Abstract
Chylothorax is a well-recognized complication after neonatal cardiothoracic surgery. Management strategies include cessation of enteral feedings, repeated aspiration, chest drainage, and total parenteral nutrition. Somatostatin and its analogue, octreotide, have been used with promising results. The authors present three cases of neonatal postoperative chylothorax in which octreotide was used. After literature review, we can say that octreotide is relatively safe, and may reduce clinical course and complications associated with neonatal postoperative chylothorax. One should be aware of possible association between octreotide and necrotizing enterocolitis. Prospective controlled trials supporting octreotide use are lacking.
Similar content being viewed by others
Introduction
Chylothorax is a well-recognized complication after neonatal cardiothoracic surgery. Diagnosis is established by needle aspiration or by chest tube insertion. The “milky” pleural aspirate with raised triglycerides and predominance of lymphocytes confirms chylothorax. Although exact etiology of chylothorax following surgery remains unknown, various theories have been proposed, including disruption of lymphatics, injury to the thoracic duct, and back pressure phenomenon of the visceral lymphatics leading to small breaks in the thoracic duct [1]. Management strategies include cessation of enteral feedings, repeated aspiration, chest drainage, and total parenteral nutrition. Ligation of the thoracic duct, pleurodesis of pleuroperitoneal shunting is reserved for refractory cases [2]. Somatostatin and its analogue, octreotide, have been used in treating chylothorax after various cardiothoracic procedures with promising results. The authors present three cases of neonatal postoperative chylothorax in which octreotide was used.
Case reports
Patient 1
A 36-week gestation, 2.46-kg girl was submitted to laparotomy for right diaphragmatic hernia repair in day 2 of life. On eighth postoperative day respiratory distress developed. Chest X-ray showed a moderate right pleural effusion. A 10 F chest tube was inserted, draining 54 ml of chylous and another 63 ml during the following 24 h. Oral feeding was discontinued, and parenteral nutrition started. There was initial decrease in pleural drainage, but on 14th postoperative day there was considerable raise in thoracic tube output and octreotide infusion was started. We used initial dose of 2 μg/kg/h and progressively raised it to maximum dose of 10 μg/kg/h. Chylothorax resolved on 13th day of treatment and thoracic tube was removed (Fig. 1.). On 33rd postoperative day (day 19th of octreotide treatment), the patient was extubated. Control chest X-ray revealed small pleural effusion that resolved in the following 48 h without need for aspiration. Tapering for octreotide was initiated on the 22nd day of treatment. No side effects of octreotide therapy were noted. Medium chain triglyceride (MCT) feeds were introduced on the 24th day of treatment and maternal milk was initiated 6 days after that.
Patient 2
A 37-week gestation, 2.37-kg boy was submitted to laparotomy for left diaphragmatic hernia repair in day two of life. He also had bilateral undescended testis. On second postoperative day a moderate left pleural effusion was noted on the chest X-ray. A 10 F chest tube was inserted and fluid analysis revealed chylothorax. Enteral feeding had not been initiated yet. 24 h drainage started at 60 ml and rose to 218 ml within 3 days (Fig. 2). On the fourth postoperative day we started 1 μg/kg/h octreotide infusion. Octreotide dose was progressively increased upto a maximum dose of 8 μg/kg/h, on the ninth day. By that time, drainage suddenly decreased. MCT diet was introduced in that same day. Complete resolution of chylothorax was achieved on the 12th day of treatment. No side effects were noted. Chest tube was removed and the patient was extubated. Regular milk formula was initiated 13 days after that without pleural effusion recurrence.
Patient 3
A 37-week gestation, 3.02-kg boy was submitted to left thoracotomy for esophageal atresia type C repair on first day of life. He also had a small patent foramen ovale not requiring any intervention. On 11th postoperative day respiratory distress obliged reintubation. Chest X-ray revealed bilateral pleural effusion. 81 ml of chylous was aspirated on the right side. On 12th postoperative day another 14 ml was aspirated and a chest tube was left in place (Fig. 3). Oral feeding had not been initiated yet. Octreotide was promptly initiated at a starting dose of 0.5 μg/kg/h and progressively increased until 10 μg/kg/h. There was a temporary decrease of thoracic output when maximum dose was achieved, but it started increasing by the 25th day of treatment. On the 30th day of treatment pleurodesis was performed using povidone–iodine solution. Chylothorax resolved within 6 days. Thoracic tube was removed 8 days after pleurodesis. Octreotide was stopped on the tenth day. The patient was extubated and started on regular milk formula.
