (2003) Minimally invasive lumbar fusion. Spine (Phila Pa 1976) 28(15 Suppl):S26–35. https://doi.org/10.1097/01.BRS.0000076895.52418.5E
Liu H, Li J, Sun Y, Wang X, Wang W, Guo L, Zhang F, Zhang P, Zhang W (2022) A Comparative study of a new retractor-assisted WILTSE TLIF, MIS-TLIF, and traditional PLIF for treatment of single-level lumbar degenerative diseases. Orthop Surg 14(7):1317–1330. https://doi.org/10.1111/os.13289
Ali EMS, El-Hewala TA, Eladawy AM, Sheta RA (2022) Does minimally invasive transforaminal lumbar interbody fusion (MIS-TLIF) influence functional outcomes and spinopelvic parameters in isthmic spondylolisthesis? J Orthop Surg Res 17(1):272. https://doi.org/10.1186/s13018-022-03144-y
Modi HN, Shrestha U (2021) Comparison of clinical outcome and radiologic parameters in open TLIF versus MIS-TLIF in single- or double-level lumbar surgeries. Int J Spine Surg 15(5):962–970. https://doi.org/10.14444/8126
Hammad A, Wirries A, Ardeshiri A, Nikiforov O, Geiger F (2019) Open versus minimally invasive TLIF: literature review and meta-analysis. J Orthop Surg Res 14(1):229. https://doi.org/10.1186/s13018-019-1266-y
Le H, Anderson R, Phan E, Wick J, Barber J, Roberto R, Klineberg E, Javidan Y (2021) Clinical and radiographic comparison between open versus minimally invasive transforaminal lumbar interbody fusion with bilateral facetectomies. Global Spine J 11(6):903–910. https://doi.org/10.1177/2192568220932879
Hung PI, Chang MC, Chou PH, Lin HH, Wang ST, Liu CL (2017) Is a drain tube necessary for minimally invasive lumbar spine fusion surgery? Eur Spine J 26(3):733–737. https://doi.org/10.1007/s00586-016-4672-4
Funding
This study was supported by the Project of State Key Laboratory of Radiation Medicine and Protection, Soochow University (GZK1202128); Suzhou scientific research foundation of integrated traditional Chinese and Western Medicine (SKJYD2021220); Suzhou health talent plan (GSWS2021019).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest.
Ethical approval
This study was approved by the Second Affiliated Hospital of Soochow University's Ethics Committee (number: JD-HG-2020–22).
Informed consent
An informed consent was obtained by all patients included in the study
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiang, F., Wu, H., Pu, M. et al. Natural pressure drainage versus negative pressure drainage following transforaminal lumbar interbody fusion (TLIF) for the treatment of lumbar degeneration disease: a prospective cohort study. Arch Orthop Trauma Surg 143, 6131–6138 (2023). https://doi.org/10.1007/s00402-023-04937-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-023-04937-4