Abstract
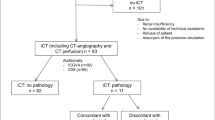
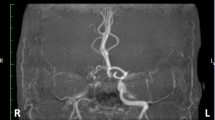
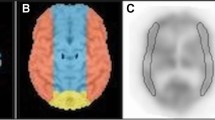
We evaluate the utility of providing a pulsatile blood flow by applying off-pump coronary artery bypass grafting (CABG) or intra-aortic balloon pumping (IABP) with conventional CABG to prevent perioperative stroke in patients with cerebral hypoperfusion on single-photon emission-computed tomography (SPECT). A total of 286 patients underwent isolated CABG with a cerebral magnetic resonance angiography (MRA) evaluation between 2006 and 2015. Seventy-five had significant stenosis and/or occlusion of craniocervical vessels; the other 211 had no significant stenosis. Cerebral SPECT was performed for 49 (SPECT group) of the 75 patients. The SPECT group was further divided into a normal perfusion (NP) (n = 37); and a hypoperfusion (HP) (n = 12). In the present study we compared the NP group and the 211 patients with no significant stenosis (as a control group) to the HP group. No strokes occurred in the HP group, and 1 stroke occurred at the time of operation in the control group. Postoperative stroke within 30 days occurred in 3 patients in the control group; the difference was not statistically significant. The long-term stroke-free rates of the HP and Control group did not differ to a statistically significant extent. The functional evaluation of cerebral perfusion by SPECT is important when patients have significant stenotic lesions on cerebral MRA. Maintaining an adequate pulsatile flow by off-pump CABG or IABP with conventional CABG will help prevent perioperative stroke, even if cerebral hypoperfusion is detected by SPECT.



Similar content being viewed by others
References
Roach GW, Kanchuger M, Mangano CM, Newman M, Nussmeier N, Wolman R, Aggarwal A, Marschall K, Graham SH, Ley C (1996) Adverse cerebral outcomes after coronary bypass surgery. Multicenter Study of Perioperative Ischemia Research Group and the Ischemia Research and Education Foundation Investigators. N Engl J Med 335(25):1857–1863
Puskas JD, Winston AD, Wright CE, Gott JP, Brown WM 3rd, Craver JM, Jones EL, Guyton RA, Weintraub WS (2000) Stroke after coronary artery operation: incidence, correlates, outcome, and cost. Ann Thorac Surg 69(4):1053–1056
Salazar JD, Wityk RJ, Grega MA, Borowicz LM, Doty JR, Petrofski JA, Baumgartner WA (2001) Stroke after cardiac surgery: short- and long-term outcomes. Ann Thorac Surg 72(4):1195–1201
Borger MA, Ivanov J, Weisel RD, Rao V, Peniston CM (2001) Stroke during coronary bypass surgery: principal role of cerebral macroemboli. Eur J Cardiothorac Surg 19(5):627–632
Hirotani T, Kameda T, Kumamoto T, Shirota S, Yamano M (2000) Stroke after coronary artery bypass grafting in patients with cerebrovascular disease. Ann Thorac Surg 70(5):1571–1576
Matsuura K, Mogi K, Sakurai M, Kawamura T, Takahara Y (2011) Impact of preexisting cerebral ischemia detected by magnetic resonance imaging and angiography on late outcome after coronary artery bypass surgery. Ann Thorac Surg 91(3):665–670
Okamoto K, Ushijima Y, Okuyama C, Nakamura T, Nishimura T (2002) Measurement of cerebral blood flow using graph plot analysis and I-123 iodoamphetamine. Clin Nucl Med 27(3):191–196
McKhann GM, Goldsborough MA, Borowicz LM Jr, Mellits ED, Brookmeyer R, Quaskey SA, Baumgartner WA, Cameron DE, Stuart RS, Gardner TJ (1997) Predictors of stroke risk in coronary artery bypass patients. Ann Thorac Surg 63(2):516–521
Tarakji KG, Sabik JF 3rd, Bhudia SK, Batizy LH, Blackstone EH (2011) Temporal onset, risk factors, and outcomes associated with stroke after coronary artery bypass grafting. JAMA 305(4):381–390
Horwich P, Buth KJ, Légaré JF (2013) New onset postoperative atrial fibrillation is associated with a long-term risk for stroke and death following cardiac surgery. J Cardiac Surg 28(1):8–13
Endo D, Kato TS, Iwamura T, Oishi A, Yokoyama Y, Kuwaki K, Inaba H, Amano A (2017) The impact of surgical left atrial appendage amputation/ligation on stroke prevention in patients undergoing off-pump coronary artery bypass grafting. Heart Vessels 32(6):726–734
