Abstract
Purpose
In infants and toddlers, gastrostomy tube placement (GT) is typically accompanied by consideration of concomitant Nissen fundoplication (NF). Historically, rates of NF have varied across providers and institutions. This study examines practice variation and longitudinal trends in NF at pediatric tertiary centers.
Methods
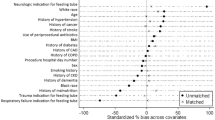
Patients ≤ 2 years who underwent GT between 2008 and 2018 were identified in the Pediatric Health Information System database. Patient demographics and rates of NF were examined. Descriptive statistics were used to evaluate the variation in the proportion of GT with NF at each hospital, by volume and over time.
Results
40,348 patients were identified across 40 hospitals. Most patients were male (53.8%), non-Hispanic white (49.5%) and publicly-insured (60.4%). Rates of NF by hospital varied significantly from 4.2 to 75.2% (p < 0.001), though were not associated with geographic region (p = 0.088). Rates of NF decreased from 42.8% in 2008 to 14.2% in 2018, with a mean annual rate of change of − 3.07% (95% CI − 3.53, − 2.61). This trend remained when stratifying hospitals into volume quartiles.
Conclusion
There is significant practice variation in performing NF. Regardless of volume, the rate of NF is also decreasing. Objective NF outcome measurements are needed to standardize the management of long-term enteral access in this population.






Similar content being viewed by others
References
Sømme S, Bronsert M, Morrato E, Ziegler M (2013) Frequency and variety of inpatient pediatric surgical procedures in the United States. Pediatrics 132(6):e1466–e1472. https://doi.org/10.1542/peds.2013-1243
Yoo BG, Yang HK, Lee YJ, Byun SY, Kim HY, Park JH (2014) Fundoplication in neonates and infants with primary gastroesophageal reflux. Pediatr Gastroenterol Hepatol Nutr 17(2):93–97. https://doi.org/10.5223/pghn.2014.17.2.93
Fonkalsrud EW, Ashcraft KW, Coran AG et al (1998) Surgical treatment of gastroesophageal reflux in children: a combined hospital study of 7467 patients. Pediatrics 101(3):419–422. https://doi.org/10.1542/peds.101.3.419
Kazerooni NL, VanCamp J, Hirschl RB, Drongowski RA, Coran AG (1994) Fundoplication in 160 children under 2 years of age. J Pediatr Surg 29(5):677–681. https://doi.org/10.1016/0022-3468(94)90739-0
Cullis PS, Siminas S, Losty PD (2020) Efficacy of antireflux surgery in children with or without neurological impairment: a systematic review. Br J Surg 107(6):636–646. https://doi.org/10.1002/bjs.11488
Goldin AB, Garrison M, Christakis D (2009) Variations between hospitals in antireflux procedures in children. Arch Pediatr Adolesc Med 163(7):658–663. https://doi.org/10.1001/archpediatrics.2009.103
Martin K, Deshaies C, Emil S (2014) Outcomes of pediatric laparoscopic fundoplication: a critical review of the literature. Can J Gastroenterol Hepatol 28(2):97–102. https://doi.org/10.1155/2014/738203
Short HL, Zhu W, McCracken C, Travers C, Waller LA, Raval MV (2017) Exploring regional variability in utilization of antireflux surgery in children. J Surg Res 214:49–56. https://doi.org/10.1016/j.jss.2017.02.075
Olson D, Birkholz M, Gaensbauer JT, Asturias EJ, Todd JK (2015) Analysis of the pediatric health information system database as a surveillance tool for travel-associated infectious diseases. Am J Trop Med Hyg 92(5):1067–1069. https://doi.org/10.4269/ajtmh.14-0794
Peltz A, Wu CL, White ML et al (2016) Characteristics of rural children admitted to pediatric hospitals. Pediatrics 137(5):e20153156. https://doi.org/10.1542/peds.2015-3156
Deans KJ, Cooper JN, Rangel SJ, Raval MV, Minneci PC, Moss RL (2014) Enhancing NSQIP-pediatric through integration with the pediatric health information system. J Pediatr Surg 49(1):207–212. https://doi.org/10.1016/j.jpedsurg.2013.09.058
Stey AM, Vinocur CD, Moss RL et al (2018) Hospital variation in rates of concurrent fundoplication during gastrostomy enteral access procedures. Surg Endosc 32(5):2201–2211. https://doi.org/10.1007/s00464-017-5518-9
Birkmeyer JD, Reames BN, McCulloch P, Carr AJ, Campbell WB, Wennberg JE (2013) Understanding of regional variation in the use of surgery. Lancet 382(9898):1121–1129. https://doi.org/10.1016/S0140-6736(13)61215-5
Weinstein JN, Bronner KK, Morgan TS, Wennberg JE (2004) Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff (Millwood) 23(Suppl 2):VAR81–VAR89. https://doi.org/10.1377/hlthaff.var.81
Goldin AB, Sawin R, Seidel KD, Flum DR (2006) Do antireflux operations decrease the rate of reflux-related hospitalizations in children? Pediatrics 118(6):2326–2333. https://doi.org/10.1542/peds.2006-2212
Horgan S, Pellegrini CA (1997) Surgical treatment of gastroesophageal reflux disease. Surg Clin North Am 77(5):1063–1082. https://doi.org/10.1016/s0039-6109(05)70605-8
Pascoe E, Falvey T, Jiwane A, Henry G, Krishnan U (2016) Outcomes of fundoplication for paediatric gastroesophageal reflux disease. Pediatr Surg Int 32(4):353–361. https://doi.org/10.1007/s00383-015-3843-4
Lee SL, Shabatian H, Hsu JW, Applebaum H, Haigh PI (2008) Hospital admissions for respiratory symptoms and failure to thrive before and after Nissen fundoplication. J Pediatr Surg 43(1):59–65. https://doi.org/10.1016/j.jpedsurg.2007.09.020
McCulloch P, Nagendran M, Campbell WB et al (2013) Strategies to reduce variation in the use of surgery. Lancet 382(9898):1130–1139. https://doi.org/10.1016/S0140-6736(13)61216-7
Shah M, Klooster M, Yanni G, Shah A (2010) Frequency and methods of gastrojejunal tube replacement in children. Curr Gastroenterol Rep 12(3):223–227. https://doi.org/10.1007/s11894-010-0107-2
Raval MV, Phillips JD (2006) Optimal enteral feeding in children with gastric dysfunction: surgical jejunostomy vs image-guided gastrojejunal tube placement. J Pediatr Surg 41(10):1679–1682. https://doi.org/10.1016/j.jpedsurg.2006.05.050
Massoumi RL, Abdelhafeez AH, Christensen MA et al (2016) Gastrojejunostomy tube bowel perforations in low-weight infants. JPEN J Parenter Enteral Nutr 40(8):1177–1182. https://doi.org/10.1177/0148607115575741
Godbole P, Margabanthu G, Crabbe DC et al (2002) Limitations and uses of gastrojejunal feeding tubes. Arch Dis Child 86(2):134–137. https://doi.org/10.1136/adc.86.2.134
Funding
The authors have no financial relationships relevant to this article to disclose. No funding was secured for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Table 2.
Rights and permissions
About this article
Cite this article
Bouchard, M.E., Stewart, D.H., Hall, M. et al. Trends in gastrostomy tube placement with concomitant Nissen fundoplication for infants and young children at Pediatric Tertiary Centers. Pediatr Surg Int 37, 617–625 (2021). https://doi.org/10.1007/s00383-020-04845-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-020-04845-3