Abstract
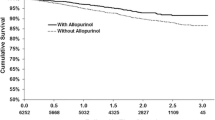
Antihistamines are widely used to treat pruritus in patients receiving hemodialysis. In a previous cross-sectional study, we reported an association between antihistamine use and the absence of eccentric cardiac hypertrophy in patients receiving hemodialysis. Therefore, in this study, we sought to evaluate the efficacy of antihistamines on all-cause and cardiovascular mortality in patients receiving hemodialysis according to our outpatient dialysis database. We used a propensity score matching method. Among the 389 patients receiving hemodialysis according to our database, we extracted those taking antihistamines and matched them with patients not taking antihistamines using propensity scores based on 38 variables. All-cause mortality and cardiovascular mortality were estimated by the Kaplan–Meier method, and a log-rank test was used to examine the differences between the survival curves. We included 154 patients, or 77 matched pairs, from the entire cohort (c-statistic = 0.78, p < 0.0001). There were no differences in any background factor between the antihistamine and non-antihistamine group. During the mean observational period of 5.4 years, 50 patients died, and the all-cause mortality rate was 27.3% (21 patients) in the antihistamine group and 37.3% (29 patients) in the non-antihistamine group (p = 0.0314). The cardiovascular mortality rate was 16.9% (13 patients) in the antihistamine group and 25.9% (20 patients) in the non-antihistamine group (p = 0.0417). The results of this study suggest that all-cause and cardiovascular mortality improved with antihistamine use in patients receiving hemodialysis. However, the clinical efficacy of antihistamines needs to be confirmed in a prospective randomized study in the future.


Similar content being viewed by others
References
Iseki K (2000) Cerebrovascular disease in ESRD. In: Loscalzo J, London G (eds) The cardiovascular complications in end-stage renal disease. Oxford University Press, Oxford, pp 443–461
Ogawa T, Koeda M, Nitta K (2015) Left ventricular diastolic dysfunction in end-stage kidney disease: pathogenesis, diagnosis, and treatment. Ther Apher Dial 19:427–435
Yamazaki M, Ogawa T, Tamei N, Ando Y, Nitta K (2011) Relation of N-terminal pro-B-type natriuretic peptide (NT-proBNP) and left atrial volume index to left ventricular function in chronic hemodialysis patients. Heart Vessels 26:421–427
Omae K, Ogawa T, Yoshikawa M, Nitta K (2012) Left atrial dilatation and ST-T changes predict cardiovascular outcome in chronic hemodialysis patients. Heart Vessels 27:610–617
Inoue T, Ogawa T, Ishida H, Ando Y, Nitta K (2012) Aortic arch calcification evaluated on chest X-ray is a strong independent predictor of cardiovascular events in chronic hemodialysis patients. Heart Vessels 27:135–142
Kitamura K, Fujii H, Nakai K, Kono K, Goto S, Nishii T, Kono A, Nishi S (2017) Relationship between cardiac calcification and left ventricular hypertrophy in patients with chronic kidney disease at hemodialysis initiation. Heart Vessels. doi:10.1007/s00380-017-0969-4
Obokata M, Kurosawa K, Ishida H, Ito K, Ogawa T, Ando Y, Kurabayashi M, Negishi K (2017) Incremental prognostic value of ventricular-arterial coupling over ejection fraction in patients with maintenance hemodialysis. J Am Soc Echocardiogr. doi:10.1016/j.echo.2016.12.014
Cice G, Ferrara L, D’Andrea A, D’Isa S, Di Benedetto A, Cittadini A, Russo PE, Golino P, Calabrò R (2003) Carvedilol increases two-year survival in dialysis patients with dilated cardiomyopathy: a prospective, placebo-controlled trial. J Am Coll Cardiol 41:1438–1444