Discussion
Chylothorax after neonatal surgery is usually a transient disorder that will resolve after a period of diminished flow through the thoracic lymphatics. Diminished lymphatic flow can be accomplished by minimizing chyle production, through the use of MCT diet, or (as is usually required) by the discontinuation of enteral feedings altogether. Conservative approach usually entails prolonged pleural drainage, mechanical ventilation, and total parental nutrition. Reported complications of such management include hypoproteinemia, coagulopathy, lymphopenia, hypogammaglobulinemia, line sepsis, and ventilator-associated lung injury. Surgical intervention is recommended if chylous drainage persists after 2–5 weeks of conservative management. Surgical options include thoracic duct ligation, pleuroperitoneal shunting, pleurectomy, or pleurodesis [3]. Pleurodesis is one way to obtain pleural adhesion, obliterating chylous leaks. Available agents include talc, bleomycin, tetracycline, OK-432, and povidone–iodine [4, 5].
The use of somatostatin to treat chylothorax was first reported in an adult in 1990 [6] and in a neonate in 2001 [7]. Octreotide is a synthetic somatostatin analog that has been used in the management of persistent hyperinsulinemic states, in newborn infants [8]. Somatostatin and octreotide cause mild vasoconstriction of splanchnic vessels and reduces gastric, pancreatic and intestinal secretions as well as intestinal absorption and hepatic venous flow, which collectively may act in concert to reduce chyle flow [9]. Reported side-effects include transient loose stools, nausea, flatulence, hypoglycemia and liver dysfunction. Two cases of necrotizing enterocolitis due to octreotide have been reported in neonates. The first case reported was a newborn with a chylothorax after gastroschisis correction [10]. The other case was a 22-day-old boy with refractory hypoglycemia [11].
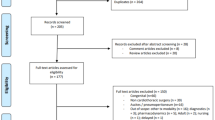
Since the first two cases of reported use of octreotide in postoperative neonatal chylothorax [7], 26 other cases have been reported in the literature [1–3, 10, 12–20] (Table 1). There is significant heterogeneity in dosing regimens, therapeutic durations, and time to start octreotide. All the authors used octreotide as second line treatment. Octreotide was initiated when total parenteral nutrition (TPN) or MCT feeds alone failed in resolving chylothorax. Days to octreotide therapy initiation ranged from 4 to 31. Therapy duration ranged from 3 to 49 days. Intravenous infusion has been the most used mode of administration, although subcutaneous and intravenous bolus have been used. Intravenous infusion dosing ranged from 0.3 to 10 μg/kg/h (7–240 μg/kg/day). Most authors began treatment with a lower dose and progressively raised it, but the dose to elicit significant reduction in lymphorrhea was quite variable. There was no apparent consensus about how long therapy should be continued after chylothorax resolution. Tapering of octreotide was longer if chylous effusion recurred.
There is no consensus about enteral feeding while on octreotide therapy either. Most of the patients were on TPN until the resolution of chylothorax. Some were on MCT feeds from the beginning and others started them before finishing octreotide therapy. Reported side effects included loose stools, transient rash, and the case of necrotizing enterocolitis reported earlier. Gonzalez et al. [1] reported that one of their patients died of sepsis while on octreotide therapy, but the point of origin was not specified.
It is difficult to evaluate octreotide therapy success rate for neonatal chylothorax, especially those due to surgical intervention. Although most of the initial reports presented cases where octreotide or somatostatin had been effective, some recent series of patients presented cases where pleurodesis or surgical procedure was needed to cease chylous drainage. On their series of chylothorax post-congenital diaphragmatic hernia repair, Gonzalez et al. [1] reported that none of their four patients on octreotide therapy had their thoracic tube output consistently reduced, despite a maximum dose of 96 μg/kg/day. Copons Férnandez et al. [14] presented a series of 22 neonatal chylothorax of different etiologies. In their series, five of ten patients who did not respond to TPN were successfully treated with octreotide. Analyzing the postoperative chylothoraxes alone, there was a 50% success rate for a maximum dose of 36 μg/kg/day.
In our experience, two of the three patients had their chylothorax resolved within 12 days after initiation of octreotide therapy. Both these patients had a sudden decrease on chylous output when maximum dose was achieved. The case requiring pleurodesis had a bilateral effusion and large amount of chylous drainage. Massive chylous leakage has been appointed as one of the reasons for octreotide failure in older children [21].
Because there was some concern regarding chylothorax recurrence, octreotide therapy was maintained and even tapered upwards for some days. In either case, we cannot be sure about the exact role of octreotide on chylothorax resolution or was it due to TPN and bowel rest alone.
Conclusion
Despite the significant heterogeneity of case reports published, one can say that octreotide is relatively safe, and may reduce clinical course and complications associated with neonatal postoperative chylothorax. The association between octreotide and necrotizing enterocolitis should be noted. Prospective controlled trials comparing various octreotide regimens and conventional therapy are needed.
