Abstract
Purpose
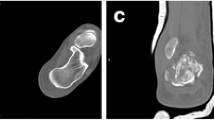
Severe calcaneal malunion is a clinical conundrum for the difficulty of calcaneal reconstruction without soft tissue complications. The aim of this study is to introduce the treatment strategy and preliminary results of staged Illizarov distraction histogenesis and corrective reconstruction for severe malunion of calcaneal fractures.
Methods
From June 2014 to May 2020, 14 patients with severe calcaneal malunion treated with the staged strategy were retrospectively analyzed. At the first stage, calcaneal osteotomy and external fixation with Ilizarov frame were performed. The restoration of the approximate configuration of calcaneus and the expansion of contractural soft tissue were achieved by gradual calcaneal distraction. At the second stage, corrective reconstruction was performed and autogenous iliac crest bone graft was used. Clinical and radiographic outcomes were evaluated at final follow-up.
Results
The average time of Ilizarov distraction and total fixation was 21.4 days and 41.0 days at first-stage treatment. At a mean follow-up of 33.1 months, the average American Orthopaedic Foot and Ankle Society (AOFAS) ankle and hindfoot score increased significantly from 24.0 to 72.4 (p < 0.01). And the mean visual analogue scale (VAS) score had improved remarkably from 8.2 to 2.4 (p < 0.01). Radiographs showed that talocalcaneal height, calcaneal width, calcaneal tuberosity height, hindfoot alignment angle, and talar declination angle were improved to a great extent (p < 0.01). Only one patient had minor pin site infection at first-stage treatment and one got superficial wound infection after second-stage surgery. No wound dehiscence, skin necrosis, or deep infection occurred.
Conclusion
Staged Ilizarov distraction histogenesis and corrective reconstruction is a safe and effective treatment strategy for reducing soft tissue complications and improving reconstruction results in surgical correction of severe calcaneal malunion.





Similar content being viewed by others
Data availability
The data of the current study is available from the corresponding author on reasonable request.
References
Atkins RM (2014) The treatment of calcaneal malunion. Foot Ankle Clin 19(3):521–540. https://doi.org/10.1016/j.fcl.2014.06.016
Iceman KL, Magnus MK, Roukis TS (2019) Salvaging the unsalvageable severe malunion deformity after displaced intra-articular calcaneal fractures: what options exist? Clin Podiatr Med Surg 36(2):339–347. https://doi.org/10.1016/j.cpm.2018.10.013
Eckstein C, Kottmann T, Füchtmeier B, Müller F (2016) Long-term results of surgically treated calcaneal fractures: an analysis with a minimum follow-up period of twenty years. Int Orthop 40(2):365–370. https://doi.org/10.1007/s00264-015-3042-x
Stapleton JJ, Belczyk R, Zgonis T (2009) Surgical treatment of calcaneal fracture malunions and posttraumatic deformities. Clin Podiatr Med Surg 26(1):79–90. https://doi.org/10.1016/j.cpm.2008.10.003
Banerjee R, Saltzman C, Anderson RB, Nickisch F (2011) Management of calcaneal malunion. J Am Acad Orthop Surg 19(1):27–36. https://doi.org/10.5435/00124635-201101000-00004
Clare MP, Crawford WS (2017) Managing complications of calcaneus fractures. Foot Ankle Clin 22(1):105–116. https://doi.org/10.1016/j.fcl.2016.09.007
Rammelt S, Grass R, Zawadski T, Biewener A, Zwipp H (2004) Foot function after subtalar distraction bone-block arthrodesis. a prospective study. J Bone Jt Surg Br 86(5):659–668. https://doi.org/10.1302/0301-620x.86b5.14205
Trnka HJ, Easley ME, Lam PW, Anderson CD, Schon LC, Myerson MS (2001) Subtalar distraction bone block arthrodesis. J Bone Jt Surg Br 83(6):849–854. https://doi.org/10.1302/0301-620x.83b6.10537
Amendola A, Lammens P (1996) Subtalar arthrodesis using interposition iliac crest bone graft after calcaneal fracture. Foot Ankle Int 17(10):608–614. https://doi.org/10.1177/107110079601701004
Ilizarov GA (1990) Clinical application of the tension-stress effect for limb lengthening. Clin Orthop Relat Res 250:8–26. https://doi.org/10.1097/00003086-199001000-00003
Aronson J (1997) Limb-lengthening, skeletal reconstruction, and bone transport with the Ilizarov method. J Bone Jt Surg Am 79(8):1243–1258. https://doi.org/10.2106/00004623-199708000-00019
Robert Rozbruch S, Weitzman AM, Tracey Watson J, Freudigman P, Katz HV, Ilizarov S (2006) Simultaneous treatment of tibial bone and soft-tissue defects with the Ilizarov method. J Orthop Trauma 20(3):197–205. https://doi.org/10.1097/00005131-200603000-00006
Paley D, Maar DC (2000) Ilizarov bone transport treatment for tibial defects. J Orthop Trauma 14(2):76–85. https://doi.org/10.1097/00005131-200002000-00002
Rammelt S, Zwipp H (2013) Corrective arthrodeses and osteotomies for post-traumatic hindfoot malalignment: indications, techniques, results. Int Orthop 37(9):1707–1717. https://doi.org/10.1007/s00264-013-2021-3
