Abstract
Purpose
Identifying at-risk children can provide a crucial opportunity for preventative measures to avoid opioid addiction. This study sought to determine at-risk pediatric patients that were previously hospitalized due to other causes prior to their opioid-related admission.
Methods
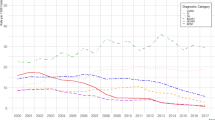
The Nationwide Readmissions Database (2010–2014) was queried for children 1–18 years old with an opioid-related hospitalization. Previous admissions (up to 1 year prior) and associated diagnoses were compared. Results were weighted for national estimates.
Results
51,349 opioid-related hospitalizations were identified with an overall in-hospital mortality of 0.8%. Seventeen percent had a previous admission during the same calendar year of which 44% had > 1 and 11% had ≥ 5 prior admissions. Only 4% of prior admissions occurred at a different hospital. Males and females were equally represented, and 82% were ≥ 13 years old. Only 16% of previously admitted patients underwent a major surgical procedure during a previous hospitalization. The most common concomitant diagnoses for patients with prior hospitalizations were drug abuse (37%), chronic pulmonary disease (18%), and depression (10%).
Conclusion
Opioid-related hospitalizations often occur among children with multiple recent admissions, usually to the same hospital. Most patients do not have a history of cancer or recent surgery to account for their opioid use.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Kolodny A, Courtwright DT, Hwang CS et al (2015) The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health 36:559–574. https://doi.org/10.1146/annurev-publhealth-031914-122957
Gaither JR, Leventhal JM, Ryan SA, Camenga DR (2016) National trends in hospitalizations for opioid poisonings among children and adolescents, 1997 to 2012. JAMA Pediatr 170:1195–1201. https://doi.org/10.1001/jamapediatrics.2016.2154
Harbaugh CM, Lee JS, Hu HM et al (2018) Persistent opioid use among pediatric patients after surgery. Pediatrics 141:e20172439. https://doi.org/10.1542/peds.2017-2439
Knipper E, Banta-Green CJ, Jimenez N (2017) Opioid use disorder and misuse: a review of the epidemiology and medical implications for pediatric anesthesiologists. Paediatr Anaesth 27:1070–1076. https://doi.org/10.1111/pan.13225
Tadros A, Layman SM, Davis SM et al (2016) Emergency department visits by pediatric patients for poisoning by prescription opioids. Am J Drug Alcohol Abuse 42:550–555. https://doi.org/10.1080/00952990.2016.1194851
Gaither JR, Shabanova V, Leventhal JM (2018) US national trends in pediatric deaths from prescription and illicit opioids, 1999–2016. JAMA Netw Open 1:e186558. https://doi.org/10.1001/jamanetworkopen.2018.6558
Kozlowski LJ, Kost-Byerly S, Colantuoni E et al (2014) Pain prevalence, intensity, assessment and management in a hospitalized pediatric population. Pain Manag Nurs 15:22–35. https://doi.org/10.1016/j.pmn.2012.04.003
American Academy of Pediatrics, Committee on Psychosocial Aspects of Child and Family Health, Task Force on Pain in Infants, Children, and Adolescents (2001) The assessment and management of acute pain in infants, children, and adolescents. Pediatrics 108:793–797. https://doi.org/10.1542/peds.108.3.793
McGrath PA (1996) Development of the World Health Organization guidelines on cancer pain relief and palliative care in children. J Pain Symptom Manage 12:87–92. https://doi.org/10.1016/0885-3924(96)00099-1
Friedrichsdorf SJ, Kang TI (2007) The management of pain in children with life-limiting illnesses. Pediatr Clin North Am 54(645–672):x. https://doi.org/10.1016/j.pcl.2007.07.007