References
Gonzalez R, Bryner BS, Teitelbaum DH, Hirschl RB, Drongowski RA, Mychaliska GB (2009) Chylothorax after congenital diaphragmatic hernia repair. J Pediatr Surg 44:1181–1185
Goyal A, Smith NP, Jesudason EC, Kerr S, Losty PD (2003) Octreotide for treatment of chylothorax after repair of congenital diaphragmatic hernia. J Pediatr Surg 38:E19–E20
Au M, Weber TR, Fleming RE (2003) Successful use of somatostatin in a case of neonatal chylothorax. J Pediatr Surg 38:1106–1107
Matsukuma E, Aoki Y, Sakai M, Kawamoto N, Watanabe H, Iwagaki S, Takahashi Y et al (2009) Treatment with OK-432 for persistent congenital chylothorax in newborn infants resistant to octreotide. J Pediatr Surg 44:e37–e39
Brissaud O, Desfrere L, Mohsen R, Fayon M, Demarquez JL (2003) Congenital idiopathic chylothorax in neonates: chemical pleurodesis with povidone–iodine (betadine). Arch Dis Child Fetal Neonatal Ed 88:F531–F533
Ulíbarri JI, Sanz Y, Fuentes C, Mancha A, Aramendia M, Sánchez S (1990) Reduction of lymphorrhagia from ruptured thoracic duct by somatostatin. Lancet 336:258
Buettiker V, Hug MI, Burger R, Baenziger O (2001) Somatostatin: a new therapeutic option for the treatment of chylothorax. Intensive Care Med 27:1083–1086
Glaser B, Hirsch HJ, Landau H (1993) Persistent hyperinsulinemic hypoglycemia of infancy: long-term octreotide treatment without pancreatectomy. J Pediatr 123:644–650
Siu SL, Lam DS (2006) Spontaneous neonatal chylothorax treated with octreotide. J Paediatr Child Health 42:65–67
Mohseni-Bod H, Macrae D, Slavik Z (2004) Somatostatin analog (octreotide) in management of neonatal postoperative chylothorax: is it safe? Pediatr Crit Care Med 5:356–357
Reck-Burneo CA, Parekh A, Velcek FT (2008) Is octreotide a risk factor in necrotizing enterocolitis? J Pediatr Surg 43:1209–1210
Hung WP, Wang JN, Chang (2009) Octreotide therapy in two children with intractable postoperative chylothorax. Int J Cardiol. doi:10.1016/j.ijcard.2008.12.210
Prada Arias M, Rodriguez Barca P, Carbajosa Herrero MT, de Celis Villasana L, Viñals González F (2008) Chylothorax following repair of oesophageal atresia: conservative treatment with octreotide. An Pediatr (Barc) 69:181–196 (in Spanish)
Copons Fernández C, Benítez Segura I, Castillo Salinas F, Salcedo Abizanda S (2008) Neonatal chylothorax: aetiology, clinical course and efficacy of treatment. An Pediatr (Barc) 68:224–231 (in Spanish)
Rocha G, Henriques-Coelho T, Correia-Pinto J, Guedes MB, Guimarães H (2007) Octreotide for conservative management of postoperative chylothorax in the neonate. Acta Med Port 20:467–470 (in Portuguese)
Chan EH, Russel JL, Williams WG (2005) Postoperative chylothorax after cardiothoracic surgery in children. Ann Thorac Surg 80:1864–1871
González Santacruz M, Tarazona Fargueta JL, Muñoz Alvarez P, Mira Navarro J, Jiménez Cobo B (2005) Use of somatostatin in five neonates with chylothorax. An Pediatr (Barc) 63:244–248 (in Spanish)
Tibballs J, Soto R, Bharucha T (2004) Management of newborn lymphangiectasia and chylothorax after cardiac surgery with octreotide infusion. Ann Thorac Surg 77:2213–2215
Clarke SA, Lakhoo K, Sherwood W (2005) Somatostatin for intractable postoperative chylothorax in a premature infant. Pediatr Surg Int 21:390–391
Pettitt TW, Caspi J, Borne A (2002) Treatment of persistent chylothorax after Norwood procedure with somatostatin. Ann Thorac Surg 73:977–979
Rosti L, Bini RM, Chessa M, Butera G, Drago M, Carminati M (2002) The effectiveness of octreotide in the treatment of post-operative chylothorax. Eur J Pediatr 161:149–150
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Moreira-Pinto, J., Rocha, P., Osório, A. et al. Octreotide in the treatment of neonatal postoperative chylothorax: report of three cases and literature review. Pediatr Surg Int 27, 805–809 (2011). https://doi.org/10.1007/s00383-010-2730-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-010-2730-2