Thompson MJ, Roukis TS (2019) Management of calcaneal fracture malunion with bone block distraction arthrodesis: a systematic review and meta-analysis. Clin Podiatr Med Surg 36(2):307–321. https://doi.org/10.1016/j.cpm.2018.10.011
Schepers T (2013) The subtalar distraction bone block arthrodesis following the late complications of calcaneal fractures: a systematic review. Foot 23(1):39–44. https://doi.org/10.1016/j.foot.2012.10.004
Rammelt S, Marx C (2020) Managing severely malunited calcaneal fractures and fracture-dislocations. Foot Ankle Clin 25(2):239–256. https://doi.org/10.1016/j.fcl.2020.02.005
Chen YJ, Huang TJ, Hsu KY, Hsu RW, Chen CW (1998) Subtalar distractional realignment arthrodesis with wedge bone grafting and lateral decompression for calcaneal malunion. J Trauma 45(4):729–737. https://doi.org/10.1097/00005373-199810000-00018
Lerner A, Ullmann Y, Stein H, Peled IJ (2000) Using the Ilizarov external fixation device for skin expansion. Ann Plast Surg 45(5):535–537. https://doi.org/10.1097/00000637-200045050-00012
Borges Filho PT, Neves RI, Gemperli R, Kaweski S, Kahler SH, Banducci DR, Manders EK (1991) Soft-tissue expansion in lower extremity reconstruction. Clin Plast Surg 18(3):593–599. https://doi.org/10.1016/S0094-1298(20)30857-9
Calhoun JH, Evans EB, Herndon DN (1992) Techniques for the management of burn contractures with the Ilizarov Fixator. Clin Orthop Relat Res 280:117–124. https://doi.org/10.1097/00003086-199207000-00014
Carr JB, Hansen ST, Benirschke SK (1988) Subtalar distraction bone block fusion for late complications of os calcis fractures. Foot Ankle 9(2):81–86. https://doi.org/10.1177/107110078800900204
Burton DC, Olney BW, Horton GA (1998) Late results of subtalar distraction fusion. Foot Ankle Int 19(4):197–202. https://doi.org/10.1177/107110079801900402
Bednarz PA, Beals TC, Manoli A 2nd (1997) Subtalar distraction bone block fusion: an assessment of outcome. Foot Ankle Int 18(12):785–791. https://doi.org/10.1177/107110079701801206
Myerson M, Quill GE Jr (1993) Late complications of fractures of the calcaneus. J Bone Jt Surg Am 75(3):331–341. https://doi.org/10.2106/00004623-199303000-00004
Pollard JD, Schuberth JM (2008) Posterior bone block distraction arthrodesis of the subtalar joint: a review of 22 cases. J Foot Ankle Surg 47(3):191–198. https://doi.org/10.1053/j.jfas.2008.01.003
Al-Ashhab ME (2013) Treatment for calcaneal malunion. Eur J Orthop Surg Traumatol 23(8):961–966. https://doi.org/10.1007/s00590-012-1110-0
Wang B, Zhang X, Huo Y, Liu W, Wang W, Shao X (2019) Calcaneal lengthening for partial traumatic loss of the calcaneus. Injury 50(3):796–803. https://doi.org/10.1016/j.injury.2019.01.025
Marti RK, de Heus JA, Roolker W, Poolman RW, Besselaar PP (1999) Subtalar arthrodesis with correction of deformity after fractures of the os calcis. J Bone Jt Surg Br 81(4):611–616. https://doi.org/10.1302/0301-620x.81b4.9386
Yu GR, Hu SJ, Yang YF, Zhao HM, Zhang SM (2013) Reconstruction of calcaneal fracture malunion with osteotomy and subtalar joint salvage: technique and outcomes. Foot Ankle Int 34(5):726–733. https://doi.org/10.1177/1071100713479766
Ohuchi H, Chavez JS, Alvarez CAD (2019) Changes in calcaneal pitch and heel fat pad thickness in static weight bearing radiographs while wearing shoes with arch support and heel cup orthotics. Asia Pac J Sports Med Arthrosc Rehabil Technol 17:21–24. https://doi.org/10.1016/j.asmart.2019.07.001
Sanders FRK, Peters JJ, Schallig W, Mittlmeier T, Schepers T (2020) What is the added value of pedobarography for assessing functional outcome of displaced intra-articular calcaneal fractures? a systematic review of existing literature. Clin Biomech 72:8–15. https://doi.org/10.1016/j.clinbiomech.2019.11.013
Acknowledgements
None.
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
ZH and CY performed the operations. Data collection and material preparation were performed by all authors. First draft of the manuscript was written by GTJ, then ZH, LYX, LX and LJ commented for adequate changes of its final version. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Ethical approval
This study was performed in accordance with the Helsinki declaration of 1964, and it was approved by the relevant Institutional Review Board at the West China Hospital of Sichuan University.
Informed consent
Informed consent was obtained from all patients.
Consent to participate
Informed consent was obtained from all patients.
Consent to publish
Informed consent was obtained.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gan, TJ., Li, YX., Liu, X. et al. Staged Ilizarov distraction histogenesis and corrective reconstruction for severe malunited calcaneal fractures. Arch Orthop Trauma Surg 143, 2845–2854 (2023). https://doi.org/10.1007/s00402-022-04449-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-022-04449-7