Abstract
Introduction
As more centers introduce same-day discharge (SDD) total joint arthroplasty (TJA) programs, it is vital to understand the factors associated with successful outpatient TJA and whether outcomes vary for those that failed SDD. The purpose of this study is to compare outcomes of patients that are successfully discharged home the day of surgery to those that fail-to-launch (FTL) and require a longer in-hospital stay.
Materials and methods
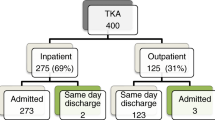
We retrospectively reviewed all patients who enrolled in our institution’s SDD TJA program from 2015 to 2020. Patients were stratified into two cohorts based on whether they were successfully SDD or FTL. Outcomes of interest included discharge disposition, 90-day readmissions, 90-day revisions, surgical time, and patient-reported outcome measures (PROMs) as assessed by the FJS-12 (3 months, 1 year, and 2 years), HOOS, JR, and KOOS, JR (preoperatively, 3 months, and 1 year). Demographic differences were assessed with chi-square and Mann–Whitney U tests. Outcomes were compared using multilinear regressions, controlling for demographic differences.
Results
A total of 1491 patients were included. Of these, 1384 (93%) were successfully SDD while 107 (7%) FTL and required a longer length-of-stay. Patients who FTL were more likely to be non-married (p = 0.007) and ASA class III (p = 0.017) compared to those who were successfully SDD. Surgical time was significantly longer for those who FTL compared to those who were successfully SDD (100.86 vs. 83.42 min; p < 0.001). Discharge disposition (p = 0.100), 90-day readmissions (p = 0.897), 90-day revisions (p = 0.997), and all PROM scores both preoperatively and postoperatively did not significantly differ between the two cohorts.
Conclusion
Our results support the notion that FTL is not a predictor of adverse outcomes as patients who FTL achieved similar outcomes as those who were successfully SDD. The findings of this study can aid orthopedic surgeons to educate their patients who wish to participate in a similar program, as well as patients that have concerns after they failed to go home on the day of surgery.
Level III Evidence
Retrospective Cohort Study.
Similar content being viewed by others
References
Pivec R, Johnson AJ, Mears SC, Mont MA (2012) Hip arthroplasty. In: The Lancet
Function M, Performance M, Arthroplasty WJ (2008) Standard of care: total knee arthroplasty standard of care : total knee arthroplasty. Brigham woman’s Hosp
Ethgen O, Bruyerè O, Richy F et al (2004) Health-related quality of life in total hip and total knee arthroplasty: a qualitative and systematic review of the literature. J Bone Jt Surg - Ser A 86:963–974
Canovas F, Dagneaux L (2018) Quality of life after total knee arthroplasty. Orthop Traumatol Surg Res
Kremers HM, Larson DR, Crowson CS et al (2014) Prevalence of total hip and knee replacement in the United States. J Bone Jt Surg - Am 97:1386–1397. https://doi.org/10.2106/JBJS.N.01141
Burn E, Edwards CJ, Murray DW et al (2018) Trends and determinants of length of stay and hospital reimbursement following knee and hip replacement: Evidence from linked primary care and NHS hospital records from 1997 to 2014. BMJ Open. https://doi.org/10.1136/bmjopen-2017-019146
Weiser MC, Kim KY, Anoushiravani AA et al (2018) Outpatient total hip arthroplasty has minimal short-term complications with the use of institutional protocols. J Arthroplasty 33:3502–3507. https://doi.org/10.1016/j.arth.2018.07.015
Hoffmann JD, Kusnezov NA, Dunn JC, et al (2018) The shift to same-day outpatient joint arthroplasty: a systematic review. J. Arthroplasty
Sher A, Keswani A, Yao D et al (2017) Predictors of same-day discharge in primary total joint arthroplasty patients and risk factors for post-discharge complications. J Arthroplasty. https://doi.org/10.1016/j.arth.2016.12.017
Berger RA, Sanders SA, Thill ES, et al (2009) Newer anesthesia and rehabilitation protocols enable outpatient hip replacement in selected patients. In: Clin Orthopaed Relat Res
Khan SK, Malviya A, Muller SD et al (2014) Reduced short-term complications and mortality following enhanced recovery primary hip and knee arthroplasty: results from 6,000 consecutive procedures. Acta Orthop. https://doi.org/10.3109/17453674.2013.874925
Padilla JA, Gabor JA, Schwarzkopf R, Davidovitch RI (2019) A novel opioid-sparing pain management protocol following total hip arthroplasty: effects on opioid consumption, pain severity, and patient-reported outcomes. J Arthroplasty 34:2669–2675. https://doi.org/10.1016/j.arth.2019.06.038
Gillis ME, Dobransky J, Dervin GF (2019) Defining growth potential and barriers to same day discharge total knee arthroplasty. Int Orthop 43:1387–1393. https://doi.org/10.1007/s00264-018-4100-y
