Abstract
Introduction
Ionising radiation is a potential risk for potentially exposed personnel. Only a few studies have examined the factors contributing to the emission of radiation in orthopaedic trauma procedures. We hypothesize that the experience of the surgeon and the fracture type influence the emission of radiation intraoperatively.
Methods
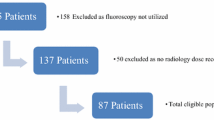
In a retrospective analysis, we examined 100 consecutive distal radius fractures receiving a volar plate osteosynthesis. The following parameters were documented: demographic data, plate system, fracture type, duration of the surgical procedure and duration of the emission of radiation, the experience level of the surgeon and the first assisting surgeon.
Results
Of all included patients (74 female), 48 had a type A, 7 a type B and 45 a type C fracture. The duration of radiation was longer for type C fractures [1.04 min (min)] in comparison to type A fractures (0.88 min) (P = 0.8152). In the type C subgroup, the highest amount of radiation was required for type C3 fractures (1.6 min), which was significantly more in comparison to type A (P = 0.0460) and type C1 fractures (P = 0.0089). The intraoperative emission of radiation (P = 0.00141) and the procedure time (P = 0.0006) depended on the experience of the surgical team.
Conclusion
The emission of radiation during this procedure depends on the fracture type and the experience of the surgical team. Operating theatre personnel should be aware of the higher emission rates during the treatment of type C fractures and in teaching hospitals with inexperienced team members.





Similar content being viewed by others
References
Herscovici D Jr, Sanders RW (2000) The effects, risks, and guidelines for radiation use in orthopaedic surgery. Clin Orthop Relat Res 375:126–132
Land CE (1980) Estimating cancer risks from low doses of ionizing radiation. Science 209:1197–1203
Nekolla EA, Griebel J, Brix G (2010) Radiation hygiene in medical X-ray imaging. Part 3: radiation exposure of patients and risk assessment. Radiologe 50:1039–1052
Buchanan GL, Chieffo A, Mehilli J et al (2012) The occupational effects of interventional cardiology: results from the WIN for Safety survey. EuroIntervention 8:658–663
Sasaki M, Cousins C, Miller DL et al (2013) ICRP publication 120: radiological protection in cardiology. Ann ICRP 42:1–125
Gebhard FT, Kraus MD, Schneider E et al (2006) Does computer-assisted spine surgery reduce intraoperative radiation doses? Spine (Phila Pa 1976) 31:2024–2027
Izadpanah K, Konrad G, Sudkamp NP, Oberst M (2009) Computer navigation in balloon kyphoplasty reduces the intraoperative radiation exposure. Spine (Phila Pa 1976) 34:1325–1329
Jones DP, Robertson PA, Lunt B, Jackson SA (2000) Radiation exposure during fluoroscopically assisted pedicle screw insertion in the lumbar spine. Spine (Phila Pa 1976) 25:1538–1541
Kim CW, Lee YP, Taylor W, Oygar A, Kim WK (2008) Use of navigation-assisted fluoroscopy to decrease radiation exposure during minimally invasive spine surgery. Spine J 8:584–590
Kosmopoulos V, Schizas C (2007) Pedicle screw placement accuracy: a meta-analysis. Spine (Phila Pa 1976) 32:E111–E120
Kraus MD, Krischak G, Keppler P, Gebhard FT, Schuetz UH (2010) Can computer-assisted surgery reduce the effective dose for spinal fusion and sacroiliac screw insertion? Clin Orthop Relat Res 468:2419–2429
Rampersaud YR, Foley KT, Shen AC, Williams S, Solomito M (2000) Radiation exposure to the spine surgeon during fluoroscopically assisted pedicle screw insertion. Spine (Phila Pa 1976) 25:2637–2645
Nellans KW, Kowalski E, Chung KC (2012) The epidemiology of distal radius fractures. Hand Clin 28:113–125
Cui Z, Pan J, Yu B, Zhang K, Xiong X (2011) Internal versus external fixation for unstable distal radius fractures: an up-to-date meta-analysis. Int Orthop 35:1333–1341
Diaz-Garcia RJ, Oda T, Shauver MJ, Chung KC (2011) A systematic review of outcomes and complications of treating unstable distal radius fractures in the elderly. J Hand Surg Am 36:824–835
Downing ND, Karantana A (2008) A revolution in the management of fractures of the distal radius? J Bone Jt Surg Br 90:1271–1275
Thomas KE, Parnell-Parmley JE, Haidar S et al (2006) Assessment of radiation dose awareness among pediatricians. Pediatr Radiol 36:823–832
Mastrangelo G, Fedeli U, Fadda E et al (2005) Increased cancer risk among surgeons in an orthopaedic hospital. Occup Med (Lond) 55:498–500
Smith GL, Briggs TW, Lavy CB, Nordeen H (1992) Ionising radiation: are orthopaedic surgeons at risk? Ann R Coll Surg Engl 74:326–328
Oddy MJ, Aldam CH (2006) Ionising radiation exposure to orthopaedic trainees: the effect of sub-specialty training. Ann R Coll Surg Engl 88:297–301
Kraus R, Pavlidis T, Szalay G, Meyer C, Schnettler R (2007) Elastic stable intramedullary nailing (ESIN) in pediatric forearm shaft fractures: intraoperative image intensifier times. Z Orthop Unfall 145:195–198
Fuchs M, Schmid A, Eiteljorge T, Modler M, Sturmer KM (1998) Exposure of the surgeon to radiation during surgery. Int Orthop 22:153–156
Barry TP (1984) Radiation exposure to an orthopedic surgeon. Clin Orthop Relat Res 182:160–164
Giordano BD, Grauer JN, Miller CP, Morgan TL, Rechtine GR (2011) Radiation exposure issues in orthopaedics. J Bone Jt Surg Am 93(12):e69(1–10)
Acknowledgments
No author of this article, their immediate family, and any research foundation with which they are affiliated did receive any financial payment or other benefit from any commercial entity related to the subject of this article.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kraus, M., Röderer, G., Max, M. et al. Influence of fracture type and surgeon experience on the emission of radiation in distal radius fractures. Arch Orthop Trauma Surg 133, 941–946 (2013). https://doi.org/10.1007/s00402-013-1739-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00402-013-1739-0