Abstract
Background
Filum terminale lipomas (FTL) represent a sub-type of spinal lipomas, where there is fatty infiltration of the filum. It becomes a surgical entity when it manifests as clinical or radiological tethered cord syndrome. Intraoperative neuromonitoring (IONM) has been suggested as a valuable tool in children for tethered cord surgeries. FTL is distinct and cannot be compared with complex tethered cord syndrome (TCS). Untethering an FTL is a relatively straightforward microsurgical exercise, usually based on anatomical findings. Neurological morbidity in FTL untethering is extremely low. The necessity of IONM in FTL has not been evaluated. The objective of this study was to identify the role of IONM in untethering an FTL
Methods
Available electronic data and case files were interrogated to identify children (0–18 years) who underwent an untethering of FTL between 2008 and 2019. We had a shift in our policy and tried to use IONM as often as possible in all tethered cord surgery from 2014. All children were categorised under ‘IONM implemented’ or ‘no IONM’ group. Outcomes analysed were as follows: (1) Clinical status on short-term and long-term follow-up, (2) alteration of surgical course by IONM and (3) complications specifically associated with IONM
Results
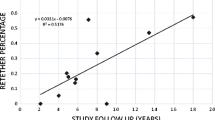
Among 80 children included in this study, IONM was implemented in 37 children and 43 children underwent untethering without IONM. 32.5% of children were ‘syndromic’. Seventy-five percent of children were under age 3 years during surgery. Both groups (No IONM vs. IONM implemented) were well matched in most variables. Majority of ‘no IONM’ surgeries were performed prior to 2014. There was no neurological morbidity in the entire cohort. Mean duration of follow-up was 49.10 (± 33.67) months. Short-term and long-term clinical status remained stable in both cohorts. In 16 children, the filum was stimulated. Based on our protocol, majority had a negative response. One child showed a positive response, contradicted by thorough microscopic inspection. Despite a positive response, the filum was untethered. IONM was not associated with any complication in this study.
Conclusion
FTL untethering is an inherently low-risk microsurgery in experienced hands with rarely reported neurological morbidity. IONM may not be required for all FTL and may be used more judiciously.





Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Abbreviations
- FTL:
-
Filum terminale lipoma
- TCS:
-
Tethered cord syndrome
- IONM:
-
Intraoperative neuromonitoring
- MEP:
-
Motor evoked potential
- SSEP:
-
Somato-sensory evoked potentials
- EMG:
-
Electromyography
- CMAP:
-
Compound muscle action potential
- TIVA:
-
Total intravenous anaesthesia
References
Morota N, Ihara S, Ogiwara H (2017) New classification of spinal lipomas based on embryonic stage. J Neurosurg Pediatr 19:428–439. https://doi.org/10.3171/2016.10.PEDS16247
Blount JP, Elton S (2001) Spinal lipomas. Neurosurg Focus 10:1–13
Cools MJ, Al-Holou WN, Stetler WR et al (2014) Filum terminale lipomas: Imaging prevalence, natural history, and conus position - clinical article. J Neurosurg Pediatr 13:559–567. https://doi.org/10.3171/2014.2.PEDS13528
O’Neill BR, Yu AK, Tyler-Kabara EC (2010) Prevalence of tethered spinal cord in infants with VACTERL: clinical article. J Neurosurg Pediatr 6:177–182. https://doi.org/10.3171/2010.5.PEDS09428
Kuo MF, Tsai Y, Hsu WM, Chen RS, Tu YK, Wang HS (2007) Tethered spinal cord and VACTERL association. J Neurosurg 106:201–204. https://doi.org/10.3171/ped.2007.106.3.201
Ostling LR, Bierbrauer KS, Kuntz C IV (2012) Outcome, reoperation, and complications in 99 consecutive children operated for tight or fatty filum. World Neurosurg 77:187–191. https://doi.org/10.1016/j.wneu.2011.05.017
Vassilyadi M, Tataryn Z, Merziotis M (2013) Retethering in children after sectioning of the filum terminale. Pediatr Neurosurg 48:335–341. https://doi.org/10.1159/000353477
Von Koch CS, Quinones-Hinojosa A, Gulati M et al (2002) Clinical outcome in children undergoing tethered cord release utilizing intraoperative neurophysiological monitoring. Pediatr Neurosurg 37:81–86. https://doi.org/10.1159/000065109
Yong RL, Habrock-Bach T, Vaughan M, Kestle JR, Steinbok P (2011) Symptomatic retethering of the spinal cord after section of a tight filum terminale. Neurosurgery 68:1594–1601. https://doi.org/10.1227/NEU.0b013e31821246c6
Hoving EW, Haitsma E, Ophuis CMCO, Journée HL (2011) The value of intraoperative neurophysiological monitoring in tethered cord surgery. Child’s Nerv Syst 27:1445–1452. https://doi.org/10.1007/s00381-011-1471-4