Stambough JB, Nunley RM, Curry MC et al (2015) Rapid recovery protocols for primary total hip arthroplasty can safely reduce length of stay without increasing readmissions. J Arthroplasty. https://doi.org/10.1016/j.arth.2015.01.023
Berend KR, Lombardi AV, Mallory TH (2004) Rapid recovery protocol for peri-operative care of total hip and total knee arthroplasty patients. Surg Technol Int
Kehlet H, Wilmore DW (2008) Evidence-based surgical care and the evolution of fast-track surgery. Ann Surg. https://doi.org/10.1097/SLA.0b013e31817f2c1a
Lovecchio F, Alvi H, Sahota S et al (2016) Is outpatient arthroplasty as safe as fast-track inpatient arthroplasty? a propensity score matched analysis. J Arthroplasty 31:197–201. https://doi.org/10.1016/j.arth.2016.05.037
Springer BD, Odum SM, Vegari DN et al (2017) Impact of inpatient versus outpatient total joint arthroplasty on 30-day hospital readmission rates and unplanned episodes of care. Orthop Clin North Am 48:15–23
Otero JE, Gholson JJ, Pugely AJ et al (2016) Length of hospitalization after joint arthroplasty: does early discharge affect complications and readmission rates? J Arthroplasty 31:2714–2725. https://doi.org/10.1016/j.arth.2016.07.026
Kort NP, Bemelmans YFL, van der Kuy PHM, et al (2017) Patient selection criteria for outpatient joint arthroplasty. Knee Surg Sport Traumatol Arthrosc
Meneghini RM, Ziemba-Davis M, Ishmael MK et al (2017) Safe selection of outpatient joint arthroplasty patients with medical risk stratification: the “outpatient arthroplasty risk assessment score.” J Arthroplasty 32:2325–2331. https://doi.org/10.1016/j.arth.2017.03.004
Kim KY, Feng JE, Anoushiravani AA et al (2018) Rapid discharge in total hip arthroplasty: utility of the outpatient arthroplasty risk assessment tool in predicting same-day and next-day discharge. J Arthroplasty 33:2412–2416. https://doi.org/10.1016/j.arth.2018.03.025
Goyal N, Chen AF, Padgett SE et al (2017) Otto aufranc award: a multicenter, randomized study of outpatient versus inpatient total hip arthroplasty. Clin Orthop Relat Res 475:364–372. https://doi.org/10.1007/s11999-016-4915-z
Gromov K, Kjærsgaard-Andersen P, Revald P et al (2017) Feasibility of outpatient total hip and knee arthroplasty in unselected patients: A prospective 2-center study. Acta Orthop. https://doi.org/10.1080/17453674.2017.1314158
Coenders MJ, Mathijssen NMC, Vehmeijer SBW (2020) Three and a half years’ experience with outpatient total hip arthroplasty. Bone Jt J. https://doi.org/10.1302/0301-620X.102B1.BJJ-2019-0045.R2
Fraser JF, Danoff JR, Manrique J et al (2018) Identifying reasons for failed same-day discharge following primary total hip arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2018.08.003
Gogineni HC, Gray CF, Prieto HA et al (2019) Transition to outpatient total hip and knee arthroplasty: experience at an academic tertiary care center. Arthroplast Today 5:100–105. https://doi.org/10.1016/j.artd.2018.10.008
Keulen MHF, Asselberghs S, Bemelmans YFL et al (2020) Reasons for unsuccessful same-day discharge following outpatient hip and knee arthroplasty: 5½ years’ experience from a single institution. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.04.064
Keulen MHF, Asselberghs S, Boonen B et al (2020) Predictors of (un)successful same-day discharge in selected patients following outpatient hip and knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2020.03.034
Lieberman EG, Hansen EJ, Clohisy JC et al (2021) Allergies, preoperative narcotic use, and increased age predict failed same day discharge after joint replacement. J Arthroplasty. https://doi.org/10.1016/j.arth.2021.01.015
Giesinger JM, Kuster MS, Holzner B, Giesinger K (2013) Development of a computer-adaptive version of the forgotten joint score. J Arthroplasty 28:418–422. https://doi.org/10.1016/j.arth.2012.08.026
Lyman S, Lee YY, Franklin PD et al (2016) Validation of the HOOS, JR: a short-form hip replacement survey. Clin Orthop Relat Res 474:1472–1482. https://doi.org/10.1007/s11999-016-4718-2
Lyman S, Lee YY, Franklin PD et al (2016) Validation of the KOOS, JR: a short-form knee arthroplasty outcomes survey. Clin Orthop Relat Res 474:1461–1471. https://doi.org/10.1007/s11999-016-4719-1
Aynardi M, Post Z, Ong A et al (2014) Outpatient surgery as a means of cost reduction in total hip arthroplasty: a case-control study. HSS J 10:252–255. https://doi.org/10.1007/s11420-014-9401-0
Kim KY, Anoushiravani AA, Elbuluk A et al (2018) Primary total hip arthroplasty with same-day discharge: Who failed and why. Orthopedics. https://doi.org/10.3928/01477447-20171127-01
