Abstract
Purpose
The main treatment for majority of pediatric brain tumors relies on surgery. In postoperative period, patients require monitoring in a pediatric intensive care unit (PICU). In this study, we analyzed the incidence of postoperative neurological complications and the outcome of neurological impairment in individual patients.
Patients and methods
Our retrospective single-center study concerned all patients who were admitted to the PICU of the University Hospital of Angers between 2002 and 2008, after brain tumor resection. Population, perioperative data, and outcome through the stay in PICU have been analyzed.
Results
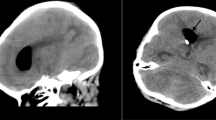
We reported 117 neurosurgical procedures. Majority of children (85.3%) were affected by neurological deficit before surgery: cranial nerve palsy and cerebellar syndrome were the most frequent impairment. In the first 2 days, neurological symptoms improved for 27 patients (23.7%), especially in children with preoperative cerebellar syndrome, convulsions, or endocrine disorders. Mean length of stay in PICU was correlated with the severity of neurological impairment (p = 0.006). Five children presented a transient mutism after surgery for infratentorial tumors (n = 5/54, 9.2%). Eight spontaneous cerebral spinal fluid leaks occurred precociously after surgery, and neurological infections complicated half of them. Neurological infections occurred in 12 patients (ten meningitis, one ventriculitis, and one brain abscess). One patient died after surgery.
Conclusions
All these complications and their risk factors have to be systematically searched for in order to decrease postoperative morbidity of brain tumors in children. They justify neurosurgeons and anesthesiologists specialized in these pathologies.






Similar content being viewed by others
References
Desandes E, Lacour B, Sommelet D, Buemi A, Danzon A, Delafosse P, Grosclaude P, Mace-Lesech J, Raverdy-Bourdon N, Tretarre B, Velten M, Brugieres L (2004) Cancer incidence among adolescents in France. Pediatr Blood Cancer 43:742
Desandes E, Clavel J, Berger C, Bernard JL, Blouin P, de Lumley L, Demeocq F, Freycon F, Gembara P, Goubin A, Le Gall E, Pillon P, Sommelet D, Tron I, Lacour B (2004) Cancer incidence among children in France, 1990–1999. Pediatr Blood Cancer 43:749
Meyer P, Orliaguet G, Blanot S, Cuttaree H, Jarreau MM, Charron B, Carli P (2002) Anesthesia-resuscitation for intracranial expansive processes in children. Ann Fr Anesth Rèanim 21:90
Morelli D, Pirotte B, Lubansu A, Detemmerman D, Aeby A, Fricx C, Berre J, David P, Brotchi J (2005) Persistent hydrocephalus after early surgical management of posterior fossa tumors in children: is routine preoperative endoscopic third ventriculostomy justified? J Neurosurg 103:247
Abdullah S, Qaddoumi I, Bouffet E (2008) Advances in the management of pediatric central nervous system tumors. Ann NY Acad Sci 1138:22
Nejat F, El Khashab M, Rutka JT (2008) Initial management of childhood brain tumors: neurosurgical considerations. J Child Neurol 23:1136
Chang SM, Parney IF, McDermott M, Barker FG 2nd, Schmidt MH, Huang W, Laws ER Jr, Lillehei KO, Bernstein M, Brem H, Sloan AE, Berger M (2003) Perioperative complications and neurological outcomes of first and second craniotomies among patients enrolled in the Glioma Outcome Project. J Neurosurg 98:1175
Pollack IF (1994) Brain tumors in children. N Engl J Med 331:1500
Kaderali Z, Lamberti-Pasculli M, Rutka JT (2009) The changing epidemiology of paediatric brain tumours: a review from the Hospital for Sick Children. Childs Nerv Syst 25:787
Bauchet L, Rigau V, Mathieu-Daude H, Fabbro-Peray P, Palenzuela G, Figarella-Branger D, Moritz J, Puget S, Bauchet F, Pallusseau L, Duffau H, Coubes P, Tretarre B, Labrousse F, Dhellemmes P (2009) Clinical epidemiology for childhood primary central nervous system tumors. J Neurooncol 92:87
Sainte-Rose C, Cinalli G, Roux FE, Maixner R, Chumas PD, Mansour M, Carpentier A, Bourgeois M, Zerah M, Pierre-Kahn A, Renier D (2001) Management of hydrocephalus in pediatric patients with posterior fossa tumors: the role of endoscopic third ventriculostomy. J Neurosurg 95:791
Russell SM, Elliott R, Forshaw D, Kelly PJ, Golfinos JG (2005) Resection of parietal lobe gliomas: incidence and evolution of neurological deficits in 28 consecutive patients correlated to the location and morphological characteristics of the tumor. J Neurosurg 103:1010
Rekate HL, Grubb RL, Aram DM, Hahn JF, Ratcheson RA (1985) Muteness of cerebellar origin. Arch Neurol 42:697
Siffert J, Poussaint TY, Goumnerova LC, Scott RM, LaValley B, Tarbell NJ, Pomeroy SL (2000) Neurological dysfunction associated with postoperative cerebellar mutism. J Neurooncol 48:75
Rath GP, Bithal PK, Chaturvedi A, Dash HH (2007) Complications related to positioning in posterior fossa craniectomy. J Clin Neurosci 14:520
Dailey AT, McKhann GM 2nd, Berger MS (1995) The pathophysiology of oral pharyngeal apraxia and mutism following posterior fossa tumor resection in children. J Neurosurg 83:467
Kotil K, Eras M, Akcetin M, Bilge T (2008) Cerebellar mutism following posterior fossa tumor resection in children. Turk Neurosurg 18:89
Dubey A, Sung WS, Shaya M, Patwardhan R, Willis B, Smith D, Nanda A (2009) Complications of posterior cranial fossa surgery—an institutional experience of 500 patients. Surg Neurol 72:369
Kalfas IH, Little JR (1988) Postoperative hemorrhage: a survey of 4992 intracranial procedures. Neurosurgery 23:343
Palmer JD, Sparrow OC, Iannotti F (1994) Postoperative hematoma: a 5-year survey and identification of avoidable risk factors. Neurosurgery 35:1061
Dashti SR, Baharvahdat H, Spetzler RF, Sauvageau E, Chang SW, Stiefel MF, Park MS, Bambakidis NC (2008) Operative intracranial infection following craniotomy. Neurosurg Focus 24:E10
Korinek AM (1997) Risk factors for neurosurgical site infections after craniotomy: a prospective multicenter study of 2944 patients. The French Study Group of Neurosurgical Infections, the SEHP, and the C-CLIN Paris-Nord. Service Epidemiologie Hygiene et Prevention. Neurosurgery 41:1073
Korinek AM, Baugnon T, Golmard JL, van Effenterre R, Coriat P, Puybasset L (2006) Risk factors for adult nosocomial meningitis after craniotomy: role of antibiotic prophylaxis. Neurosurgery 59:126
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Proust Houdemont, S., De Carli, E., Delion, M. et al. Short-term neurological outcome of children after surgery for brain tumors: incidence and characteristics in a pediatric intensive care unit. Childs Nerv Syst 27, 933–941 (2011). https://doi.org/10.1007/s00381-010-1373-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-010-1373-x