Abstract
Objective
Shunt infection is a common and serious complication of cerebrospinal fluid (CSF) shunting most commonly caused by skin flora contamination at surgery. Recent studies indicate that the use of antibiotic-impregnated (AI) shunt systems may reduce the risk of postoperative shunt infections. We evaluated the incidence of shunt infections associated with the use of AI shunt catheters and compared it with the incidence associated with standard non-AI catheters.
Materials and methods
All shunt procedures performed by one surgeon using AI catheters were reviewed. An equal number of consecutive shunt procedures performed by the same surgeon using non-AI catheters were reviewed from the period immediately before the introduction of the AI system. Patients with <9 months of follow-up were excluded; all shunt infections and shunt-related complications were recorded. The proportions of infected shunts in the AI and control groups were compared using a χ 2 analysis.
Conclusion
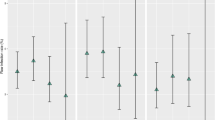
We reviewed 160 shunt procedures (80 per group). The infection rate was 5.0% among patients with AI catheters compared with 8.8% in the control group (P = 0.534, Fischer’s exact). The average time to infection was similar between the two groups. Among the AI group, the shunt infection rate did not differ between ventricular catheter, distal catheter revisions, and revisions of ventricular and peritoneal tubing. In contrast with other reports, we found no significant reduction in the pediatric CSF shunt infection rate with the use of AI shunt systems. Any recommendation for or against the routine use of AI systems in children requires a prospective, blinded, randomized-controlled trial with adequate power.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Aryan HE, Meltzer HS, Park MS, Bennett RL, Jandial R, Levy ML (2005) Initial experience with antibiotic-impregnated silicone catheters for shunting of cerebrospinal fluid in children. Childs Nerv Syst 21:56–61
Bayston R, Grove N, Siegel J, Lawellin D, Barsham S (1989) Prevention of hydrocephalus shunt catheter colonisation in vitro by impregnation with antimicrobials. J Neurol Neurosurg Psychiatry 52:605–609
Borgbjerg BM, Gjerris F, Albeck MJ, Borgesen SE (1995) Risk of infection after cerebrospinal fluid shunt: an analysis of 884 first-time shunts. Acta Neurochir (Wien) 136:1–7
Borges LF (1982) Cerebrospinal fluid shunts interfere with host defenses. Neurosurgery 10:55–60
Chapman PH, Borges LF (1985) Shunt infections: prevention and treatment. Clin Neurosurg 32:652–664
Cotton MF, Hartzenberg B, Donald PR, Burger PJ (1991) Ventriculoperitoneal shunt infections in children. A 6-year study. S Afr Med J 79:139–142
Drake JM, Kestle JR, Milner R, Cinalli G, Boop F, Piatt J Jr, Haines S, Schiff SJ, Cochrane DD, Steinbok P, MacNeil N (1998) Randomized trial of cerebrospinal fluid shunt valve design in pediatric hydrocephalus. Neurosurgery 43:294–303, discussion 303–305
Fan-Havard P, Nahata MC (1987) Treatment and prevention of infections of cerebrospinal fluid shunts. Clin Pharm 6:866–880
Gardner P, Leipzig T, Phillips P (1985) Infections of central nervous system shunts. Med Clin North Am 69:297–314
Gardner P, Leipzig TJ, Sadigh M (1988) Infections of mechanical cerebrospinal fluid shunts. Curr Clin Top Infect Dis 9:185–214
George R, Leibrock L, Epstein M (1979) Long-term analysis of cerebrospinal fluid shunt infections. A 25-year experience. J Neurosurg 51:804–811
Govender ST, Nathoo N, van Dellen JR (2003) Evaluation of an antibiotic-impregnated shunt system for the treatment of hydrocephalus. J Neurosurg 99:831–839
Gray ED, Peters G, Verstegen M, Regelmann WE (1984) Effect of extracellular slime substance from Staphylococcus epidermidis on the human cellular immune response. Lancet 1:365–367
Hampl J, Schierholz J, Jansen B, Aschoff A (1995) In vitro and in vivo efficacy of a rifampin-loaded silicone catheter for the prevention of CSF shunt infections. Acta Neurochir (Wien) 133:147–152
Ignelzi RJ, Kirsch WM (1975) Follow-up analysis of ventriculoperitoneal and ventriculoatrial shunts for hydrocephalus. J Neurosurg 42:679–682
James HE, Walsh JW, Wilson HD, Connor JD, Bean JR, Tibbs PA (1980) Prospective randomized study of therapy in cerebrospinal fluid shunt infection. Neurosurgery 7:459–463
Kestle JR, Drake JM, Cochrane DD, Milner R, Walker ML, Abbott R 3rd, Boop FA, Endoscopic Shunt Insertion Trial participants (2003) Lack of benefit of endoscopic ventriculoperitoneal shunt insertion: a multicenter randomized trial. J Neurosurg 98:284–290
Kestle JR, Garton HJ, Whitehead WE, Drake JM, Kulkarni AV, Cochrane DD, Muszynski C, Walker ML (2006) Management of shunt infections: a multicenter pilot study. J Neurosurg 105:177–181
Kockro RA, Hampl JA, Jansen B, Peters G, Scheihing M, Giacomelli R, Kunze S, Aschoff A (2000) Use of scanning electron microscopy to investigate the prophylactic efficacy of rifampin-impregnated CSF shunt catheters. J Med Microbiol 49:441–450
Kohnen W, Schaper J, Klein O, Tieke B, Jansen B (1998) A silicone ventricular catheter coated with a combination of rifampin and trimethoprim for the prevention of catheter-related infections. Zentralbl Bakteriol 287:147–156
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36:858–862
Meirovitch J, Kitai-Cohen Y, Keren G, Fiendler G, Rubinstein E (1987) Cerebrospinal fluid shunt infections in children. Pediatr Infect Dis J 6:921–924
Peters G, Locci R, Pulverer G (1982) Adherence and growth of coagulase-negative staphylococci on surfaces of intravenous catheters. J Infect Dis 146:479–482
Schierholz JM, Pulverer G (1997) Development of a new CSF-shunt with sustained release of an antimicrobial broad-spectrum combination. Zentralbl Bakteriol 286:107–123
Schoenbaum SC, Gardner P, Shillito J (1975) Infections of cerebrospinal fluid shunts: epidemiology, clinical manifestations, and therapy. J Infect Dis 131:543–552
Sciubba DM, Stuart RM, McGirt MJ, Woodworth GF, Samdani A, Carson B, Jallo GI (2005) Effect of antibiotic-impregnated shunt catheters in decreasing the incidence of shunt infection in the treatment of hydrocephalus. J Neurosurg 103:131–136
Walters BC, Hoffman HJ, Hendrick EB, Humphreys RP (1984) Cerebrospinal fluid shunt infection. Influences on initial management and subsequent outcome. J Neurosurg 60:1014–1021
Walters BC, Hoffman HJ, Hendrick EB, Humphreys RP (1985) Decreased risk of infection in cerebrospinal fluid shunt surgery using prophylactic antibiotics: a case-control study. Z Kinderchir 40(Suppl 1):15–18
Acknowledgments
The authors thank Kristin Kraus for her editorial assistance in preparing this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kan, P., Kestle, J. Lack of efficacy of antibiotic-impregnated shunt systems in preventing shunt infections in children. Childs Nerv Syst 23, 773–777 (2007). https://doi.org/10.1007/s00381-007-0296-7
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-007-0296-7