Abstract
Background
Closed reduction and pinning is the accepted treatment choice for dislocated supracondylar humeral fractures in children (SCHF). Rates of open reduction, complications and outcome are reported to be dependent on delay of surgery. We investigated whether delay of surgery had influence on the incidence of open reduction, complications and outcome of surgical treatment of SCHFs in the authors’ institution.
Methods
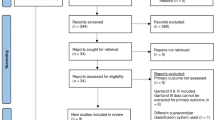
Three hundred and forty-one children with 343 supracondylar humeral fractures (Gartland II: 144; Gartland III: 199) who underwent surgery between 2000 and 2009 were retrospectively analysed. The group consisted of 194 males and 149 females. The average age was 6.3 years. Mean follow-up was 6.2 months. Time interval between trauma and surgical intervention was determined using our institutional database. Clinical and radiographical data were collected for each group. Influence of delay of treatment on rates of open reduction, complications and outcome was calculated using logistic regression analysis. Furthermore, patients were grouped into 4 groups of delay (<6 h, n = 166; 6–12 h, n = 95; 12–24 h, n = 68; >24 h, n = 14) and the aforementioned variables were compared among these groups.
Results
The incidence of open procedures in 343 supracondylar humeral fractures was 2.6 %. Complication rates were similar to the literature (10.8 %) primarily consisting of transient neurological impairments (9.0 %) which all were fully reversible by conservative treatment. Poor outcome was seen in 1.7 % of the patients. Delay of surgical treatment had no influence on rates of open surgery (p = 0.662), complications (p = 0.365) or poor outcome (p = 0.942).
Conclusions
In this retrospective study delay of treatment of SCHF did not have significant influence on the incidence of open reduction, complications, and outcome. Therefore, in SCHF with sufficient blood perfusion and nerve function, elective treatment is reasonable to avoid surgical interventions in the middle of the night which are stressful and wearing both for patients and for surgeons.
Level of evidence
III (retrospective comparative study).
Similar content being viewed by others
References
Beaty JH (2003) Elbow fractures in children and adolescents. Instr Course Lect 52:661–665
Houshian S, Mehdi B, Larsen MS (2001) The epidemiology of elbow fracture in children: analysis of 355 fractures, with special reference to supracondylar humerus fractures. J Orthop Sci 6(4):312–315. doi:10.1007/s0077610060312
Otsuka NY, Kasser JR (1997) Supracondylar Fractures of the Humerus in Children. J Am Acad Orthop Surg 5(1):19–26
Cheng JC, Lam TP, Shen WY (1995) Closed reduction and percutaneous pinning for type III displaced supracondylar fractures of the humerus in children. J Orthop Trauma 9(6):511–515
Omid R, Choi PD, Skaggs DL (2008) Supracondylar humeral fractures in children. J Bone Joint Surg Am 90(5):1121–1132. doi:10.2106/JBJS.G.01354
Pirone AM, Graham HK, Krajbich JI (1988) Management of displaced extension-type supracondylar fractures of the humerus in children. J Bone Joint Surg Am 70(5):641–650
Ponce BA, Hedequist DJ, Zurakowski D, Atkinson CC, Waters PM (2004) Complications and timing of follow-up after closed reduction and percutaneous pinning of supracondylar humerus fractures: follow-up after percutaneous pinning of supracondylar humerus fractures. J Pediatr Orthop 24(6):610–614 00004694-200411000-00002 [pii]
Reynolds RA, Jackson H (2005) Concept of treatment in supracondylar humeral fractures. Injury 36(Suppl 1):A51–A56. doi:10.1016/j.injury.2004.12.013
Colaris JW, Horn TM, van den Ende ED, Allema JH, Merkus JW (2008) Supracondylar fractures of the humerus in children. Comparison of results in two treatment periods. Acta Chir Belg 108(6):715–719
von Laer L, Gunter SM, Knopf S, Weinberg AM (2002) Supracondylar humerus fracture in childhood—an efficacy study. Results of a multicenter study by the Pediatric Traumatology Section of the German Society of Trauma Surgery–II: costs and effectiveness of the treatment. Unfallchirurg 105(3):217–223
