Abstract
Purpose
Robot-assisted radical prostatectomy (RARP) is a common surgical procedure for the treatment of prostate cancer. Although beneficial, it can lead to intraoperative hypoxia due to high-pressure pneumoperitoneum and Trendelenburg position. This study explored the use of oxygen reserve index (ORi) to monitor and predict hypoxia during RARP.
Methods
A retrospective analysis was conducted on 329 patients who underwent RARP at the Seoul National University Bundang Hospital between July 2021 and March 2023. Various pre- and intraoperative variables were collected, including ORi values. The relationship between ORi values and hypoxia occurrence was assessed using receiver operating characteristic curves and logistic regression analysis.
Results
Intraoperative hypoxia occurred in 18.8% of the patients. The receiver operating characteristic curve showed a satisfactory area under the curve of 0.762, with the ideal ORi cut-off value for predicting hypoxia set at 0.16. Sensitivity and specificity were 64.5% and 75.7%, respectively. An ORi value of < 0.16 and a higher body mass index were identified as independent risk factors of hypoxia during RARP.
Conclusions
ORi monitoring provides a non-invasive approach to predict intraoperative hypoxia during RARP, enabling early management. Additionally, the significant relationship between a higher body mass index and hypoxia underscores the importance of individualized patient assessment.
Similar content being viewed by others
Introduction
Robot-assisted radical prostatectomy (RARP) is a widely performed surgery, accounting for 70–85% of prostatectomies performed in the United States [1]. During RARP, a high-pressure pneumoperitoneum is applied, and the patient is placed in the Trendelenburg position [2]. Although this surgical position (high-pressure pneumoperitoneum + Trendelenburg position) has the advantage of improving the surgeon’s visibility and protecting other organs, it can make mechanical ventilation difficult for patients owing to the cephalad movement of the diaphragm [3]. Consequently, hypoxia may occur, leading to tissue hypoxia, hemodynamic instability, and postoperative complications that require immediate intervention [4].
Pulse oximetry is a widely used method for determining oxygen saturation (SpO2) and diagnosing hypoxia during surgery [5]. However, it is important to note that SpO2 remains almost constant when the partial pressure of oxygen (PaO2) exceeds approximately 80 mmHg [6, 7]. This characteristic limits its effectiveness in predicting impending hypoxia, as SpO2 values may not decrease significantly until PaO2 falls below 80 mmHg. This limitation may require additional monitoring strategies to identify slight changes in oxygenation and offer early warnings of impending hypoxia.
The oxygen reserve index (ORi) (Masimo Corp., Irvine, CA, USA) is a monitoring parameter that can continuously and noninvasively measure oxygen reserves [8]. The index is a dimensionless value ranging from 0.00 to 1.00, corresponding to the arterial partial pressure of oxygen levels ranging from 100 to 200 mmHg [9]. ORi monitoring may aid in detecting hypoxia in advance during ventilatory impairment [8, 9]. Therefore, clinicians may benefit from ORi monitoring for appropriate and prompt management of patients at risk of respiratory compromise.
Our institution uses ORi as a routine monitoring parameter in patients undergoing RARP. This study aimed to analyze the use of ORi in patients undergoing RARP, propose a cut-off value for hypoxia, and investigate its correlation with intraoperative hypoxia.
Materials and methods
Ethics statement
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB number B-2305-828-101). Because this was a retrospective study, the requirement for informed consent was waived.
Population
This study included patients who underwent RARP for prostate cancer between July 2021 and March 2023. Patients whose intraoperative ORi data were not recorded, those who did not undergo ORi monitoring during surgery, and those who underwent ORi monitoring after surgical position (high pneumoperitonuem + Trendelenburg position) were excluded.
Anesthesia and monitoring
Patients were transferred to the operating room after receiving premedication with 0.02 mg/kg of midazolam in the reception area. They were monitored using electrocardiography, pulse oximetry, and non-invasive blood pressure measurements. A sensor (Rainbow® sensor, R1 25L, Revision M, Masimo Corp., Irvine, CA, USA) that can measure ORi and SpO2 was applied to the fourth finger and covered with a shield. General anesthesia was maintained with sevoflurane, desflurane, or propofol using target-controlled infusion. Mechanical ventilation was maintained with a fraction of inspired oxygen of 0.5 and a tidal volume of 6–8 ml/kg (ideal body weight). The respiratory rate was adjusted to maintain the end-tidal carbon dioxide at 30–35 mmHg. Positive end-expiratory pressure (PEEP) (0–10 cmH2O) was applied at the anesthesiologist’s discretion.
