Abstract
Purpose
Colorectal cancer patients are commonly considered a single entity in outcomes studies. This is particularly true for quality of life (QOL) studies. This study aims to compare oncologic and QOL outcomes between right colon, left colon, and rectal cancer in patients operated on in a single high-volume institution.
Methods
A prospectively maintained database was queried to identify patients with pathological stages I–III colorectal adenocarcinoma electively operated on with curative intent between 2000 and 2010. Patient characteristics, perioperative and oncologic outcomes, and QOL were compared according to cancer location.
Results
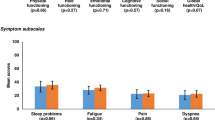
Two-thousand sixty-five (606 right colon cancer [RCC], 366 left colon cancer [LCC], and 1093 rectal cancer [RC]) patients met the inclusion criteria. LCC had better overall survival (OS) and disease-free survival (DFS) in the non-adjusted analysis (p < 0.001) and better OS in multivariate analysis adjusted by age, gender, ASA, chemotherapy, and pathological stage (p = 0.024). Although RCC had worse OS and DFS in non-adjusted survival analysis than LCC and RC, when adjusted for the factors above, RCC had better survival outcomes than RC, but not LCC. COX regression analysis showed age (p < 0.001), gender (p = 0.016), ASA (p < 0.001), pathological stage (p < 0.001), adjuvant chemotherapy (p = 0.043), and cancer location (p = 0.024) were independently associated with OS. Age (p < 0.001), gender (p = 0.030), ASA (p = 0.004), and pathological stage (p < 0.001) were independently associated with DFS. Patients with RC reported more sexual dysfunction and work restrictions than colon cancers (p = 0.015 and p < 0.001, respectively).
Conclusion
In an adjusted multivariate analysis, colon cancers demonstrated better survival outcomes when compared to rectal cancers.


Similar content being viewed by others
References
Siegel RL, Miller KD, Fuchs HE, Jemal A (2021) Cancer statistics, 2021. CA Cancer J Clin 71(1):7–33. https://doi.org/10.3322/caac.21654
Brenner H, Kloor M, Pox CP (2014) Colorectal cancer. Lancet 383(9927):1490–1502. https://doi.org/10.1016/s0140-6736(13)61649-9
Vogel JD, Eskicioglu C, Weiser MR, Feingold DL, Steele SR (2017) The American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of colon cancer. Dis Colon Rectum 60(10):999–1017. https://doi.org/10.1097/dcr.0000000000000926
Monson JR, Weiser MR, Buie WD, Chang GJ, Rafferty JF, Buie WD et al (2013) Practice parameters for the management of rectal cancer (revised). Dis Colon Rectum 56(5):535–550. https://doi.org/10.1097/DCR.0b013e31828cb66c
Lee GH, Malietzis G, Askari A, Bernardo D, Al-Hassi HO, Clark SK (2015) Is right-sided colon cancer different to left-sided colorectal cancer? — a systematic review. Eur J Surg Oncol 41(3):300–308. https://doi.org/10.1016/j.ejso.2014.11.001
Rosenberg R, Maak M, Schuster T, Becker K, Friess H, Gertler R (2010) Does a rectal cancer of the upper third behave more like a colon or a rectal cancer? Dis Colon Rectum 53(5):761–770. https://doi.org/10.1007/DCR.0b013e3181cdb25a
Lopez-Kostner F, Lavery IC, Hool GR, Rybicki LA, Fazio VW (1998) Total mesorectal excision is not necessary for cancers of the upper rectum. Surgery 124(4):612–7. discussion 7–8. https://doi.org/10.1067/msy.1998.91361
Heald RJ, Ryall RD (1986) Recurrence and survival after total mesorectal excision for rectal cancer. Lancet 1(8496):1479–1482. https://doi.org/10.1016/s0140-6736(86)91510-2
West NP, Anderin C, Smith KJ, Holm T, Quirke P (2010) Multicentre experience with extralevator abdominoperineal excision for low rectal cancer. Br J Surg 97(4):588–599. https://doi.org/10.1002/bjs.6916
Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T et al (2001) Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med 345(9):638–646. https://doi.org/10.1056/NEJMoa010580
Maeda K, Koide Y, Katsuno H (2014) When is local excision appropriate for “early” rectal cancer? Surg Today 44(11):2000–2014. https://doi.org/10.1007/s00595-013-0766-3
Hohenberger W, Weber K, Matzel K, Papadopoulos T, Merkel S (2009) Standardized surgery for colonic cancer: complete mesocolic excision and central ligation—technical notes and outcome. Colorectal Dis 11(4):354–64. discussion 64–5. https://doi.org/10.1111/j.1463-1318.2008.01735.x
Renouf DJ, Woods R, Speers C, Hay J, Phang PT, Fitzgerald C et al (2013) Improvements in 5-year outcomes of stage II/III rectal cancer relative to colon cancer. Am J Clin Oncol 36(6):558–564. https://doi.org/10.1097/COC.0b013e318256f5dc
