Abstract
Background
To determine the utility of diagnostic 18F-DCPyL PSMA-PET/CT to aid management of men with highly suspicious multiparametric MRI prostate (PIRAD 4–5 lesions) and discrepant negative prostate biopsy.
Methods
A multicentre prospective consecutive case series was conducted (2018–2021), recruiting men with prior mpMRI prostate PIRADS 4–5 lesions and negative prostate biopsy. All men had 18F-DCPyL PSMA-PET/CT with subsequent management based on the concordance between MRI and PET: (1) Concordant lesions were biopsied using in-bore MRI targeting; (2) PSMA-PET/CT avidity without MRI correlate were biopsied using cognitive/software targeting with ultrasound guidance and (3) Patients with negative PET/CT were returned to standard of care follow-up.
Results
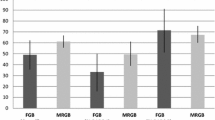
29 patients were recruited with 48% (n = 14) having concordant MRI/PET abnormalities. MRI targeted biopsy found prostate cancer in six patients, with grade groups GG3 (n = 1), GG2 (n = 1), GG1 (n = 4) found. Of the 20 men who PSMA-PET/CT avidity and biopsy, analysis showed higher SUVmax (20.1 vs 6.8, p = 0.036) predicted prostate cancer. Of patients who had PSMA-PET avidity without MRI correlate, and those with no PSMA-PET avidity, only one patient was subsequently found to have prostate cancer (GG1). The study is limited by small size and short follow-up of 17 months (IQR 12.5–29.9).
Conclusions
PSMA-PET/CT is useful in this group of men but requires further investigation. Avidity (higher SUVmax) that correlates to the mpMRI prostate lesion should be considered for targeted biopsy.
Similar content being viewed by others
Data availability
This is a small prospective case series - there is no data available to share.
References
Kasivisvanathan V, Rannikko AS, Borghi M, Panebianco V, Mynderse LA, Vaarala MH et al (2018) MRI-targeted or standard biopsy for prostate-cancer diagnosis. N Engl J Med 378(19):1767–1777
Ahmed HU, El-Shater Bosaily A, Brown LC, Gabe R, Kaplan R, Parmar MK et al (2017) Diagnostic accuracy of multi-parametric MRI and TRUS biopsy in prostate cancer (PROMIS): a paired validating confirmatory study. The Lancet 389(10071):815–822
Turkbey B, Rosenkrantz AB, Haider MA, Padhani AR, Villeirs G, Macura KJ et al (2019) Prostate imaging reporting and data system version 2.1: 2019 update of prostate imaging reporting and data system version 2. Eur Urol 76(3):340–351
Kam J, Yuminaga Y, Krelle M, Gavin D, Koschel S, Aluwihare K et al (2019) Evaluation of the accuracy of multiparametric MRI for predicting prostate cancer pathology and tumour staging in the real world: an multicentre study. BJU Int 124(2):297–301
Purysko AS, Bittencourt LK, Bullen JA, Mostardeiro TR, Herts BR, Klein EA (2017) Accuracy and interobserver agreement for prostate imaging reporting and data system, version 2, for the characterization of lesions identified on multiparametric MRI of the prostate. AJR Am J Roentgenol 209(2):339–349
Brembilla G, Dell’Oglio P, Stabile A, Damascelli A, Brunetti L, Ravelli S et al (2020) Interreader variability in prostate MRI reporting using prostate imaging reporting and data system version 2.1. Eur Radiol 30(6):3383–3392
Moldovan PC, Van den Broeck T, Sylvester R, Marconi L, Bellmunt J, van den Bergh RCN et al (2017) What is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate cancer at biopsy? A systematic review and meta-analysis from the European Association of Urology Prostate Cancer Guidelines Panel. Eur Urol 72(2):250–266
