Abstract
Purpose
Three-tesla intraoperative MRI (iMRI) is a promising tool that could help confirm complete resections and disconnections in pediatric epilepsy surgery, leading to improved outcomes. However, a large proportion of epileptogenic pathologies in children are poorly defined on imaging, which brings into question the utility of iMRI for these cases. Our aim was to compare postoperative seizure outcomes between iMRI- and non-iMRI-based epilepsy surgeries.
Methods
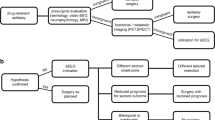
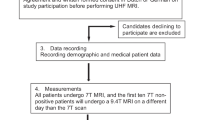
We performed a comparative retrospective analysis of non-iMRI- versus iMRI-based epilepsy surgeries with 2-year follow-up. Patients were stratified into well-defined cases (WDCs), poorly defined cases (PDCs), and diffuse hemispheric cases (DHCs). Primary outcomes were rates of complete seizure freedom and surgical complications. Secondary outcomes included good (Engel class I/II) seizure outcome, extent of resection/disconnection, and operative duration. Regression models were used to adjust for confounding.
Results
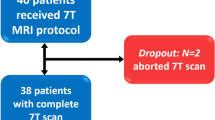
Thirty-nine iMRI-based and 39 non-iMRI-based surgeries were included. The distributions of age, sex, and lesion class in each era were similar, but the distributions of individual pathologies varied. Seizure freedom and complication rates at 2-year follow-up were not different between the groups, but Engel class I/II outcome was more common in the iMRI group. Extent of resection/disconnection and length of surgery were similar in both groups. PDCs had the worst outcomes, which were unchanged by the use of iMRI.
Conclusion
Three-tesla iMRI-based epilepsy surgery may have the potential to improve patient outcomes. However, we conclude that iMRI, in its current state of use at our institute, does not improve outcomes for children undergoing epilepsy surgery. Given that its use appears safe, further research on this technology is warranted, particularly for the most challenging PDCs.

Similar content being viewed by others
References
Blumcke I, Aronica E, Urbach H, Alexopoulos A, Gonzalez-Martinez JA (2014) A neuropathology-based approach to epilepsy surgery in brain tumors and proposal for a new terminology use for long-term epilepsy-associated brain tumors. Acta Neuropathol 128:39–54. doi:10.1007/s00401-014-1288-9
Alshafai L, Ochi A, Go C, McCoy B, Hawkins C, Otsubo H, Snead OC, Rutka J, Widjaja E (2014) Clinical, EEG, MRI, MEG, and surgical outcomes of pediatric epilepsy with astrocytic inclusions versus focal cortical dysplasia. Epilepsia 55:1568–1575. doi:10.1111/epi.12756
Balogun JA, Khan OH, Taylor M, Dirks P, Der T, Carter Snead Iii O, Weiss S, Ochi A, Drake J, Rutka JT (2014) Pediatric awake craniotomy and intra-operative stimulation mapping. J Clin Neurosci 21:1891–1894. doi:10.1016/j.jocn.2014.07.013
Bi WL, Chiocca EA (2014) Image-guided maximal resection of intrinsic tumors. World Neurosurgery 82:604–605. doi:10.1016/j.wneu.2014.04.070
Wang ZI, Jones SE, Ristic AJ, Wong C, Kakisaka Y, Jin K, Schneider F, Gonzalez-Martinez JA, Mosher JC, Nair D, Burgess RC, Najm IM, Alexopoulos AV (2012) Voxel-based morphometric MRI post-processing in MRI-negative focal cortical dysplasia followed by simultaneously recorded MEG and stereo-EEG. Epilepsy Res 100:188–193. doi:10.1016/j.eplepsyres.2012.02.011
Leach JL, Miles L, Henkel DM, Greiner HM, Kukreja MK, Holland KD, Rose DF, Zhang B, Mangano FT (2014) Magnetic resonance imaging abnormalities in the resection region correlate with histopathological type, gliosis extent, and postoperative outcome in pediatric cortical dysplasia. J Neurosurg Pediatr 14:68–80. doi:10.3171/2014.3.PEDS13560
Hader WJ, Mackay M, Otsubo H, Chitoku S, Weiss S, Becker L, Snead OC, Snead OC III, Rutka JT (2004) Cortical dysplastic lesions in children with intractable epilepsy: role of complete resection. J Neurosurg Pediatr 100:110–117. doi:10.3171/ped.2004.100.2.0110
Ng WH, Mukhida K, Rutka JT (2010) Image guidance and neuromonitoring in neurosurgery. Childs Nerv Syst 26:491–502. doi:10.1007/s00381-010-1083-4
Duncan JS, de Tisi J (2013) MRI in the diagnosis and management of epileptomas. Epilepsia 54:40–43. doi:10.1111/epi.12442
Hong S-C, Hong SC, Kang K-S, Kang KS, Seo DW, Seo DW, Hong SB, Hong SB, Lee M, Lee M, Nam DH, Nam D-H, Lee J-I, Lee JI, Kim JS, Kim JS, Shin H-J, Shin HJ, Park K, Park K, Eoh W, Eoh W, Suh YL, Suh Y-L, Kim JH, Kim J-H (2000) Surgical treatment of intractable epilepsy accompanying cortical dysplasia. J Neurosurg 93:766–773. doi:10.3171/jns.2000.93.5.0766
Mühlebner A, Gröppel G, Dressler A, Reiter-Fink E, Kasprian G, Prayer D, Dorfer C, Czech T, Hainfellner JA, Coras R, Blumcke I, Feucht M (2014) Epilepsy surgery in children and adolescents with malformations of cortical development—outcome and impact of the new ILAE classification on focal cortical dysplasia. Epilepsy Res 108:1652–1661. doi:10.1016/j.eplepsyres.2014.08.012