Surgical procedure
The four-armed da Vinci robot system was used to perform RARP via the transperitoneal approach. Patients were placed in the lithotomy position. The following procedures were performed after docking: (1) bladder detachment; (2) endopelvic fascial incision; (3) dorsal venous complex dissection; (4) bladder neck dissection; (5) dissection of the vas deferens and seminal vesicle; (6) dissection of the posterior, lateral, and apical spaces; (7) posterior reconstruction; and (8) vesicourethral anastomosis and bladder neck reconstruction [10].
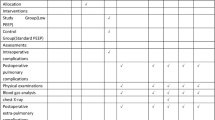
Clinical data collection
We reviewed the electronic medical records and collected pre- and intraoperative data. Preoperative data included age, height, weight, body mass index (BMI), American Society of Anesthesiologists class, smoking history, comorbid pulmonary disease (chronic obstructive pulmonary disease, asthma, tuberculosis, interstitial lung disease, and bronchiectasis), history of lung surgery, and pulmonary function test results. Intraoperative data included the pressure of the pneumoperitoneum, main anesthetics used, PEEP, ORi (recorded 1 min before pneumoperitoneum), SpO2, and occurrence of intraoperative hypoxia. Intraoperative hypoxia was defined as SpO2 < 95% during the docking of the robotic system, based on the World Health Organization’s guideline and several studies [11,12,13,14,15,16].
Statistical analysis
We used R version 3.6.1 (R Foundation for Statistical Computing, Vienna, Austria) with the “pROC” package to draw receiver operating characteristic (ROC) curves and determine the cut-off value [17]. Other statistical analyses were performed using Statistical Package for the Social Sciences version 22 for Windows (SPSS Inc., Chicago, IL, USA). Continuous variables were presented as mean ± standard deviation or median [interquartile range] based on a normal distribution. Categorical variables were presented as numbers (percentages). Univariate and multivariate logistic analyses were performed to identify the potential risk factors for intraoperative hypoxia. Initially, univariate logistic analysis was carried out for all variables, and variables with P < 0.1 were selected for multivariate logistic analysis using forward selection. Statistical significance was set at P < 0.05.
Results
A total of 878 patients underwent RARP between July 2021 and March 2023. Of these patients, 146 had no recorded ORi data, 378 were not monitored for ORi during surgery, and 25 were monitored for ORi after surgical position was established (high pneumoperitoneum + Trendelenburg position). Thus, a total of 329 patients were included in the final analysis. Intraoperative hypoxia was identified in 62 patients (18.8%) (Fig. 1). Table 1 summarizes the preoperative and intraoperative variables.
An ROC curve was used to determine the optimal cut-off value for ORi in predicting hypoxia (Fig. 2). The area under the ROC curve was 0.762, which was considered acceptable. The ROC curve showed that 0.16 was the ideal ORi cut-off value for predicting hypoxia. Sensitivity and specificity were 64.5% and 75.7%, respectively.
Table 2 shows the results of univariate and multivariate logistic regression analyses for the occurrence of intraoperative hypoxia. An ORi value of < 0.16 was an independent risk factor for hypoxia during RARP (odds ratio [OR] 3.532, 95% confidence interval [CI] 1.864–6.695, P < 0.001). In addition, higher BMI independently increased the occurrence of intraoperative hypoxia (OR 1.348, 95% CI, 1.183–1.535; P < 0.001).
Discussion
This study aimed to investigate the role of ORi as a predictive measure for intraoperative hypoxia during RARP. We found that an ORi value of < 0.16 and a higher BMI were independent risk factors for intraoperative hypoxia.