Lo G, Burton KR, Haider MA, Fleshner N, Finelli A, Ghai S (2019) Negative predictive value of prostate multiparametric magnetic resonance imaging among men with negative prostate biopsy and elevated prostate specific antigen: a clinical outcome retrospective cohort study. J Urol 202(6):1159–1165
Whish-Wilson T, Costello D, Finch S, Sutherland T, Wong LM (2020) Funding of prostate magnetic resonance imaging leads to fewer biopsies and potential savings to health systems in the management of prostate cancer: funding prostate MRI has potential savings. BJU Int. https://doi.org/10.1111/bju.15231
Tsourlakis MC, Klein F, Kluth M, Quaas A, Graefen M, Haese A et al (2015) PSMA expression is highly homogenous in primary prostate cancer. Appl Immunohistochem Amp Mol Morphol AIMM 23(6):449–455
Hofman MS, Lawrentschuk N, Francis RJ, Tang C, Vela I, Thomas P et al (2020) Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): a prospective, randomised, multicentre study. The Lancet 395(10231):1208–1216
Perera M, Papa N, Roberts M, Williams M, Udovicich C, Vela I et al (2020) Gallium-68 prostate-specific membrane antigen positron emission tomography in advanced prostate cancer—updated diagnostic utility, sensitivity, specificity, and distribution of prostate-specific membrane antigen-avid lesions: a systematic review and meta-analysis. Eur Urol 77(4):403–417
Perry E, Talwar A, Taubman K, Ng M, Wong LM, Booth R et al (2021) [18F]DCFPyL PET/CT in detection and localization of recurrent prostate cancer following prostatectomy including low PSA < 0.5 ng/mL. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-020-05143-9
Koschel S, Taubman K, Sutherland T, Yap K, Chao M, Guerrieri M et al (2021) Patterns of disease detection using [18F]DCFPyL PET/CT imaging in patients with detectable PSA post prostatectomy being considered for salvage radiotherapy: a prospective trial. Eur J Nucl Med Mol Imaging. https://doi.org/10.1007/s00259-021-05354-8
Morris MJ, Rowe SP, Gorin MA, Saperstein L, Pouliot F, Josephson D et al (2021) Diagnostic performance of 18F-DCFPyL-PET/CT in men with biochemically recurrent prostate cancer: results from the CONDOR phase III, Multicenter Study. Clin Cancer Res 27(13):3674–3682
Amin A, Blazevski A, Thompson J, Scheltema MJ, Hofman MS, Murphy D et al (2020) Protocol for the PRIMARY clinical trial, a prospective, multicentre, cross-sectional study of the additive diagnostic value of gallium-68 prostate-specific membrane antigen positron-emission tomography/computed tomography to multiparametric magnetic resonance imaging in the diagnostic setting for men being investigated for prostate cancer. BJU Int 125(4):515–524
Tran V, Hong A, Sutherland T, Taubman K, Lee SF, Lenaghan D et al (2022) PEDAL protocol: a prospective single-arm paired comparison of multiparametric MRI and 18F-DCFPyl PSMA PET/CT to diagnose prostate cancer. BMJ Open 12(9):e061815
Emmett L, Buteau J, Papa N, Moon D, Thompson J, Roberts MJ, et al (2021) The additive diagnostic value of prostate-specific membrane antigen positron emission tomography computed tomography to multiparametric magnetic resonance imaging triage in the diagnosis of prostate cancer (PRIMARY): a prospective multicentre study. Eur Urol Dec 80(6):682–689
Margel D, Bernstine H, Groshar D, Ber Y, Nezrit O, Segal N et al (2021) Diagnostic performance of 68Ga prostate-specific membrane antigen PET/MRI compared with multiparametric MRI for detecting clinically significant prostate cancer. Radiology 301(2):379–386
Berger I, Annabattula C, Lewis J, Shetty DV, Kam J, Maclean F et al (2018) 68Ga-PSMA PET/CT vs. mpMRI for locoregional prostate cancer staging: correlation with final histopathology. Prostate Cancer Prostatic Dis 21(2):204–211
