Abstract
Purpose
The purpose of this study is to create a new risk nomogram to predict perioperative major adverse cardiac events in patients undergoing colorectal carcinoma surgery.
Methods
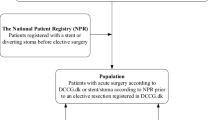
A total of 1899 patients who underwent colorectal carcinoma surgery at a tertiary teaching hospital in China between 2007 and 2012 were recruited. Logistic regression analysis was used to define risk factors for major adverse cardiac events. A nomogram-predicting model was built based on the logistic regression model and discrimination was tested by receiver operating characteristic curves.
Results
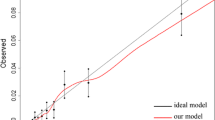
Fifty-six (2.9%) among 1899 included patients developed at least one cardiac event. Eight risk factors were found in the multivariate logistic regression model, which included age ≥60 years, smoking, a history of chronic kidney disease, coronary artery disease, congestive heart failure, hypertension, preoperative albumin levels ≤35 g/L, blood transfusion ≥500 mL, and intraoperative blood pressure variability. P = 0.708 in the Hosmer–Lemeshow test indicated acceptable calibration power. Based on this multivariate model, we built a risk nomogram model for these cardiac events with an area under the curve (95% confidence interval) of 0.923 (0.889, 0.957), which demonstrated good discrimination of this model. When the probability cutoff was 1.9% (total score of 83), the nomogram model had the best sensitivity and specificity in predicting cardiac events.
Conclusions
A new nomogram model for predicting perioperative major adverse cardiac events in patients who had colorectal carcinoma surgery was established in this study. When the total score is >83, patients undergoing colorectal carcinoma surgery should be considered at high risk of perioperative major adverse cardiac events.




Similar content being viewed by others
Change history
23 June 2018
On this article the authors requested to add another affiliation which is Key Laboratory on Assisted Circulation, Ministry of Health, Guangzhou 510,080, China for Juhong Zhang, Xiuren Gao and Zhibin Huang. The new affiliation is now added in this article. The remainder of the article remains unchanged.
References
England RS (2005) Aging China: the demographic challenge to China’s economic prospects. Praeger, Westport
Xu L, Yu C, Jiang J et al (2015) Major adverse cardiac events in elderly patients with coronary artery disease undergoing noncardiac surgery: a multicenter prospective study in China. Arch Gerontol Geriatr 61(3):503–509
Hanyuda A, Ogino S, Rong QZ et al (2016) Body mass index and risk of colorectal cancer according to tumor lymphocytic infiltrate. Int J Cancer 139(4):854–868
Kristensen SD, Knuuti J, Saraste A et al (2014) 2014 ESC/ESA guidelines on non-cardiac surgery: cardiovascular assessment and management: the joint task force on non-cardiac surgery: cardiovascular assessment and management of the European Society of Cardiology (ESC) and the European Society of Anaesthesiology (ESA). Eur Heart J 35(35):2383–2431
Causey MW, Maykel JA, Hatch Q, Miller S, Steele SR (2011) Identifying risk factors for renal failure and myocardial infarction following colorectal surgery. J Surg Res 170(1):32–37
Biccard BM, Rodseth RN (2013) What evidence is there for intraoperative predictors of perioperative cardiac outcomes? A systematic review. Perioper Med (Lond) 2(1):14
Cutlip DE, Windecker S, Mehran R et al (2007) Clinical end points in coronary stent trials: a case for standardized definitions. Circulation 115(17):2344–2351
Devereaux PJ, Goldman L, Yusuf S, Gilbert K, Leslie K, Guyatt GH (2005) Surveillance and prevention of major perioperative ischemic cardiac events in patients undergoing noncardiac surgery: a review. CMAJ 173(7):779–788
Zlotnik A, Abraira V (2015) A general-purpose nomogram generator for predictive logistic regression models. Stata J 15(2):537–546
Lu CX, Chen HL, Shen WQ, Feng LP (2017) A new nomogram score for predicting surgery-related pressure ulcers in cardiovascular surgical patients. Int Wound J 14(1):226–232
Fleisher LA, Fleischmann KE, Auerbach AD et al (2014) 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: executive summary: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 130(24):2215–2245
Kumar R, McKinney WP, Raj G et al (2001) Adverse cardiac events after surgery: assessing risk in a veteran population. J Gen Intern Med 16(8):507–518
Alcock RF, Kouzios D, Naoum C, Hillis GS, Brieger DB (2012) Perioperative myocardial necrosis in patients at high cardiovascular risk undergoing elective non-cardiac surgery. Heart 98(10):792–798
Freeman WK, Gibbons RJ (2009) Perioperative cardiovascular assessment of patients undergoing noncardiac surgery. Mayo Clin Proc 84(1):79–90
Pandey A, Sood A, Sammon JD et al (2015) Effect of preoperative angina pectoris on cardiac outcomes in patients with previous myocardial infarction undergoing major noncardiac surgery (data from ACS-NSQIP). Am J Cardiol 115(8):1080–1084
Hammill BG, Curtis LH, Bennett-Guerrero E et al (2008) Impact of heart failure on patients undergoing major noncardiac surgery. Anesthesiology 108(4):559–567
Goldman L, Caldera DL, Nussbaum SR et al (1977) Multifactorial index of cardiac risk in noncardiac surgical procedures. N Engl J Med 297(16):845–850
Lee TH, Marcantonio ER, Mangione CM et al (1999) Derivation and prospective validation of a simple index for prediction of cardiac risk of major noncardiac surgery. Circulation 100(10):1043–1049
Wang TY, Martin JR, Loriaux DB et al (2016) Risk assessment and characterization of 30-day perioperative myocardial infarction following spine surgery: a retrospective analysis of 1346 consecutive adult patients. Spine (Phila Pa 1976) 41(5):438–444
Ma J, Xin Q, Wang X, Gao M, Wang Y, Liu J (2015) Prediction of perioperative cardiac events through preoperative NT-pro-BNP and cTnI after emergent non-cardiac surgery in elderly patients. PLoS One 10(3):e0121306
Liu ZJ, Yu CH, Xu L, Han W, Jiang JM, Huang YG (2013) Risk factors for perioperative major cardiac events in Chinese elderly patients with coronary heart disease undergoing noncardiac surgery. Chin Med J 126(18):3464–3469
Charlson ME, MacKenzie CR, Gold JP et al (1989) The preoperative and intraoperative hemodynamic predictors of postoperative myocardial infarction or ischemia in patients undergoing noncardiac surgery. Ann Surg 210(5):637–648
Acknowledgements
We appreciate all medical record administators in our hospital for their help in data collecting. We also thank Peizhen Zhao, a junior statistician in the Department of Medical Statistics, College of Public Health, Sun Yat-sen University, for statistical assistance.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
This study has been approved by the Regional Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University and all patients have signed informed consent.
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Zhang, J., Xiao, Y., Yang, D. et al. Development of a new risk nomogram of perioperative major adverse cardiac events for Chinese patients undergoing colorectal carcinoma surgery. Int J Colorectal Dis 32, 1157–1164 (2017). https://doi.org/10.1007/s00384-017-2812-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00384-017-2812-x