Cravero JP, Agarwal R, Berde C et al (2019) The Society for Pediatric Anesthesia recommendations for the use of opioids in children during the perioperative period. Paediatr Anaesth 29:547–571. https://doi.org/10.1111/pan.13639
Van Cleve WC, Grigg EB (2017) Variability in opioid prescribing for children undergoing ambulatory surgery in the United States. J Clin Anesth 41:16–20. https://doi.org/10.1016/j.jclinane.2017.05.014
Denning N-L, Kvasnovsky C, Golden JM et al (2019) Inconsistency in opioid prescribing practices after pediatric ambulatory hernia surgery. J Surg Res 241:57–62. https://doi.org/10.1016/j.jss.2019.03.043
Corona LE, Roth EB, Thao A et al (2021) Opioid prescribing is excessive and variable after pediatric ambulatory urologic surgery. J Pediatr Urol 17:259.e1-259.e6. https://doi.org/10.1016/j.jpurol.2021.01.008
Dart RC, Surratt HL, Cicero TJ et al (2015) Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med 372:241–248. https://doi.org/10.1056/NEJMsa1406143
Manchikanti L, Fellows B, Ailinani H, Pampati V (2010) Therapeutic use, abuse, and nonmedical use of opioids: a ten-year perspective. Pain Physician 13:401–435
George JA, Park PS, Hunsberger J et al (2016) An Analysis of 34,218 pediatric outpatient controlled substance prescriptions. Anesth Analg 122:807–813. https://doi.org/10.1213/ANE.0000000000001081
Ahrari M, Ali S, Hartling L et al (2021) Nonmedical opioid use after short-term therapeutic exposure in children: a systematic review. Pediatrics 148:e2021051927. https://doi.org/10.1542/peds.2021-051927
Sun N, Steinberg BE, Faraoni D, Isaac L (2021) Variability in discharge opioid prescribing practices for children: a historical cohort study. Can J Anesth/J Can Anesth. https://doi.org/10.1007/s12630-021-02160-6
Miech R, Johnston L, O’Malley PM et al (2015) Prescription opioids in adolescence and future opioid misuse. Pediatrics 136:e1169–e1177. https://doi.org/10.1542/peds.2015-1364
McCabe SE, West BT, Boyd CJ (2013) Medical use, medical misuse, and nonmedical use of prescription opioids: results from a longitudinal study. Pain 154:708–713. https://doi.org/10.1016/j.pain.2013.01.011
Osborne V, Striley CW, Nixon SJ et al (2019) Sex differences in patterns of prescription opioid non-medical use among 10–18 year olds in the US. Addict Behav 89:163–171. https://doi.org/10.1016/j.addbeh.2018.10.009
McCabe SE, Veliz P, Schulenberg JE (2016) Adolescent context of exposure to prescription opioids and substance use disorder symptoms at age 35: a national longitudinal study. Pain 157:2173–2178. https://doi.org/10.1097/j.pain.0000000000000624
Overton HN, Hanna MN, Bruhn WE et al (2018) Opioid-prescribing guidelines for common surgical procedures: an expert panel consensus. J Am Coll Surg 227:411–418. https://doi.org/10.1016/j.jamcollsurg.2018.07.659
Rajbhandari-Thapa J, Zhang D, Padilla HM, Chung SR (2019) Opioid-related hospitalization and its association with chronic diseases: findings from the national inpatient sample, 2011–2015. Prev Chronic Dis 16:E157. https://doi.org/10.5888/pcd16.190169
NRD Overview. https://www.hcup-us.ahrq.gov/nrdoverview.jsp. Accessed 14 Oct 2021
Opioid Hospital Stays/Emergency Department Visits—HCUP Fast Stats. https://www.hcup-us.ahrq.gov/faststats/OpioidUseServlet. Accessed 14 Oct 2021
Gryczynski J, Nordeck CD, Welsh C et al (2021) Preventing hospital readmission for patients with comorbid substance use disorder. Ann Intern Med 174:899–909. https://doi.org/10.7326/M20-5475