Kalapara AA, Nzenza T, Pan HYC, Ballok Z, Ramdave S, O’Sullivan R et al (2020) Detection and localisation of primary prostate cancer using 68 gallium prostate-specific membrane antigen positron emission tomography/computed tomography compared with multiparametric magnetic resonance imaging and radical prostatectomy specimen pathology. BJU Int 126(1):83–90
Panicek DM, Hricak H (2016) How sure are you, doctor? A standardized lexicon to describe the radiologist’s level of certainty. Am J Roentgenol 207(1):2–3
National Cancer Institute. NCI Common Terminology Criteria for Adverse Events 2017. https://evs.nci.nih.gov/ftp1/CTCAE/About.html
Ptasznik G, Papa N, Kelly BD, Thompson J, Stricker P, Roberts MJ, et al (2022) High PSMA PET SUVmax in PI-RADS 4 or 5 men confers a high probability of significant prostate cancer. BJU Int 130 (Suppl 3):5–7
Emmett LM, Papa N, Buteau J, Ho B, Liu V, Roberts M, et al (2022) The PRIMARY Score: Using intra-prostatic PSMA PET/CT patterns to optimise prostate cancer diagnosis. J Nucl Med 63(11):1644–1650. https://doi.org/10.2967/jnumed.121.263448
Meng X, Chao B, Chen F, Huang R, Taneja SS, Deng FM (2021) Followup of men with PI-RADS™ 4 or 5 abnormality on prostate magnetic resonance imaging and nonmalignant pathological findings on initial targeted prostate biopsy. J Urol 205(3):748–754
Gaziev G, Wadhwa K, Barrett T, Koo BC, Gallagher FA, Serrao E et al (2016) Defining the learning curve for multiparametric magnetic resonance imaging (MRI) of the prostate using MRI-transrectal ultrasonography (TRUS) fusion-guided transperineal prostate biopsies as a validation tool. BJU Int 117(1):80–86
Greer MD, Shih JH, Lay N, Barrett T, Bittencourt L, Borofsky S et al (2019) Interreader variability of prostate imaging reporting and data system version 2 in detecting and assessing prostate cancer lesions at prostate MRI. Am J Roentgenol 212(6):1197–1205
Müller S, Lilleaasen G, Sand TE, Løfsgaard L, Estop-Garanto M, Helgø D et al (2018) Poor reproducibility of PIRADS score in two multiparametric MRIs before biopsy in men with elevated PSA. World J Urol 36(5):687–691
Wegelin O, van Melick HHE, Hooft L, Bosch JLHR, Reitsma HB, Barentsz JO et al (2017) Comparing three different techniques for magnetic resonance imaging-targeted prostate biopsies: a systematic review of in-bore versus magnetic resonance imaging-transrectal ultrasound fusion versus cognitive registration. Is there a preferred technique? Eur Urol 71(4):517–531
Acknowledgements
This clinical trial is supported by Cyclotek (Aust) Pty Ltd and their key partners, the Australian Government as part of its CRC Projects Program, General Electrical Healthcare and Macquarie University. Dr. Samantha Koschel is supported by a Research Training Program Scholarship from the Australian Government. We also acknowledge the support of the St Vincent’s Research Endowment fund.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Cyclotek Pty Ltd have supported authors LMW and TS in this study by providing 18F-DCPyL tracer. However they were not involved in the design, statistical analysis, interpretation of results or writing of manuscript. Unrelated to this project, LMW has received grants from Epworth Medical Foundation and consulting fees from Abbvie and AstraZeneca.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, LM., Koschel, S., Whish-Wilson, T. et al. Investigating PSMA-PET/CT to resolve prostate MRI PIRADS4-5 and negative biopsy discordance. World J Urol 41, 463–469 (2023). https://doi.org/10.1007/s00345-022-04243-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-022-04243-5