Foley RN, Herzog CA, Collins AJ, United States Renal Data System (2002) Blood pressure and long-term mortality in United States hemodialysis patients: USRDS Waves 3 and 4 Study. Kidney Int 62:1784–1790
Nakao K, Makino H, Morita S, Takahashi Y, Akizawa T, Saito A, Asano Y, Kurokawa K, Fukuhara S, Akiba T (2009) J-DOPPS Investigators Group: beta-blocker prescription and outcomes in hemodialysis patients from the Japan Dialysis Outcomes and Practice Patterns Study. Nephron Clin Pract 113:c132–c139
Wetmore JB, Shireman TI (2009) The ABCs of cardioprotection in dialysis patients: a systematic review. Am J Kidney Dis 53:457–466
Akbari A, Knoll G, Ferguson D, McCormick B, Davis A, Biyani M (2009) Angiotensin-converting enzyme inhibitors and angiotensin receptor blockers in peritoneal dialysis: systematic review and meta-analysis of randomized controlled trials. Perit Dial Int 29:554–561
Navaneethan SD, Nigwekar SU, Perkovic V, Johnson DW, Craig JC, Strippoli GF (2009) HMG CoA reductase inhibitors (statins) for dialysis patients. Cochrane Database Syst Rev (2):CD004289. doi:10.1002/14651858.CD004289.pub3
Takahashi A, Takase H, Toriyama T, Sugiura T, Kurita Y, Ueda R, Dohi Y (2006) Candesartan, an angiotensin II type-1 receptor blocker, reduces cardiovascular events in patients on chronic haemodialysis-a randomized study. Nephrol Dial Transplant 21:2507–2512
Cice G, Di Benedetto A, D’Isa S, D’Andrea A, Marcelli D, Gatti E, Calabrò R (2010) Effects of telmisartan added to Angiotensin-converting enzyme inhibitors on mortality and morbidity in hemodialysis patients with chronic heart failure a double-blind, placebo-controlled trial. J Am Coll Cardiol 56:1701–1708
Kelley JL, Chi DS, Abou-Auda W, Smith JK, Krishnaswamy G (2000) The molecular role of mast cells in atherosclerotic cardiovascular disease. Mol Med Today 6:304–308
Levick SP, McLarty JL, Murray DB, Freeman RM, Carver WE, Brower GL (2009) Cardiac mast cells mediate left ventricular fibrosis in the hypertensive rat heart. Hypertension 53:1041–1047
Tang CW, Lan C, Liu R (2004) Increased activity of the intestinal mucosal mast cells in rats with multiple organ failure. Chin J Dig Dis 5:81–86
Janicki JS, Brower GL, Gardner JD, Forman MF, Stewart JA Jr, Murray DB, Chancey AL (2006) Cardiac mast cell regulation of matrix metalloproteinase-related ventricular remodeling in chronic pressure or volume overload. Cardiovasc Res 69:657–665
Omae K, Ogawa T, Yoshikawa M, Nitta K (2010) The use of H1-receptor antagonists and left ventricular remodeling in patients on chronic hemodialysis. Heart Vessels 25:163–169
Zoccali C, Benedetto FA, Mallamaci F, Tripepi G, Giacone G, Stancanelli B, Cataliotti A, Malatino LS (2004) Left ventricular mass monitoring in the follow-up of dialysis patients: prognostic value of left ventricular hypertrophy progression. Kidney Int 65:1492–1498
Stack AG, Saran R (2002) Clinical correlates and mortality impact of left ventricular hypertrophy among new ESRD patients in the United States. Am J Kidney Dis 40:1202–1210
Austin PC (2007) Propensity-score matching in the cardiovascular surgery literature from 2004 to 2006: a systematic review and suggestions for improvement. J Thorac Cardiovasc Surg 134:1128–1135
Macfarlane PW, Latif S (1996) Automated serial ECG comparison based on the Minnesota code. J Electrocardiol 29:29–34
Kovanen PT (2009) Mast cells in atherogenesis: actions and reactions. Curr Atheroscler Rep 11:214–219
Lindstedt KA, Kovanen PT (2004) Mast cells in vulnerable coronary plaques: potential mechanisms linking mast cell activation to plaque erosion and rupture. Curr Opin Lipidol 15:567–573