Weinberg AM, Marzi I, Gunter SM, Wessel L, Riedel J, von Laer L (2002) Supracondylar humerus fracture in childhood—an efficacy study. Results of a multicenter study by the Pediatric Traumatology Section of the German Society of Trauma Surgery–I: epidemiology, effectiveness evaluation and classification. Unfallchirurg 105(3):208–216
Yildirim AO, Unal VS, Oken OF, Gulcek M, Ozsular M, Ucaner A (2009) Timing of surgical treatment for type III supracondylar humerus fractures in pediatric patients. J Child Orthop 3(4):265–269. doi:10.1007/s11832-009-0189-2
Bales JG, Spencer HT, Wong MA, Fong YJ, Zionts LE, Silva M (2010) The effects of surgical delay on the outcome of pediatric supracondylar humeral fractures. J Pediatr Orthop 30(8):785–791. doi:10.1097/BPO.0b013e3181f9fc03
Farley FA, Patel P, Craig CL, Blakemore LC, Hensinger RN, Zhang L, Caird MS (2008) Pediatric supracondylar humerus fractures: treatment by type of orthopedic surgeon. J Child Orthop 2(2):91–95. doi:10.1007/s11832-008-0089-x
O’Hara LJ, Barlow JW, Clarke NM (2000) Displaced supracondylar fractures of the humerus in children. Audit changes practice. J Bone Joint Surg Br 82(2):204–210
Giannini S, Maffei G, Girolami M, Ceccarelli F (1983) The treatment of supracondylar fractures of the humerus in children by closed reduction and fixation with percutaneous Kirschner wires. Ital J Orthop Traumatol 9(2):181–188
Jacobs RL (1967) Supracondylar fracture of the humerus in children. IMJ Ill Med J 132(5):696–701
Minkowitz B, Busch MT (1994) Supracondylar humerus fractures. Current trends and controversies. Orthop Clin North Am 25(4):581–594
Paradis G, Lavallee P, Gagnon N, Lemire L (1993) Supracondylar fractures of the humerus in children. Technique and results of crossed percutaneous K-wire fixation. Clin Orthop Relat Res 297:231–237
Segal D (1979) Pediatric orthopedic emergencies. Pediatr Clin North Am 26(4):793–802
Walmsley PJ, Kelly MB, Robb JE, Annan IH, Porter DE (2006) Delay increases the need for open reduction of type-III supracondylar fractures of the humerus. J Bone Joint Surg Br 88(4):528–530. doi:10.1302/0301-620X.88B4.17491
Ramachandran M, Skaggs DL, Crawford HA, Eastwood DM, Lalonde FD, Vitale MG, Do TT, Kay RM (2008) Delaying treatment of supracondylar fractures in children: has the pendulum swung too far? J Bone Joint Surg Br 90(9):1228–1233. doi:10.1302/0301-620X.90B9.20728
Keon-Cohen BT (1966) Fractures at the elbow. J Bone Joint Surg Am 48(8):1623–1639
Loizou CL, Simillis C, Hutchinson JR (2009) A systematic review of early versus delayed treatment for type III supracondylar humeral fractures in children. Injury 40(3):245–248. doi:10.1016/j.injury.2008.07.031
Carmichael KD, Joyner K (2006) Quality of reduction versus timing of surgical intervention for pediatric supracondylar humerus fractures. Orthopedics 29(7):628–632
Leet AI, Frisancho J, Ebramzadeh E (2002) Delayed treatment of type 3 supracondylar humerus fractures in children. J Pediatr Orthop 22(2):203–207
Iyengar SR, Hoffinger SA, Townsend DR (1999) Early versus delayed reduction and pinning of type III displaced supracondylar fractures of the humerus in children: a comparative study. J Orthop Trauma 13(1):51–55
Mehlman CT, Strub WM, Roy DR, Wall EJ, Crawford AH (2001) The effect of surgical timing on the perioperative complications of treatment of supracondylar humeral fractures in children. J Bone Joint Surg Am 83-A(3):323–327
Gupta N, Kay RM, Leitch K, Femino JD, Tolo VT, Skaggs DL (2004) Effect of surgical delay on perioperative complications and need for open reduction in supracondylar humerus fractures in children. J Pediatr Orthop 24(3):245–248 00004694-200405000-00001 [pii]
Sibinski M, Sharma H, Bennet GC (2006) Early versus delayed treatment of extension type-3 supracondylar fractures of the humerus in children. J Bone Joint Surg Br 88(3):380–381. doi:10.1302/0301-620X.88B3.17181
Garg S, Weller A, Larson AN, Fletcher ND, Kwon M, Schiller J, Browne R, Copley L, Ho C (2014) Clinical characteristics of severe supracondylar humerus fractures in children. J Pediatr Orthop 34(1):34–39. doi:10.1097/BPO.0b013e31829c0046
Kronner JM Jr, Legakis JE, Kovacevic N, Thomas RL, Reynolds RA, Jones ET (2013) An evaluation of supracondylar humerus fractures: is there a correlation between postponing treatment and the need for open surgical intervention? J Child Orthop 7(2):131–137. doi:10.1007/s11832-013-0482-y