Nordeck CD, Welsh C, Schwartz RP et al (2018) Rehospitalization and substance use disorder (SUD) treatment entry among patients seen by a hospital SUD consultation-liaison service. Drug Alcohol Depend 186:23–28. https://doi.org/10.1016/j.drugalcdep.2017.12.043
Welsh JW, Dennis ML, Funk R et al (2022) Trends and age-related disparities in opioid use disorder treatment admissions for adolescents and young adults. J Subst Abuse Treat 132:108584. https://doi.org/10.1016/j.jsat.2021.108584
Anderson KT, Bartz-Kurycki MA, Ferguson DM et al (2018) Too much of a bad thing: discharge opioid prescriptions in pediatric appendectomy patients. J Pediatr Surg 53:2374–2377. https://doi.org/10.1016/j.jpedsurg.2018.08.034
Cairo SB, Calabro KA, Bowdish E et al (2019) Variation in postoperative narcotic prescribing after pediatric appendectomy. J Pediatr Surg 54:1866–1871. https://doi.org/10.1016/j.jpedsurg.2018.11.015
Bedi P, Rai MP, Bumrah K et al (2021) Pattern and burden of opioid-related hospitalizations in the USA from 2016 to 2018. Br J Clin Pharmacol 87:4366–4374. https://doi.org/10.1111/bcp.14857
Wilson JD, Abebe KZ, Kraemer K et al (2021) Trajectories of opioid use following first opioid prescription in opioid-naive youths and young adults. JAMA Netw Open 4:e214552. https://doi.org/10.1001/jamanetworkopen.2021.4552
Cho J, Kelley-Quon LI, Barrington-Trimis JL et al (2021) Behavioral health risk factors for nonmedical prescription opioid use in adolescence. Pediatrics 148:e2021051451. https://doi.org/10.1542/peds.2021-051451
Edlund MJ, Forman-Hoffman VL, Winder CR et al (2015) Opioid abuse and depression in adolescents: results from the National Survey on Drug Use and Health. Drug Alcohol Depend 152:131–138. https://doi.org/10.1016/j.drugalcdep.2015.04.010
Valentine SL, Nadkarni VM, Curley MAQ, Pediatric Acute Lung Injury Consensus Conference Group (2015) Nonpulmonary treatments for pediatric acute respiratory distress syndrome: proceedings from the Pediatric Acute Lung Injury Consensus Conference. Pediatr Crit Care Med 16:S73-85. https://doi.org/10.1097/PCC.0000000000000435
Chidambaran V, Olbrecht V, Hossain M et al (2014) Risk predictors of opioid-induced critical respiratory events in children: naloxone use as a quality measure of opioid safety. Pain Med 15:2139–2149. https://doi.org/10.1111/pme.12575
Shanahan L, Hill SN, Bechtiger L et al (2021) Prevalence and childhood precursors of opioid use in the early decades of life. JAMA Pediatr 175:276–285. https://doi.org/10.1001/jamapediatrics.2020.5205
Acknowledgements
The authors would like to acknowledge all HCUP Data Partners contributing to HCUP, a list of which can be found at (https://www.hcup-us.ahrq.gov/db/hcupdatapartners.jsp). This research did not receive any specific grant from funding agencies in the public, commercial, or not for-profit sectors.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Study conception and design: AF, CTH, EAP, JES. Acquisition of data: AF, CTH, HJQ, KQ. Analysis and interpretation of data: CTH, HJQ, AF, CMT, JES, EAP, ACM. Drafting of manuscript: AF, CTH, HJQ, KQ, CMT, EAP, JES, ACM. Critical revision of manuscript: AF, CTH, CMT, EAP, JES.
Corresponding author
Ethics declarations
Conflict of interest
None.
Financial disclosures
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ferrantella, A., Huerta, C.T., Quinn, K. et al. Risk factors associated with recent opioid-related hospitalizations in children: a nationwide analysis. Pediatr Surg Int 38, 843–851 (2022). https://doi.org/10.1007/s00383-022-05088-0
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-022-05088-0