Abstract
Introduction
The interval slide procedure (IS) has been introduced to improve mobility in massive, retracted rotator cuff tears. As clinical studies showed controversial results, the benefit of the IS is still widely discussed.
Aim
Aim of this study was to analyze the effect of IS procedure on tendon mobility in a fresh porcine cadaver model.
Materials and methods
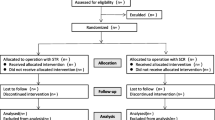
In 30 fresh porcine cadaver shoulders with artificial supraspinatus defect tendon mobility was tested by measuring the load (in N) during tendon reduction to the footprint at the greater tubercle using a sensor enhanced arthroscopic grasper (t1). In intervention group (N = 15) anterior IS (t2), posterior IS (t3) and intraarticular capsule release (t4) were successively performed, each followed by tendon mobility assessment. Tendon mobility of the control group (N = 15) was measured in same time schedule without intervention.
Results
Mobility did not differ between groups for native tendons (CG 28.0 ± 11.2 N vs. IG 26.6 ± 11.6 N; P = 0.75). IS procedure significantly improves mobility at about 25.2% (t1 26.6 ± 11.6 N vs. t4 19.9 ± 12.3 N; P < 0.001) compared to the native tendon and 34.1% compared to CG (CG 30.2 ± 13.7 N vs. 19.9 ± 12.3 N; P = 0.026). In posthoc analyzes, anterior IS (P < 0.001) and capsule release (P = 0.005) significantly increased mobility, whereas the posterior IS did not (P = 0.778).
Conclusion
The IS procedure results in increased supraspinatus tendon mobility in fresh porcine cadaver shoulders. However, performing the posterior IS subsequent to the anterior IS no significant improvement of mobility has been observed.






Similar content being viewed by others
References
Yamaguchi K, Ditsios K, Middleton WD, Hildebolt CF, Galatz LM, Teefey SA (2006) The demographic and morphological features of rotator cuff disease. A comparison of asymptomatic and symptomatic shoulders. J Bone Jt Surg Am 88(8):1699–1704. https://doi.org/10.2106/JBJS.E.00835
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H, Kobayashi T (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elbow Surg 19(1):116–120. https://doi.org/10.1016/j.jse.2009.04.006
Savage AJ, Spruiell MD, Schwertz JM, McGwin G, Eberhardt A, Ponce BA (2013) The effect of sliding knots on the suture-tendon interface strength: a biomechanical analysis comparing sliding and static arthroscopic knots. Am J Sports Med 41(2):296–301. https://doi.org/10.1177/0363546512472168
Barber FA, Herbert MA (2013) Cyclic loading biomechanical analysis of the pullout strengths of rotator cuff and glenoid anchors: 2013 update. Arthroscopy 29(5):832–844. https://doi.org/10.1016/j.arthro.2013.01.028
Barber FA, Herbert MA (2017) All-suture anchors: biomechanical analysis of pullout strength, displacement, and failure mode. Arthroscopy 33(6):1113–1121. https://doi.org/10.1016/j.arthro.2016.09.031
Colvin AC, Egorova N, Harrison AK, Moskowitz A, Flatow EL (2012) National trends in rotator cuff repair. J Bone Jt Surg Am 94(3):227–233. https://doi.org/10.2106/jbjs.j.00739
Kim JH, Hong IT, Ryu KJ, Bong ST, Lee YS, Kim JH (2014) Retear rate in the late postoperative period after arthroscopic rotator cuff repair. Am J Sports Med 42(11):2606–2613. https://doi.org/10.1177/0363546514547177
Kim KC, Shin HD, Cha SM, Park JY (2014) Repair integrity and functional outcome after arthroscopic conversion to a full-thickness rotator cuff tear: articular- versus bursal-side partial tears. Am J Sports Med 42(2):451–456. https://doi.org/10.1177/0363546513512770
Hein J, Reilly JM, Chae J, Maerz T, Anderson K (2015) Retear rates after arthroscopic single-row, double-row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow-up: a systematic review. Arthroscopy 31(11):2274–2281. https://doi.org/10.1016/j.arthro.2015.06.004