Our data indicated that 18.8% of patients undergoing RARP experienced hypoxia during docking of the robotic system. Compared to our findings, a previous study of patients undergoing robot-assisted gynecologic surgery showed a lower incidence of intraoperative hypoxia [18]. Although the surgical position (pneumoperitoneum and Trendelenburg position) was similar to that used in RARP, intraoperative hypoxia occurred in 3.75% of patients. This discrepancy can be explained by the pressure of the pneumoperitoneum applied during robot-assisted surgery. The authors reported that the pressure range was 8–15 mmHg during robot-assisted gynecologic surgery, whereas the pressure was relatively higher (10–17 mmHg) during RARP. The higher pressure used in our study may have influenced more significant physiological changes [19], possibly leading to a higher incidence of intraoperative hypoxia. Another possible reason for this discrepancy could be the definition of hypoxia. Badawy et al. [18] defined hypoxia as SpO2 of < 90%, whereas we used a different threshold, which could account for the different rates of hypoxia observed. Patient factors, including age, BMI, and overall health status, may also have contributed to the variation in the occurrence of hypoxia.
Pulse oximetry measures arterial oxygen saturation. Owing to the relationship between SpO2 and PaO2, SpO2 remains relatively stable until PaO2 drops below 80 mmHg [6, 7]. Conversely, ORi provides an integrated assessment of both arterial and venous oxygen saturation. Even if SpO2 reaches a plateau at PaO2 levels above 80 mmHg, variations in venous oxygen saturation may still occur [20]. This principle enables ORi to provide more sensitive and comprehensive information about oxygen status.
In our analysis, the cut-off value of ORi, which helps predict the occurrence of hypoxia, was 0.16. Previous studies have evaluated the ability of ORi to predict hypoxia and suggested a cut-off value for hypoxia occurrence [21, 22]. However, Hille et al. [21] suggested a higher cut-off value for ORi (0.4) to indicate hypoxia during endotracheal intubation in critically ill patients. Applegate et al. [22] found that a decrease in ORi to 0.24 could be a warning sign of lowering PaO2 to 100 mmHg. These variations in the cut-off values can be attributed to the different criteria for hypoxia used in the studies (95% vs. 97%). Nevertheless, these findings provide valuable insights into predicting hypoxia using ORi. To the best of our knowledge, this study introduces a novel approach by utilizing ORi, in conjunction with pulse oximetry, to provide a more comprehensive monitoring strategy. This approach aims to detect and warn of impending hypoxia earlier in patients undergoing surgeries that require high pneumoperitoneum and Trendelenburg position, thereby enhancing patient safety and outcomes.
The significant association between ORi and hypoxia observed in our study is consistent with previous research, suggesting that ORi can serve as an early warning signal for hypoxia before it is detected by traditional pulse oximetry. One study explored the use of ORi to measure the oxygen reserves during rapid sequence induction [23]. The authors analyzed data from 16 patients and revealed that ORi could anticipate a decrease in oxygenation approximately 30 s before any notable decline in SpO2. They suggested that the incidence of hypoxia during rapid sequence induction can be reduced by ORi monitoring. In another study, including 38 pediatric patients who underwent general anesthesia for ophthalmic artery catheterization, the authors found that ORi values were consistently lower in patients with cardiorespiratory events than those without (0.03 vs. 0.25) [24]. They recommended that clinicians prepare for inadequate ventilation in patients with a low ORi before the procedure. Similarly, observing a low ORi allows for potentially preventive interventions and improved patient safety during RARP.
A higher BMI was independently associated with intraoperative hypoxia. This finding is consistent with the results of a previous study. Kendale et al. [25] conducted a retrospective cohort analysis of 15,238 patients who underwent general anesthesia for noncardiac surgery and found a significant increase in the incidence of intraoperative hypoxia, defined as SpO2 < 90%, with increasing BMI.
This study has some limitations. First, the retrospective nature of this study may have introduced a bias. Second, we could not adjust for all potential confounding factors, such as intraoperative fluid management or other comorbidities. Third, more than half of the included patients underwent RARP with a high pneumoperitoneum pressure of 17 mmHg. This factor, along with the variability in standard practices regarding pneumoperitoneum pressure, may limit the generalizability of our findings and underscores the need for further research on the impact of different pneumoperitoneum pressures on clinical outcomes, including the incidence of hypoxia and the predictability of ORi in RARP settings across various surgical practices.
Conclusions
This study investigated the potential role of ORi as a predictive measure for intraoperative hypoxia during RARP. The findings demonstrated that an ORi value of < 0.16 and a higher BMI were independent risk factors for intraoperative hypoxia. This study emphasizes the potential benefits of ORi monitoring in managing patients undergoing RARP, allowing for immediate intervention and potentially enhancing patient safety. Further prospective studies are needed to assess the applicability of ORi monitoring in procedures beyond RARP and to explore the effectiveness of specific ORi-guided ventilatory management strategies, including a detailed protocol for intervention based on predicted hypoxia.