Palmini A, Palmini A, Andermann F, Andermann F, Olivier A, Olivier A, Tampieri D, Tampieri D, Robitaille Y, Robitaille Y, Andermann E, Andermann E, Wright G, Wright G (1991) Focal neuronal migration disorders and intractable partial epilepsy: a study of 30 patients. Ann Neurol 30:741–749. doi:10.1002/ana.410300602
Chandra SP, Bal CS, Jain S, Joshua SP, Gaikwad S, Garg A, Ansari A, Nehra A, Sarkar C, Tripathi M (2014) Intraoperative coregistration of magnetic resonance imaging, positron emission tomography, and electrocorticographic data for neocortical lesional epilepsies may improve the localization of the epileptogenic focus: a pilot study. World Neurosurgery 82:110–117. doi:10.1016/j.wneu.2013.02.057
Raybaud C, Shroff M, Rutka JT, Chuang SH (2006) Imaging surgical epilepsy in children. Childs Nerv Syst 22:786–809. doi:10.1007/s00381-006-0132-5
Kelly JJ, Hader WJ, Myles ST, Sutherland GR (2005) Epilepsy surgery with intraoperative MRI at 1.5 T. Neurosurg Clin N Am 16:173–183. doi:10.1016/j.nec.2004.07.006
Kurwale NS, Chandra SP, Chouksey P, Arora A, Garg A, Sarkar C, Bal C, Tripathi M (2015) Impact of intraoperative MRI on outcomes in epilepsy surgery: preliminary experience of two years. Br J Neurosurg 29:380–385. doi:10.3109/02688697.2014.1003034
Sommer B, Grummich P, Coras R, Kasper BS, Blumcke I, Hamer HM, Stefan H, Buchfelder M, Roessler K (2013) Integration of functional neuronavigation and intraoperative MRI in surgery for drug-resistant extratemporal epilepsy close to eloquent brain areas. Neurosurg Focus 34:E4. doi:10.3171/2013.2.FOCUS12397
Engel J Jr, Van Ness PC, Rasmussen TB, Ojemann LM (1993) Outcome with respect to epileptic seizures. 609–621
Zou G (2004) A modified Poisson regression approach to prospective studies with binary data. Am J Epidemiol 159:702–706
Sommer B, Wimmer C, Coras R, Blumcke I, Lorber B, Hamer HM, Stefan H, Buchfelder M, Roessler K (2015) Resection of cerebral gangliogliomas causing drug-resistant epilepsy: short- and long-term outcomes using intraoperative MRI and neuronavigation. Neurosurg Focus 38:E5. doi:10.3171/2014.10.FOCUS14616
Kabat J, Król P (2012) Focal cortical dysplasia—review. Polish journal of radiology / Polish Medical Society of Radiology 77:35–43
Dorfer C, Widjaja E, Ochi A, Carter Snead Iii O, Rutka JT (2015) Epilepsy surgery: recent advances in brain mapping, neuroimaging and surgical procedures. J Neurosurg Sci 59:141–155
Wu X-T, Rampp S, Buchfelder M, Kuwert T, Blümcke I, Dörfler A, Zhou D, Stefan H (2012) Interictal magnetoencephalography used in magnetic resonance imaging-negative patients with epilepsy. Acta Neurol Scand 127:274–280. doi:10.1111/j.1600-0404.2012.01712.x
Albert GW, Ibrahim GM, Otsubo H, Ochi A, Go CY, Snead OC, Snead OC III, Drake JM, Rutka JT (2014) Magnetoencephalography-guided resection of epileptogenic foci in children. J Neurosurg Pediatr 14:532–537. doi:10.3171/2014.8.PEDS13640
Chuang NA, Otsubo H, Pang EW, Chuang SH (2006) Pediatric magnetoencephalography and magnetic source imaging. Neuroimaging Clin N Am 16:193–210. doi:10.1016/j.nic.2005.11.001
Lee DJ, Zwienenberg-Lee M, Seyal M, Shahlaie K (2015) Intraoperative computed tomography for intracranial electrode implantation surgery in medically refractory epilepsy. J Neurosurg 122:526–531. doi:10.3171/2014.9.JNS13919
Cui Z-Q, Ling Z-P, Song H-F, Hu S, Sun G-C, Chen X-L, Pan L-S, Li C, Xu B-N (2014) Combining pyramidal tract mapping, microscopic-based neuronavigation, and intraoperative magnetic resonance imaging improves outcome of epilepsy foci resection in the sensorimotor cortex. Turkish Neurosurgery 24:538–545. doi:10.5137/1019-5149.JTN.9517-13.0
Klamer S, Rona S, Elshahabi A, Lerche H, Braun C, Honegger J, Erb M, Focke NK (2015) Multimodal effective connectivity analysis reveals seizure focus and propagation in musicogenic epilepsy. NeuroImage 113:70–77. doi:10.1016/j.neuroimage.2015.03.027
Acknowledgments
We would like to dedicate this article in the memory of Dr. Denis Melançon who was a brilliant pioneering neuroradiologist who contributed significantly to the use and interpretation of MRI and who was a tremendous colleague and friend.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics
The present study was approved by the Research Ethics Board of the Montreal Children’s Hospital.
Conflict of interest
None of the authors has any conflict of interest to disclose.
Rights and permissions
About this article
Cite this article
Warsi, N.M., Lasry, O., Farah, A. et al. 3-T intraoperative MRI (iMRI) for pediatric epilepsy surgery. Childs Nerv Syst 32, 2415–2422 (2016). https://doi.org/10.1007/s00381-016-3263-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-016-3263-3