Hartog YMD, Mathijssen NMC, Vehmeijer SBW (2013) Reduced length of hospital stay after the introduction of a rapid recovery protocol for primary THA procedures. Acta Orthop. https://doi.org/10.3109/17453674.2013.838657
Larsen JR, Skovgaard B, Prynø T et al (2017) Feasibility of day-case total hip arthroplasty: A single-centre observational study. HIP Int. https://doi.org/10.5301/hipint.5000421
Parcells BW, Giacobbe D, MacKnet D et al (2016) Total joint arthroplasty in a stand-alone ambulatory surgical center: Short-term outcomes. Orthopedics. https://doi.org/10.3928/01477447-20160419-06
Gabor JA, Singh V, Schwarzkopf R, Davidovitch RI (2020) Similar outcomes after hospital-based same-day discharge vs inpatient total hip arthroplasty. Arthroplast Today 6:451–456. https://doi.org/10.1016/j.artd.2020.05.008
Berger RA, Kusuma SK, Sanders SA, et al (2009) The feasibility and perioperative complications of outpatient knee arthroplasty. In: Clin Orthopaed Relat Res
Sibia US, King PJ, MacDonald JH (2017) Who is not a candidate for a 1-day hospital-based total knee arthroplasty? J Arthroplasty. https://doi.org/10.1016/j.arth.2016.06.055
Husted H, Holm G, Jacobsen S (2008) Predictors of length of stay and patient satisfaction after hip and knee replacement surgery: Fast-track experience in 712 patients. Acta Orthop. https://doi.org/10.1080/17453670710014941
Sibia US, MacDonald JH, King PJ (2016) Predictors of hospital length of stay in an enhanced recovery after surgery program for primary total hip arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2016.02.060
Ali A, Lindstrand A, Sundberg M, Flivik G (2017) Preoperative anxiety and depression correlate with dissatisfaction after total knee arthroplasty: a prospective longitudinal cohort study of 186 patients, with 4-year follow-up. J Arthroplasty 32:767–770. https://doi.org/10.1016/j.arth.2016.08.033
Lopez-Olivo MA, Landon GC, Siff SJ et al (2011) Psychosocial determinants of outcomes in knee replacement. Ann Rheum Dis 70:1775–1781. https://doi.org/10.1136/ard.2010.146423
Horn EE, Xu Y, Beam CR et al (2013) Accounting for the physical and mental health benefits of entry into marriage: A genetically informed study of selection and causation. J Fam Psychol 27:30–41. https://doi.org/10.1037/a0029803
Carr D, Springer KW (2010) Advances in families and health research in the 21st century. J Marriage Fam 72:743–761. https://doi.org/10.1111/j.1741-3737.2010.00728.x
Robards J, Evandrou M, Falkingham J, Vlachantoni A (2012) Marital status, health and mortality. Maturitas 73:295–299. https://doi.org/10.1016/j.maturitas.2012.08.007
Lall AC, Schwarzman GR, Battaglia MR et al (2019) Effect of marital status on patient-reported outcomes following total hip arthroplasty: a matched analysis with minimum 2-year follow-up. HIP Int. https://doi.org/10.1177/1120700019864015
Belmont PJ, Goodman GP, Waterman BR, et al (2014) Thirty-day postoperative complications and mortality following total knee arthroplasty: Incidence and risk factors among a national sample of 15,321 patients. J Bone Jt Surg Ser A
Mathijssen NMC, Verburg H, van Leeuwen CCG et al (2016) Factors influencing length of hospital stay after primary total knee arthroplasty in a fast-track setting. Knee Surg Sport Traumatol Arthrosc. https://doi.org/10.1007/s00167-015-3932-x
Inneh IA (2015) The combined influence of sociodemographic, preoperative comorbid and intraoperative factors on longer length of stay after elective primary total knee arthroplasty. J Arthroplasty. https://doi.org/10.1016/j.arth.2015.05.032
Garbarino LJ, Gold PA, Sodhi N et al (2019) The effect of operative time on in-hospital length of stay in revision total knee arthroplasty. Ann Transl Med 7:66–66. https://doi.org/10.21037/atm.2019.01.54
Jans B-N, Solgaard S et al (2012) Orthostatic intolerance during early mobilization after fast-track hip arthroplasty. Br J Anaesth. https://doi.org/10.1093/bja/aer403
Funding
No funding was provided for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
V.S and A.M.N have nothing to disclose. W.M holds stock options in OrthoAlign. R.S is a paid consultant for Intellijoint and Smith & Nephew and holds stock options in Gauss Surgical. R.D is a paid consultant for Radlink, Schaerer Medical, Exactech, and Medtronics. The authors declare that they have no conflict of interest pertinent to this study.
Ethical approval
The present study was exempt from human-subjects review by our institutional review board (IRB).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, V., Nduaguba, A.M., Macaulay, W. et al. Failure to Meet Same-Day Discharge is Not a Predictor of Adverse Outcomes. Arch Orthop Trauma Surg 142, 861–869 (2022). https://doi.org/10.1007/s00402-021-03983-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-021-03983-0