Larson AN, Garg S, Weller A, Fletcher ND, Schiller JR, Kwon M, Browne R, Copley LA, Ho CA (2014) Operative treatment of type II supracondylar humerus fractures: does time to surgery affect complications? J Pediatr Orthop 34(4):382–387. doi:10.1097/bpo.0000000000000124
Mayne AI, Perry DC, Bruce CE (2014) Delayed surgery in displaced paediatric supracondylar fractures: a safe approach? Results from a large UK tertiary paediatric trauma centre. Eur J Orthop Surg Traumatol Orthop Traumatol 24(7):1107–1110. doi:10.1007/s00590-013-1292-0
Murnaghan ML, Slobogean BL, Byrne A, Tredwell SJ, Mulpuri K (2010) The effect of surgical timing on operative duration and quality of reduction in Type III supracondylar humeral fractures in children. J Child Orthop 4(2):153–158. doi:10.1007/s11832-010-0240-3
Chacko AT, Ramirez MA, Ramappa AJ, Richardson LC, Appleton PT, Rodriguez EK (2011) Does late night hip surgery affect outcome? J Trauma 71(2):447–453. doi:10.1097/TA.0b013e3182231ad7 (Discussion 453)
Eastridge BJ, Hamilton EC, O’Keefe GE, Rege RV, Valentine RJ, Jones DJ, Tesfay S, Thal ER (2003) Effect of sleep deprivation on the performance of simulated laparoscopic surgical skill. Am J Surg 186(2):169–174
Kelz RR, Freeman KM, Hosokawa PW, Asch DA, Spitz FR, Moskowitz M, Henderson WG, Mitchell ME, Itani KM (2008) Time of day is associated with postoperative morbidity: an analysis of the national surgical quality improvement program data. Ann Surg 247(3):544–552. doi:10.1097/SLA.0b013e31815d7434
Ricci WM, Gallagher B, Brandt A, Schwappach J, Tucker M, Leighton R (2009) Is after-hours orthopaedic surgery associated with adverse outcomes? A prospective comparative study. J Bone Joint Surg Am 91(9):2067–2072. doi:10.2106/JBJS.H.00661
Rothschild JM, Keohane CA, Rogers S, Gardner R, Lipsitz SR, Salzberg CA, Yu T, Yoon CS, Williams DH, Wien MF, Czeisler CA, Bates DW, Landrigan CP (2009) Risks of complications by attending physicians after performing nighttime procedures. JAMA 302(14):1565–1572. doi:10.1001/jama.2009.1423
Gartland JJ (1959) Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet 109(2):145–154
Slongo T, Schmid T, Wilkins K, Joeris A (2008) Lateral external fixation—a new surgical technique for displaced unreducible supracondylar humeral fractures in children. J Bone Joint Surg Am 90(8):1690–1697. doi:10.2106/JBJS.G.00528
Flynn JC, Matthews JG, Benoit RL (1974) Blind pinning of displaced supracondylar fractures of the humerus in children. Sixteen years’ experience with long-term follow-up. J Bone Joint Surg Am 56(2):263–272
Baumann E (1960) Zur Behandlung der Knochenbrüche am Ellbogengelenk. Langenbecks Arch Chir 295(1):300–304
Cashman JP, Guerin SM, Hemsing M, McCormack D (2010) Effect of deferred treatment of supracondylar humeral fractures. Surgeon 8(2):71–73. doi:10.1016/j.surge.2009.10.011
Silva M, Wong TC, Bernthal NM (2011) Outcomes of reduction more than 7 days after injury in supracondylar humeral fractures in children. J Pediatr Orthop 31(7):751–756. doi:10.1097/BPO.0b013e31822f16e5
Kang S, Kam M, Miraj F, Park SS (2015) The prognostic value of the fracture level in the treatment of Gartland type III supracondylar humeral fracture in children. Bone Joint J 97-B(1):134–140. doi:10.1302/0301-620x.97b1.34492
Baumann E (1965) Spezielle Frakturen-und Luxationslehre: Ellbogen/Bearb. von Ernst Baumann. Thieme, Stuttgart
Lagrange J, Rigault P (1962) Les fractures de l’extrémité inférieure de l’humérus de l’enfant. Rev Chir Orthop 48:334–414
Slongo TF, Audige L (2007) Fracture and dislocation classification compendium for children: the AO pediatric comprehensive classification of long bone fractures (PCCF). J Orthop Trauma 21(10 Suppl):S135–S160 00005131-200711101-00020 [pii]
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Schmid, T., Joeris, A., Slongo, T. et al. Displaced supracondylar humeral fractures: influence of delay of surgery on the incidence of open reduction, complications and outcome. Arch Orthop Trauma Surg 135, 963–969 (2015). https://doi.org/10.1007/s00402-015-2248-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-015-2248-0