Kuzel BR, Grindel S, Papandrea R, Ziegler D (2013) Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg 21(10):613–623. https://doi.org/10.5435/jaaos-21-10-613
Meyer DC, Wieser K, Farshad M, Gerber C (2012) Retraction of supraspinatus muscle and tendon as predictors of success of rotator cuff repair. Am J Sports Med 40(10):2242–2247. https://doi.org/10.1177/0363546512457587
Davidson PA, Rivenburgh DW (2000) Rotator cuff repair tension as a determinant of functional outcome. J Shoulder Elbow Surg 9(6):502–506. https://doi.org/10.1067/mse.2000.109385
Kim YK, Jung KH, Kim JW, Kim US, Hwang DH (2018) Factors affecting rotator cuff integrity after arthroscopic repair for medium-sized or larger cuff tears: a retrospective cohort study. J Shoulder Elbow Surg 27(6):1012–1020. https://doi.org/10.1016/j.jse.2017.11.016
Anley CM, Chan SK, Snow M (2014) Arthroscopic treatment options for irreparable rotator cuff tears of the shoulder. World J Orthop 5(5):557–565. https://doi.org/10.5312/wjo.v5.i5.557
Berdusco R, Trantalis JN, Nelson AA, Sohmer S, More KD, Wong B, Boorman RS, Lo IK (2015) Arthroscopic repair of massive, contracted, immobile tears using interval slides: clinical and MRI structural follow-up. Knee Surg Sports Traumatol Arthrosc 23(2):502–507. https://doi.org/10.1007/s00167-013-2683-9
Lo IK, Burkhart SS (2004) Arthroscopic repair of massive, contracted, immobile rotator cuff tears using single and double interval slides: technique and preliminary results. Arthroscopy 20(1):22–33. https://doi.org/10.1016/j.arthro.2003.11.013
Millett PJ, Warth RJ (2014) Posterosuperior rotator cuff tears: classification, pattern recognition, and treatment. J Am Acad Orthop Surg 22(8):521–534. https://doi.org/10.5435/jaaos-22-08-521
Tauro JC (1999) Arthroscopic “interval slide” in the repair of large rotator cuff tears. Arthroscopy 15(5):527–530. https://doi.org/10.1053/ar.1999.v15.0150521
Tauro JC (2004) Arthroscopic repair of large rotator cuff tears using the interval slide technique. Arthroscopy 20(1):13–21. https://doi.org/10.1016/j.arthro.2003.10.013
Kim SJ, Kim SH, Lee SK, Seo JW, Chun YM (2013) Arthroscopic repair of massive contracted rotator cuff tears: aggressive release with anterior and posterior interval slides do not improve cuff healing and integrity. J Bone Jt Surg Am 95(16):1482–1488. https://doi.org/10.2106/jbjs.l.01193
Porschke F, Luecke C, Guehring T, Weiss C, Studier-Fischer S, Gruetzner PA, Schnetzke M (2020) Mobility assessment of the supraspinatus in a porcine cadaver model using a sensor-enhanced, arthroscopic grasper. Ann Biomed Eng. https://doi.org/10.1007/s10439-020-02572-3
Van Ee CA, Chasse AL, Myers BS (2000) Quantifying skeletal muscle properties in cadaveric test specimens: effects of mechanical loading, postmortem time, and freezer storage. J Biomech Eng 122(1):9–14
Koenig HE, Liebich HG (2020) Veterinary anatomy of domestic animals, 7th edn. Georg Thieme Verlag
Constantinescu GM (2018) Illustrated veterinary anatomical nomenclature. MVS Medizinverlage Stuttgart GmbH
Kim DH, Jang YH, Choi YE, Lee HR, Kim SH (2016) Evaluation of repair tension in arthroscopic rotator cuff repair: does it really matter to the integrity of the rotator cuff? Am J Sports Med 44(11):2807–2812. https://doi.org/10.1177/0363546516651831
Tashjian RZ, Erickson GA, Robins RJ, Zhang Y, Burks RT, Greis PE (2017) Influence of preoperative musculotendinous junction position on rotator cuff healing after double-row repair. Arthroscopy 33(6):1159–1166. https://doi.org/10.1016/j.arthro.2016.12.010
Tashjian RZ, Hung M, Burks RT, Greis PE (2013) Influence of preoperative musculotendinous junction position on rotator cuff healing using single-row technique. Arthroscopy 29(11):1748–1754. https://doi.org/10.1016/j.arthro.2013.08.014
