Abstract
Introduction
Sarcopenia is associated with outcomes in older-adults undergoing emergency surgery. Psoas major measurement is a surrogate marker of sarcopenia with multiple calculations existing normalising to body size and no consensus as to which is optimal. We compared three different psoas-major calculations to predict outcomes in older adults undergoing emergency laparotomy.
Methods
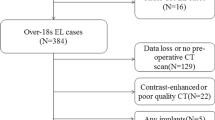
Consecutive over 65s were identified from the National Emergency Laparotomy Audit(NELA) database at a single centre between 2014 and 2018. Psoas major was measured at the L3 level and normalised to height (psoas muscle index, PMI), L3 vertebral body (psoas muscle:L3 ratio, PML3) or body surface area (psoas:body surface area, PBSA) and each correlated to outcomes. Outcome measures included inpatient, 30-day and 90-day mortality. A comparison of the three calculations was performed using the Mann-Whitney U, chi-squared, receiver operating characteristic curves (ROC) and binary logistic regression.
Results
Two hundred and sixty-four older adults underwent emergency laparotomy (median age, 75 years ((IQR, 70–81 years), 50% female)). Inpatient mortality was 19.6%, 30-day mortality was 15.1% and 90-day mortality was 18.5%. A total of 31.1% of males and 30% of females were sarcopenic (30.6% overall). A multivariate analysis confirmed each method of psoas major calculation (p < 0.0001) to be associated with mortality, as was ASA-grade (p < 0.0001). Area under the curve (AUC) was greatest for PML3 in predicting mortality (inpatient: PML3, 0.76; PMI, 0.71; PBSA, 0.70; 30-day: PML3, 0.74; PMI, 0.68; PBSA, 0.68; and 90-day: PML3, 0.78; PMI, 0.71; PBSA, 0.70). ASA-grade, P-POSSUM and PML3 were independently associated with mortality on multivariate analysis. ROC analysis of predictions from logistic regression models demonstrated PML3 to be more closely aligned to mortality than ASA or P-POSSUM (inpatient: AUC:PML3, 0.807; ASA, 0.783; P-POSSUM, 0.762; 30-day:AUC: PML3, 0.799; ASA, 0.784; P-POSSUM, 0.787; and 90-day: AUC:PML3, 0.805; ASA, 0.781; P-POSSUM, 0.756).
Conclusions
Sarcopenia was present in 30.6% of older adults undergoing emergency surgery and is associated with a significantly increased mortality. PML3 is superior to PMI or PBSA and should be considered the method of calculation of choice. Additionally, PML3 compares favourably to ASA and P-POSSUM.



Similar content being viewed by others
References
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F et al (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 39:412–423
Parmar KL, Law J, Carter B, Hewitt J, Boyle JM, Casey P et al (2019) Frailty in older patients undergoing emergency laparotomy: results from the UK observational emergency laparotomy and frailty (ELF) study. Ann Surg. https://doi.org/10.1097/SLA.0000000000003402
National Emergency Laparotomy Audit (NELA). Fourth Patient NELA report. https://www.nela.org.uk/reports (Accessed 3/10/2019)
Bouillon K, Kivimaki M, Hamer M, Sabia S, Fransson EI, Singh-Manoux A et al (2013) Measures of frailty in population-based studies: an overview. BMC Geriatr 13:64
Heymsfield SB, Gonzalez MC, Lu J, Jia G, Zheng J (2015 Nov) Skeletal muscle mass and quality: evolution of modern measurement concepts in the context of sarcopenia. Proc Nutr Soc 74(4):355–366
Lippi G, Sanchis-Gomar F, Montagnana M (2014) Biological markers in older people at risk of mobility limitations. Curr Pharm Des 20(19):3222–3244
Rutten IJ, Ubachs J, Kruitwagen RF, Van Dijk DP, Beets-Tan RG, Massuger LF et al (2017) The influence of sarcopenia on survival and surgical complications in ovarian cancer patients undergoing primary debulking surgery. Eur J Surg Oncol 43(4):717–724