Imasaka K, Yasaka M, Tayama E, Tomita Y (2015) Obstructive carotid and/or intracranial artery disease rarely affects the incidence of haemodynamic ischaemic stroke during cardiac surgery: a study on brain perfusion single-photon emission computed tomography with acetazolamide. Eur J Cardiothorac Surg 48(5):739–746
Nakamura M, Okamoto F, Nakanishi K, Maruyama R, Yamada A, Ushikoshi S, Terasaka S, Kuroda S, Sakai K, Higami T (2008) Does intensive management of cerebral hemodynamics and atheromatous aorta reduce stroke after coronary artery surgery? Ann Thorac Surg 85(2):513–519
Adamsson Eryd S, Östling G, Rosvall M, Persson M, Smith JG, Melander O, Hedblad B, Engström G (2014) Carotid intima-media thickness is associated with incidence of hospitalized atrial fibrillation. Atherosclerosis 233(2):673–678
Barr RG, Ahmed FS, Carr JJ, Hoffman EA, Jiang R, Kawut SM, Watson K (2012) Subclinical atherosclerosis, airflow obstruction and emphysema: the MESA Lung Study. Eur Respir J 39(4):846–854
Likosky DS, Marrin CA, Caplan LR, Baribeau YR, Morton JR, Weintraub RM, Hartman GS, Hernandez F Jr, Braff SP, Charlesworth DC, Malenka DJ, Ross CS, O'Connor GT, Northern New England Cardiovascular Disease Study Group (2003) Determination of etiologic mechanisms of strokes secondary to coronary artery bypass graft surgery. Stroke 34(12):2830–2834
Momjian-Mayor I, Baron JC (2005) The pathophysiology of watershed infarction in internal carotid artery disease: review of cerebral perfusion studies. Stroke 36(3):567–577
Abildstrom H, Høgh P, Sperling B, Moller JT, Yndgaard S, Rasmussen LS (2002) Cerebral blood flow and cognitive dysfunction after coronary surgery. Ann Thorac Surg 73(4):1174–1178
Yi X, Chi W, Wang C, Zhang B, Lin J (2015) Low-molecular-weight heparin or dual antiplatelet therapy is more effective than aspirin alone in preventing early neurological deterioration and improving the 6-month outcome in ischemic stroke patients. J Clin Neurol 11(1):57–65
Van Gelder IC, Healey JS, Crijns HJGM, Wang J, Hohnloser SH, Gold MR, Capucci A, Lau CP, Morillo CA, Hobbelt AH, Rienstra M, Connolly SJ (2017) Duration of device-detected subclinical atrial fibrillation and occurrence of stroke in ASSERT. Eur Heart J. 38(17):1339–1344
Vermeer SE, Hollander M, van Dijk EJ, Hofman A, Koudstaal PJ, Breteler MM, Rotterdam Scan Study (2003) Silent brain infarcts and white matter lesions increase stroke risk in the general population: the Rotterdam Scan Study. Stroke 34(5):1126–1129
Kakkos SK, Nicolaides AN, Charalambous I, Thomas D, Giannopoulos A, Naylor AR, Geroulakos G, Abbott AL, Asymptomatic Carotid Stenosis, and Risk of Stroke (ACSRS) Study Group (2014) Predictors and clinical significance of progression or regression of asymptomatic carotid stenosis. J Vasc Surg 59(4):956–967
Kowalewski M, Pawliszak W, Malvindi PG, Bokszanski MP, Perlinski D, Raffa GM, Kowalkowska ME, Zaborowska K, Navarese EP, Kolodziejczak M, Kowalewski J, Tarelli G, Taggart DP, Anisimowicz L (2016) Off-pump coronary artery bypass grafting improves short-term outcomes in high-risk patients compared with on-pump coronary artery bypass grafting: meta-analysis. J Thorac Cardiovasc Surg 151(1):60–77
Kleisli T, Cheng W, Jacobs MJ, Mirocha J, Derobertis MA, Kass RM, Blanche C, Fontana GP, Raissi SS, Magliato KE, Trento A (2005) In the current era, complete revascularization improves survival after coronary artery bypass surgery. J Thorac Cardiovasc Surg 129(6):1283–1291
Serraino GF, Marsico R, Musolino G, Ventura V, Gulletta E, Santè P, Renzulli A (2012) Pulsatile cardiopulmonary bypass with intra-aortic balloon pump improves organ function and reduces endothelial activation. Circ J 76(5):1121–1129
Salameh A, Kühne L, Grassl M, Gerdom M, von Salisch S, Vollroth M, Bakhtiary F, Mohr FW, Dähnert I, Dhein S (2015) Protective effects of pulsatile flow during cardiopulmonary bypass. Ann Thorac Surg 99(1):192–199
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declared that they have no potential conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Teramoto, C., Mutsuga, M., Kawaguchi, O. et al. A functional evaluation of cerebral perfusion for coronary artery bypass grafting patients. Heart Vessels 34, 1122–1131 (2019). https://doi.org/10.1007/s00380-019-01348-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-019-01348-7