Kim YK, Moon SH, Cho SH (2013) Treatment outcomes of single- versus double-row repair for larger than medium-sized rotator cuff tears: the effect of preoperative remnant tendon length. Am J Sports Med 41(10):2270–2277. https://doi.org/10.1177/0363546513499000
Baums MH, Spahn G, Buchhorn GH, Schultz W, Hofmann L, Klinger HM (2012) Biomechanical and magnetic resonance imaging evaluation of a single- and double-row rotator cuff repair in an in vivo sheep model. Arthroscopy 28(6):769–777. https://doi.org/10.1016/j.arthro.2011.11.019
Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ (2014) Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg 23(4):586–597. https://doi.org/10.1016/j.jse.2013.10.006
Lee KW, Moon KH, Ma CH, Lee GS, Yang DS, Choy WS (2018) Clinical and radiologic outcomes after medializing and not medializing rotator cuff tendon attachment site on chronic retracted rotator cuff tears. Arthroscopy 34(8):2298–2307. https://doi.org/10.1016/j.arthro.2018.03.015
Yamamoto N, Itoi E, Tuoheti Y, Seki N, Abe H, Minagawa H, Shimada Y, Okada K (2007) Glenohumeral joint motion after medial shift of the attachment site of the supraspinatus tendon: a cadaveric study. J Shoulder Elbow Surg 16(3):373–378. https://doi.org/10.1016/j.jse.2006.06.016
Liu J, Hughes RE, O’Driscoll SW, An KN (1998) Biomechanical effect of medial advancement of the supraspinatus tendon. A study in cadavera. J Bone Jt Surg Am 80(6):853–859
Pauly S, Kieser B, Schill A, Gerhardt C, Scheibel M (2010) Biomechanical comparison of 4 double-row suture-bridging rotator cuff repair techniques using different medial-row configurations. Arthroscopy 26(10):1281–1288. https://doi.org/10.1016/j.arthro.2010.02.013
Mihata T, Fukuhara T, Jun BJ, Watanabe C, Kinoshita M (2011) Effect of shoulder abduction angle on biomechanical properties of the repaired rotator cuff tendons with 3 types of double-row technique. Am J Sports Med 39(3):551–556. https://doi.org/10.1177/0363546510388152
Kesmezacar H, Akgun I, Ogut T, Gokay S, Uzun I (2008) The coracoacromial ligament: the morphology and relation to rotator cuff pathology. J Shoulder Elbow Surg 17(1):182–188. https://doi.org/10.1016/j.jse.2007.05.015
Neer CS 2nd, Satterlee CC, Dalsey RM, Flatow EL (1992) The anatomy and potential effects of contracture of the coracohumeral ligament. Clin Orthop Relat Res 280:182–185
Teunis T, Lubberts B, Reilly BT, Ring D (2014) A systematic review and pooled analysis of the prevalence of rotator cuff disease with increasing age. J Shoulder Elbow Surg 23(12):1913–1921. https://doi.org/10.1016/j.jse.2014.08.001
Lu YJ, Lu Y, Zhu YM, Zhang Q, Li GP, Tao JF, Jiang CY (2012) Preliminary histological and biomechanical study about the timing of surgical repair for acute rotator cuff tears in rabbits. Zhonghua wai ke za zhi Chin J Surg 50(6):560–565
Gimbel JA, Van Kleunen JP, Mehta S, Perry SM, Williams GR, Soslowsky LJ (2004) Supraspinatus tendon organizational and mechanical properties in a chronic rotator cuff tear animal model. J Biomech 37(5):739–749. https://doi.org/10.1016/j.jbiomech.2003.09.019
Acevedo DC, Vanbeek C, Lazarus MD, Williams GR, Abboud JA (2014) Reverse shoulder arthroplasty for proximal humeral fractures: update on indications, technique, and results. J Shoulder Elbow Surg 23(2):279–289. https://doi.org/10.1016/j.jse.2013.10.003
Funding
This research received no external funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
Due to the original purpose for the food industry no ethical, respectively, approval of an animal welfare organization was needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Porschke, F., Schnetzke, M., Luecke, C. et al. Biomechanical analysis of the interval slide procedure: a fresh porcine cadaver study. Arch Orthop Trauma Surg 142, 3395–3403 (2022). https://doi.org/10.1007/s00402-021-04294-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-04294-0