Tsuruda T, Kato J, Hatakeyama K, Kojima K, Yano M, Yano Y, Nakamura K, Nakamura-Uchiyama F, Matsushima Y, Imamura T, Onitsuka T, Asada Y, Nawa Y, Eto T, Kitamura K (2008) Adventitial mast cells contribute to pathogenesis in the progression of abdominal aortic aneurysm. Circ Res 102:1368–1377
Sun J, Zhang J, Lindholt JS, Sukhova GK, Liu J, He A, Abrink M, Pejler G, Stevens RL, Thompson RW, Ennis TL, Gurish MF, Libby P, Shi GP (2009) Critical role of mast cell chymase in mouse abdominal aortic aneurysm formation. Circulation 120:973–982
Akaishi Y, Hattori Y, Yoshimoto K, Kitabatake A, Yasuda K, Kanno M (2000) Involvement of tyrosine phosphorylation in the positive inotropic effect produced by H (1)-receptors with histamine in guinea-pig left atrium. Br J Pharmacol 130:907–915
Galajda Z, Balla J, Szentmiklosi AJ, Biro T, Czifra G, Dobrosi N, Cseppento A, Patonay L, Roszer T, Balla G, Popescu LM, Lekli I, Tosaki A (2011) Histamine and H1-histamine receptors faster venous circulation. J Cell Mol Med 15:2614–2623
Rozenberg I, Sluka SH, Rohrer L, Hofmann J, Becher B, Akhmedov A, Soliz J, Mocharla P, Borén J, Johansen P, Steffel J, Watanabe T, Lüscher TF, Tanner FC (2010) Histamine H1 receptor promotes atherosclerotic lesion formation by increasing vascular permeability for low-density lipoproteins. Arterioscler Thromb Vasc Biol 30:923–930
Yamada S, Wang KY, Tanimoto A, Guo X, Nabeshima A, Watanabe T, Sasaguri Y (2013) Histamine receptors expressed in circulating progenitor cells have reciprocal actions in ligation-induced arteriosclerosis. Pathol Int 63:435–447
Saiura A, Sata M, Hirata Y, Nagai R, Makuuchi M (2001) Tranilast inhibits transplant-associated coronary arteriosclerosis in a murine model of cardiac transplantation. Eur J Pharmacol 433:163–168
Guo T, Chen WQ, Zhang C, Zhao YX, Zhang Y, Guo T, Chen WQ, Zhang C, Zhao YX, Zhang Y (2009) Chymase activity is closely related with plaque vulnerability in a hamster model of atherosclerosis. Atherosclerosis 207:59–67
Hocher B, Godes M, Olivier J, Weil J, Eschenhagen T, Slowinski T, Neumayer HH, Bauer C, Paul M, Pinto YM (2002) Inhibition of left ventricular fibrosis by tranilast in rats with renovascular hypertension. J Hypertens 20:745–751
Hei ZQ, Gan XL, Huang PJ, Wei J, Shen N, Gao WL (2008) Influence of ketotifen, cromolyn sodium, and compound 48/80 on the survival rates after intestinal ischemia reperfusion injury in rats. BMC Gastroenterol 8:42
Miyazawa N, Watanabe S, Matsuda A, Kondo K, Hashimoto H, Umemura K, Nakashima M (1998) Role of histamine H1 and H2 receptor antagonists in the prevention of intimal thickening. Eur J Pharmacol 362:53–59
Matsumori A, Yamamoto K, Shimada M (2010) Cetirizine a histamine H1 receptor antagonist improves viral myocarditis. J Inflamm (Lond) 7:39
Carmichael AJ, McHugh MI, Martin AM (1991) Renal itch as an indicator of poor outcome. Lancet 337:1225–1226
Narita I, Alchi B, Omori K, Sato F, Ajiro J, Saga D, Kondo D, Skatsume M, Maruyama S, Kazama JJ, Akazawa K, Gejyo F (2006) Etiology and prognostic significance of severe uremic pruritus in chronic hemodialysis patients. Kidney Int 69:1626–1632
Acknowledgements
The authors would like to thank the dialysis room staffs of Yoshikawa Clinic for their invaluable cooperation in data collection in this study and Enago (http://www.enago.jp) for the English language review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Omae, K., Yoshikawa, M., Sakura, H. et al. Efficacy of antihistamines on mortality in patients receiving maintenance hemodialysis: an observational study using propensity score matching. Heart Vessels 32, 1195–1201 (2017). https://doi.org/10.1007/s00380-017-0989-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0989-0