Steele SR, Chang GJ, Hendren S, Weiser M, Irani J, Buie WD et al (2015) Practice guideline for the surveillance of patients after curative treatment of colon and rectal cancer. Dis Colon Rectum 58(8):713–725. https://doi.org/10.1097/dcr.0000000000000410
Fazio VW, O'Riordain MG, Lavery IC, Church JM, Lau P, Strong SA et al (1999) Long-term functional outcome and quality of life after stapled restorative proctocolectomy. Ann Surg 230(4):575–84. discussion 84–6. https://doi.org/10.1097/00000658-199910000-00013
Kalady MF, Sanchez JA, Manilich E, Hammel J, Casey G, Church JM (2009) Divergent oncogenic changes influence survival differences between colon and rectal adenocarcinomas. Dis Colon Rectum 52(6):1039–1045. https://doi.org/10.1007/DCR.0b013e31819edbd4
Chouhan H, Ferrandon S, DeVecchio J, Kalady MF, Church JM (2019) A changing spectrum of colorectal cancer biology with age: implications for the young patient. Dis Colon Rectum 62(1):21–26. https://doi.org/10.1097/dcr.0000000000001188
Yahagi M, Okabayashi K, Hasegawa H, Tsuruta M, Kitagawa Y (2016) The worse prognosis of right-sided compared with left-sided colon cancers: a systematic review and meta-analysis. J Gastrointest Surg 20(3):648–655. https://doi.org/10.1007/s11605-015-3026-6
Mukund K, Syulyukina N, Ramamoorthy S, Subramaniam S (2020) Right and left-sided colon cancers — specificity of molecular mechanisms in tumorigenesis and progression. BMC Cancer 20(1):317. https://doi.org/10.1186/s12885-020-06784-7
How P, Shihab O, Tekkis P, Brown G, Quirke P, Heald R et al (2011) A systematic review of cancer related patient outcomes after anterior resection and abdominoperineal excision for rectal cancer in the total mesorectal excision era. Surg Oncol 20(4):e149–e155. https://doi.org/10.1016/j.suronc.2011.05.001
Cedermark B, Dahlberg M, Glimelius B, Påhlman L, Rutqvist LE, Wilking N (1997) Improved survival with preoperative radiotherapy in resectable rectal cancer. N Engl J Med 336(14):980–987. https://doi.org/10.1056/nejm199704033361402
Kalady MF, de Campos-Lobato LF, Stocchi L, Geisler DP, Dietz D, Lavery IC et al (2009) Predictive factors of pathologic complete response after neoadjuvant chemoradiation for rectal cancer. Ann Surg 250(4):582–589. https://doi.org/10.1097/SLA.0b013e3181b91e63
Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R et al (2004) Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 351(17):1731–1740. https://doi.org/10.1056/NEJMoa040694
Fischer J, Hellmich G, Jackisch T, Puffer E, Zimmer J, Bleyl D et al (2015) Outcome for stage II and III rectal and colon cancer equally good after treatment improvement over three decades. Int J Colorectal Dis 30(6):797–806. https://doi.org/10.1007/s00384-015-2219-5
Liu S, Jiang T, Xiao L, Yang S, Liu Q, Gao Y et al (2021) Total neoadjuvant therapy (TNT) versus standard neoadjuvant chemoradiotherapy for locally advanced rectal cancer: a systematic review and meta-analysis. Oncologist 26(9):e1555–e1566. https://doi.org/10.1002/onco.13824
Brouwer NPM, Bos A, Lemmens V, Tanis PJ, Hugen N, Nagtegaal ID et al (2018) An overview of 25 years of incidence, treatment and outcome of colorectal cancer patients. Int J Cancer 143(11):2758–2766. https://doi.org/10.1002/ijc.31785
Fleshman J, Branda M, Sargent DJ, Boller AM, George V, Abbas M et al (2015) Effect of laparoscopic-assisted resection vs open resection of stage ii or iii rectal cancer on pathologic outcomes: the ACOSOG Z6051 randomized clinical trial. JAMA 314(13):1346–1355. https://doi.org/10.1001/jama.2015.10529
Stevenson AR, Solomon MJ, Lumley JW, Hewett P, Clouston AD, Gebski VJ et al (2015) Effect of laparoscopic-assisted resection vs open resection on pathological outcomes in rectal cancer: the ALaCaRT randomized clinical trial. JAMA 314(13):1356–1363. https://doi.org/10.1001/jama.2015.12009
Author information
Authors and Affiliations
Contributions
All authors have given substantial contributions to the conception, design, analysis, and interpretation of data for the work as well as drafting the work and final approval of the version to be published and are in agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Duraes, L.C., Steele, S.R., Valente, M.A. et al. Right colon, left colon, and rectal cancer have different oncologic and quality of life outcomes. Int J Colorectal Dis 37, 939–948 (2022). https://doi.org/10.1007/s00384-022-04121-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-022-04121-x