Data availability
The data sets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Palma-Zamora I, Abdollah F, Rogers C, Jeong W (2022) Robot-assisted radical prostatectomy: advancements in surgical technique and perioperative care. Front Surg 9:944561. https://doi.org/10.3389/fsurg.2022.944561
Ahn JH, Lim CH, Chung HI, Choi SU, Youn SZ, Lim HJ (2011) Postoperative renal function in patients is unaltered after robotic-assisted radical prostatectomy. Korean J Anesthesiol 60:192–197. https://doi.org/10.4097/kjae.2011.60.3.192
Meininger D, Byhahn C, Bueck M, Binder J, Kramer W, Kessler P, Westphal K (2002) Effects of prolonged pneumoperitoneum on hemodynamics and acid-base balance during totally endoscopic robot-assisted radical prostatectomies. World J Surg 26:1423–1427. https://doi.org/10.1007/s00268-002-6404-7
Lan L, Cen Y, Jiang L, Miao H, Lu W (2021) Risk factors for the development of intraoperative hypoxia in patients undergoing nonintubated video-assisted thoracic surgery: a retrospective study from a Single Center. Med Sci Monit 27:e928965. https://doi.org/10.12659/MSM.928965
Pedersen T, Nicholson A, Hovhannisyan K, Møller AM, Smith AF, Lewis SR (2014) Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev 2014:CD002013. https://doi.org/10.1002/14651858.CD002013.pub3
Severinghaus JW (1979) Simple, accurate equations for human blood O2 dissociation computations. J Appl Physiol Respir Environ Exerc Physiol 46:599–602. https://doi.org/10.1152/jappl.1979.46.3.599
Tsymbal E, Ayala S, Singh A, Applegate RL 2nd, Fleming NW (2021) Study of early warning for desaturation provided by Oxygen Reserve Index in obese patients. J Clin Monit Comput 35:749–756. https://doi.org/10.1007/s10877-020-00531-w
Szmuk P, Steiner JW, Olomu PN, Ploski RP, Sessler DI, Ezri T (2016) Oxygen reserve index: a novel non-invasive measure of oxygen reserve–A pilot study. Anesthesiology 124:779–784. https://doi.org/10.1097/ALN.0000000000001009
Alday E, Nieves JM, Planas A (2020) Oxygen reserve index predicts hypoxemia during one-lung ventilation: An observational diagnostic study. J Cardiothorac Vasc Anesth 34:417–422. https://doi.org/10.1053/j.jvca.2019.06.035
Mottrie A, Mazzone E, Wiklund P, Graefen M, Collins JW, De Groote R, Dell’Oglio P, Puliatti S, Gallagher AG (2021) Objective assessment of intraoperative skills for robot-assisted radical prostatectomy (RARP): results from the ERUS Scientific and Educational Working Groups Metrics Initiative. BJU Int 128:103–111. https://doi.org/10.1111/bju.15311
World Health Organization WHO (2011) Pulse Oximetry Training Manual. WHO Library Cataloguing-in-Publication Data. https://cdn.who.int/media/docs/default-source/patient-safety/pulse-oximetry/who-ps-pulse-oxymetry-training-manual-en.pdf?sfvrsn=322cb7ae_6
Nie J, Chen W, Jia Y, Zhang Y, Wang H (2023) Comparison of remifentanil and esketamine in combination with propofol for patient sedation during fiberoptic bronchoscopy. BMC Pulm Med 23:254. https://doi.org/10.1186/s12890-023-02517-1
Ramachandran SK, Cosnowski A, Shanks A, Turner CR (2010) Apneic oxygenation during prolonged laryngoscopy in obese patients: a randomized, controlled trial of nasal oxygen administration. J Clin Anesth 22:164–168. https://doi.org/10.1016/j.jclinane.2009.05.006
Abdul-Latif MS, Putland AJ, McCluskey A, Meadows DP, Remington SA (2001) Oral midazolam premedication for day case breast surgery, a randomised prospective double-blind placebo-controlled study. Anaesthesia 56:990–994. https://doi.org/10.1046/j.1365-2044.2001.01974-2.x
Yoon S, Kim BR, Min SH, Lee J, Bahk JH, Seo JH (2021) Repeated intermittent hypoxic stimuli to operative lung reduce hypoxemia during subsequent one-lung ventilation for thoracoscopic surgery: a randomized controlled trial. PLoS ONE 16:e0249880. https://doi.org/10.1371/journal.pone.0249880
