Abstract
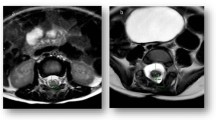
The purpose of this study was to determine factors that might be involved in neurological deterioration and the role of surgical treatment in patients with lumbosacral spinal lipoma. Pre- and postoperative courses of 34 patients were retrospectively analyzed. The age at surgery ranged from 1 month to 47 years. The records of preoperative neurological status indicated that older patients had more severe deficits, while all 8 asymptomatic patients were under 5 years of age. Motor deficits were noted in 9 patients, in 7 of whom the lipoma extended cranially beyond the L5 level. Transitional-type lipomas were accompanied by more severe deficits (asymptomatic 1, symptomatic 17) than other types (asymptomatic 7, symptomatic 9). Postoperative follow-up periods ranged from 5 months to 13 years. During these periods, 7 of the 8 asymptomatic patients remained neurologically intact. Nine of the 26 symptomatic patients improved. Age, extension of the lipoma in the spinal canal and type of lipoma will influence the preoperative neurological status of the patients. Early untethering surgery is recommended in patients with large lipomas extending beyond the L5 level.
Similar content being viewed by others
Author information
Authors and Affiliations
Additional information
Received: 24 August 1998 Revised: 19 July 1999
Rights and permissions
About this article
Cite this article
Koyanagi, I., Iwasaki, Y., Hida, K. et al. Factors in neurological deterioration and role of surgical treatment in lumbosacral spinal lipoma. Child's Nerv Syst 16, 143–149 (2000). https://doi.org/10.1007/s003810050481
Issue Date:
DOI: https://doi.org/10.1007/s003810050481