Kothbauer KF, Deletis V (2010) Intraoperative neurophysiology of the conus medullaris and cauda equina. Child’s Nerv Syst 26:247–253. https://doi.org/10.1007/s00381-009-1020-6
Kothbauer KF, Novak K (2004) Intraoperative monitoring for tethered cord surgery: an update. Neurosurg Focus 16:1–5. https://doi.org/10.3171/foc.2004.16.2.1
Sala F, Squintani G, Tramontano V, Arcaro C, Faccioli F, Mazza C (2013) Intraoperative neurophysiology in tethered cord surgery: techniques and results. Child’s Nerv Syst 29:1611–1624. https://doi.org/10.1007/s00381-013-2188-3
Halevi PD, Udayakumaran S, Ben-Sira L, Constantini S (2011) The value of postoperative MR in tethered cord: a review of 140 cases. Child’s Nerv Syst 27:2159–2162. https://doi.org/10.1007/s00381-011-1578-7
Sala F, Bricolo A, Faccioli F, et al (2007) Surgery for intramedullary spinal cord tumors: the role of intraoperative (neurophysiological) monitoring. In: European Spine Journal. Springer, p 130
Hadley MN, Shank CD, Rozzelle CJ, Walters BC (2017) Guidelines for the use of electrophysiological monitoring for surgery of the human spinal column and spinal cord. Neurosurgery 81:713–732
Sala F, Palandri G, Basso E, Lanteri P, Deletis V, Faccioli F, Bricolo A (2006) Motor evoked potential monitoring improves outcome after surgery for intramedullary spinal cord tumors: a historical control study. Neurosurgery 58:1129–1141. https://doi.org/10.1227/01.NEU.0000215948.97195.58
Yi YG, Kim K, Shin HI, Bang MS, Kim HS, Choi J, Wang KC, Kim SK, Lee JY, Phi JH, Seo HG (2019) Feasibility of intraoperative monitoring of motor evoked potentials obtained through transcranial electrical stimulation in infants younger than 3 months. J Neurosurg Pediatr 23:758–766. https://doi.org/10.3171/2019.1.PEDS18674
Gavaret M, Pesenti S, Choufani E, Pennaroli D, Bollini G, Jouve JL (2016) Intraoperative spinal cord monitoring in children under 4 years old. Eur Spine J 25:1847–1854. https://doi.org/10.1007/s00586-016-4553-x
Quiñones-Hinojosa A, Gadkary CA, Gulati M, von Koch CS, Lyon R, Weinstein PR, Yingling CD (2004) Neurophysiological monitoring for safe surgical tethered cord syndrome release in adults. Surg Neurol 62:127–133. https://doi.org/10.1016/j.surneu.2003.11.025
Selçuki M, Vatansever S, Inan S, Erdemli E, Bağdatoğlu C, Polat A (2003) Is a filum terminale with a normal appearance really normal? Child’s Nerv Syst 19:3–10. https://doi.org/10.1007/s00381-002-0665-1
Pierre-Kahn A, Zerah M, Renier D, Cinalli G, Sainte-Rose C, Lellouch-Tubiana A, Brunelle F, Merrer ML, Giudicelli Y, Pichon J, Kleinknecht B, Nataf F (1997) Congenital lumbosacral lipomas. Child’s Nerv Syst 13:298–335
Brophy JD, Sutton LN, Zimmerman RA, Bury E, Schut L (1989) Magnetic resonance imaging of lipomyelomeningocele and tethered cord. Neurosurgery:336. https://doi.org/10.1097/00006123-198909000-00002
Kumar GSS, Rajshekhar V, Babu KS (2006) Intraoperative mapping of sacral nervous system (S2 - 4). Br J Neurosurg 20:396–402. https://doi.org/10.1080/02688690601101481
Gaddam SSK, Santhi V, Babu S, Chacko G, Baddukonda RA, Rajshekhar V (2012) Gross and microscopic study of the filum terminale: does the filum contain functional neural elements? Laboratory investigation. J Neurosurg Pediatr 9:86–92. https://doi.org/10.3171/2011.10.PEDS11102
Saker E, Henry BM, Tomaszewski KA, Loukas M, Iwanaga J, Oskouian RJ, Tubbs RS (2017) The filum terminale internum and externum: a comprehensive review. J Clin Neurosci 40:6–13. https://doi.org/10.1016/j.jocn.2016.12.020
Laratta JL, Shillingford JN, Ha A et al (2018) Utilization of intraoperative neuromonitoring throughout the United States over a recent decade: an analysis of the nationwide inpatient sample. J Spine Surg 4:211–219. https://doi.org/10.21037/jss.2018.04.05
Schraag S, Pradelli L, Alsaleh AJO, Bellone M, Ghetti G, Chung TL, Westphal M, Rehberg S (2018) Propofol vs. inhalational agents to maintain general anaesthesia in ambulatory and in-patient surgery: a systematic review and meta-analysis. BMC Anesthesiol 18:162. https://doi.org/10.1186/s12871-018-0632-3
Acknowledgement
We thank Dr Swetha Kumar for editorial assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lalgudi Srinivasan, H., Valdes-Barrera, P., Agur, A. et al. Filum terminale lipomas—the role of intraoperative neuromonitoring. Childs Nerv Syst 37, 931–939 (2021). https://doi.org/10.1007/s00381-020-04856-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04856-4
Keywords
Profiles
- Jehuda Soleman View author profile