Turan A, Esa WAS, Rivas E, Wang J, Bakal O, Stamper S, Farag E, Maheswari K, Mao G, Ruetzler K, Sessler DI (2022) Tidal volume and positive end-expiratory pressure and postoperative hypoxemia during general anesthesia: a single-center multiple crossover factorial cluster trial. Anesthesiology 137:406–417. https://doi.org/10.1097/ALN.0000000000004342
Robin X, Turck N, Hainard A, Tiberti N, Lisacek F, Sanchez JC, Müller M (2011) pROC: An open-source package for R and S+ to analyze and compare ROC curves. BMC Bioinform 12:77. https://doi.org/10.1186/1471-2105-12-77
Badawy M, Béїque F, Al-Halal H, Azar T, Akkour K, Lau SK, Gotlieb WH (2011) Anesthesia considerations for robotic surgery in gynecologic oncology. J Robot Surg 5:235–239. https://doi.org/10.1007/s11701-011-0261-z
Suh MK, Seong KW, Jung SH, Kim SS (2010) The effect of pneumoperitoneum and Trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol 59:329–334. https://doi.org/10.4097/kjae.2010.59.5.329
Scheeren TWL, Belda FJ, Perel A (2018) The oxygen reserve index (ORI): a new tool to monitor oxygen therapy. J Clin Monit Comput 32:379–389. https://doi.org/10.1007/s10877-017-0049-4
Hille H, Le Thuaut A, Canet E, Lemarie J, Crosby L, Ottavy G, Garret C, Martin M, Seguin A, Lamouche-Wilquin P, Morin J (2021) Oxygen reserve index for non-invasive early hypoxemia detection during endotracheal intubation in intensive care: the prospective observational NESOI study. Ann Intensive Care 11:112. https://doi.org/10.1186/s13613-021-00903-8
Applegate RL 2nd, Dorotta IL, Wells B, Juma D, Applegate PM (2016) The relationship between oxygen reserve index and arterial partial pressure of oxygen during surgery. Anesth Analg 123:626–633. https://doi.org/10.1213/ANE.0000000000001262
Yoshida K, Isosu T, Noji Y, Hasegawa M, Iseki Y, Oishi R, Imaizumi T, Sanbe N, Obara S, Murakawa M (2018) Usefulness of oxygen reserve index (ORi™), a new parameter of oxygenation reserve potential, for rapid sequence induction of general anesthesia. J Clin Monit Comput 32:687–691. https://doi.org/10.1007/s10877-017-0068-1
Cho YJ, Jung DE, Oh Y, Nam K, Lee HC, Jeon Y, Cho YD, Kim TK (2022) Heart rate variability and oxygen reserve index during cardiorespiratory events in patients undergoing ophthalmic arterial chemotherapy: a prospective observational study. J Clin Monit Comput 36:557–567. https://doi.org/10.1007/s10877-021-00687-z
Kendale SM, Blitz JD (2016) Increasing body mass index and the incidence of intraoperative hypoxemia. J Clin Anesth 33:97–104. https://doi.org/10.1016/j.jclinane.2016.03.020
Acknowledgements
None.
Funding
Open Access funding enabled and organized by Seoul National University Hospital.
Author information
Authors and Affiliations
Contributions
JH Ryu: Data collection, data analysis, manuscript writing, and editing. YT Jeon: Study design, data collection, manuscript writing, and editing. KM Sim: Data collection, manuscript writing. SW Lee: Data analysis, manuscript writing. AY Oh: Data collection, manuscript editing. CH Koo: Study design, data analysis, manuscript writing and editing, supervision. All authors read and approve the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have nothing to declare.
Ethics approval
This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB No.: B-2305–828-101). As this was a retrospective study, the requirement for informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ryu, JH., Jeon, YT., Sim, K.M. et al. Role of oxygen reserve index monitoring in patients undergoing robot-assisted radical prostatectomy: a retrospective study. World J Urol 42, 232 (2024). https://doi.org/10.1007/s00345-024-04938-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00345-024-04938-x