Abstract
Purpose
To assess incidence and natural history of umbilical hernia following sutured and sutureless gastroschisis closure.
Methods
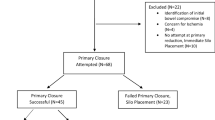
With audit approval, we undertook a retrospective clinical record review of all gastroschisis closures in our institution (2007–2013). Patient demographics, gastroschisis closure method and umbilical hernia occurrence were recorded. Data, presented as median (range), underwent appropriate statistical analysis.
Results
Fifty-three patients were identified, gestation 36 weeks (31–38), birth weight 2.39 kg (1–3.52) and 23 (43 %) were male. Fourteen patients (26 %) underwent sutureless closure: 12 primary, 2 staged; and 39 (74 %) sutured closure: 19 primary, 20 staged. Sutured closure was interrupted sutures in 24 patients, 11 pursestring and 4 not specified. Fifty patients were followed-up over 53 months (10–101) and 22 (44 %) developed umbilical hernias. There was a significantly greater hernia incidence following sutureless closure (p = 0.0002). In sutured closure, pursestring technique had the highest hernia rate (64 %). Seven patients underwent operative hernia closure; three secondary to another procedure. Seven patients had their hernias resolve. One patient was lost to follow-up and seven remain under observation with no reported complications.
Conclusions
There is a significant umbilical hernia incidence following sutureless and pursestring sutured gastroschisis closure. This has not led to complications and the majority have not undergone repair.

Similar content being viewed by others
References
Hoyme HE, Jones MC, Jones KL (1983) Gastroschisis: abdominal wall disruption secondary to early gestational interruption of the omphalomesenteric artery. Semin Perinatol 7:294–298
Kunz SN, Tieder JS, Whitlock K, Jackson JC, Avansino JR (2013) Primary fascial closure versus stage closure with silo in patients with gastroschisis. J Pediatr Surg 48:845–857
Allotey J, Davenport M, Njere I, Charlesworth P, Greenough A, Ade-Ajayi N, Patel S (2007) Benefit of pre-formed silos in the management of gastroschisis. Pediatr Surg Int 23(11):1065–1069
Sandler A, Lawrence J, Meehan J, Phearman L, Soper R (2004) A “plastic” sutureless abdominal wall closure in gastroschisis. J Pediatr Surg 39(5):738–741
Kimble RM, Singh SJ, Bourke C, Cass DT (2001) Gastroschisis reduction under anaesthesia in the neonatal unit. J Pediatr Surg 36(11):1672–1674
Bianchi A, Dickson AP (1998) Elective delayed reduction and no anaesthesia ‘minimal intervention management’ for gastroschisis. J Pediatr Surg 33(9):1338–1340
Ing CH, Di Maggio CJ, Malacova E, Whitehouse AJ, Hegarty MK, Feng T et al (2014) Comparative analysis of outcome measures used in examining neurodevelopmental effects of early childhood anesthesia exposure. Anesthesiology 120(6):1319–1332
Orion KC, Krein M, Liao J, Shaaban AF, Pitcher GJ, Shilyansky J (2011) Outcomes of plastic closure in gastroschisis. Surgery 150:177–185
Riboh J, Abrajano CT, Gaber K, Hartman G, Butler MA, Albanese CT et al (2009) Outcomes of sutureless gastroschisis closure. J Pediatr Surg 44:1947–1951
Ogasawara Y, Okazaki T, Kato Y, Lane GJ, Yamataka A (2009) Spontaneous sutureless closure of the abdominal wall defect in gastroschisis using a commercial wound retractor system. Pediatr Surg Int 25:973–976
Pacilli M, Spitz L, Kiely EM, Curry J, Pierro A (2005) Staged repair of giant omphalocele in the neonatal period. J Pediatr Surg 40(5):785–788
Davies MW, Kimble RM, Cartwright DW (2005) Gastroschisis: ward reduction compared with traditional reduction under general anaesthesia. J Pediatr Surg 40(3):523–527
Owen A, Marven S, Johnson P, Kurinczuk J, Spark P, Draper ES et al (2010) Gastroschisis: a national cohort study to describe contemporary surgical strategies and outcomes. J Pediatr Surg 45:1808–1816
Weinsheimer RL, Yanchar NL, Bouchard Kim PK, Laberge JM, Skarsgard ED et al (2008) Gastroschisis closure: does method really matter? J Pediatr Surg 43:874–878
Emani CN, Youssef F, Baird RJ, Laberge JM, Skarsgard ED, Puligandla PS (2015) A risk stratified comparison of fascial versus flap closure techniques on the early outcomes of infants with gastroschisis. J Pediatr Surg 50:102–106
Choi WW, McBride CA, Bourke C, Borzi P, Choo K, Walker R et al (2012) Long-term review of sutureless ward reduction in neonates with gastroschisis in the neonatal unit. J Pediatr Surg 47:1516–1520
Bonnard A, Zamakhshary M, de Silva N, Gerstle JT (2008) Non-operative management of gastroschisis: a case-matched study. Pediatr Surg Int 24:767–771
Serra A, Fitze G, Kamin G, Dinger J, König IR, Roesner D (2008) Preliminary report on elective preterm delivery at 34 weeks and primary abdominal closure for the management of gastroschisis. Eur J Pediatr Surg 18:32–37
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tullie, L.G.C., Bough, G.M., Shalaby, A. et al. Umbilical hernia following gastroschisis closure: a common event?. Pediatr Surg Int 32, 811–814 (2016). https://doi.org/10.1007/s00383-016-3906-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3906-1