Cooper Z, Scott JW, Rosenthal RA, Mitchell SL (2015) Emergency major abdominal surgical procedures in older adults: a systematic review of mortality and functional outcomes. J Am Geriatr Soc 63(12):2563–2571
Hawkins RB, Mehaffey JH, Charles EJ, Kern JA, Lim DS, Teman NR et al (2018) Psoas muscle size predicts risk-adjusted outcomes after surgical aortic valve replacement. Ann Thorac Surg
Paknikar R, Friedman J, Cron D, Deeb GM, Chetcuti S, Grossman PM, Wang S, Englesbe M, Patel HJ (2016) Psoas muscle size as a frailty measure for open and transcatheter aortic valve replacement. J Thorac Cardiovasc Surg 151(3):745–751
Jones KI, Doleman B, Scott S, Lund JN, Williams JP (2015) Simple psoas cross-sectional area measurement is a quick and easy method to assess sarcopenia and predicts major surgical complications. Color Dis 1:O20–O26
Drudi LM, Phung K, Ades M, Zuckerman J, Mullie L, Steinmetz OK, Obrand DI, Afilalo J (2016) Psoas muscle area predicts all- cause mortality after endovascular and open aortic aneurysm repair. Eur J Vasc Endovasc Surg 52:764–769
Yoshikawa T, Takano M, Miyamoto M, Yajima I, Shimizu Y, Aizawa Y, Suguchi Y, Moriiwa M, Aoyama T, Soyama H, Goto T, Hirata J, Suzuki A, Sasa H, Nagaoka I, Tsuda H, Furuya K (2017) Psoas muscle volume as a predictor of peripheral neurotoxicity induced by primary chemotherapy in ovarian cancers. Cancer Chemother Pharmacol 80(3):555–561
Gomibuchi T, Seto T, Komatsu M, Tanaka H, Ichimura H, Yamamoto T, Ohashi N, Wada Y, Okada K (2018) Impact of frailty on outcomes in acute type a aortic dissection. Ann Thorac Surg 106(5):1349–1355
Liu J, Motoyama S, Sato Y, Wakita A, Kawakita Y, Saito H, Minamiya Y (2016) Decreased skeletal muscle mass after neoadjuvant therapy correlates with poor prognosis in patients with esophageal cancer. Anticancer Res 36(12):6677–6685
Nyers ES, Brothers TE (2017) Perioperative psoas to lumbar vertebral index does not successfully predict amputation-free survival after lower extremity revascularization. J Vasc Surg 66(6):1820–1825
Simpson G, Parker A, Hopley P, Wilson J, Magee C (2018) Pre-operative psoas major measurement compared to P-POSSUM as a prognostic indicator in over-80s undergoing emergency laparotomy. Eur J Trauma Emerg Surg 13
Dirks RC, Edwards BL, Tong E, Schaheen B, Turrentine FE, Shada A, Smith PW (2017) Sarcopenia in emergency abdominal surgery. J Surg Res 207:13–21
Rangel EL, Rios-Diaz AJ, Uyeda JW, Castillo-Angeles M, Cooper Z, Olufajo OA, Salim A, Sodickson AD (2017) Sarcopenia increases risk of long-term mortality in elderly patients undergoing emergency abdominal surgery. J Trauma Acute Care Surg 83(6):1179–1186
Hajibandeh S, Hajibandeh S, Jarvis R, Bhogal T, Dalmia S (2018) Meta-analysis of the effect of sarcopenia in predicting postoperative mortality in emergency and elective abdominal surgery. Surgeon
Du Y, Karvellas CJ, Baracos V, Williams DC, Khadaroo RG (2014) Acute Care and Emergency Surgery (ACES) group. Sarcopenia is a predictor of outcomes in very elderly patients undergoing emergency surgery. Surgery. 156(3):521–527
Brandt E, Tengberg LT, Bay-Nielsen M (2019) Sarcopenia predicts 90-day mortality in elderly patients undergoing emergency abdominal surgery. Abdom Radiol 44(3):1155–1160
Living longer: how our population is changing and why it matters. The Office of National Statistics. https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/ageing/articles/livinglongerhowourpopulationischangingandwhyitmatters/2018-08-13 (accessed 27/08/19)
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Simpson, G., Manu, N., Magee, C. et al. Measuring sarcopenia on pre-operative CT in older adults undergoing emergency laparotomy: a comparison of three different calculations. Int J Colorectal Dis 35, 1095–1102 (2020). https://doi.org/10.1007/s00384-020-03570-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-020-03570-6