Abstract
Objective
This study aims to develop a CT-based method for quantifying tracheal shape and evaluating its ability to distinguish between cases with or without tracheal invasion in patients with thyroid carcinoma.
Methods
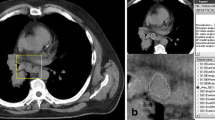
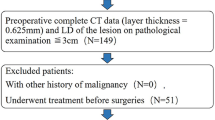
A total of 116 quantitative shape features, including 56 geometric moments and 60 bounding shape features, were defined. The tracheal lumen was semi-automatically defined with a CT threshold of less than − 500 HU. Three contiguous slices with the 1st, 2nd, and 3rd smallest trachea lumen areas were contiguously selected, and the appropriate number of slices to be included was determined. Fifty-six patients with differentiated thyroid carcinoma (DTC) invading the trachea and 22 patients with DTC but without invasion were retrospectively included. A receiver operating characteristic (ROC) curve was applied to select the representative shape features and determine the optimal threshold.
Results
23.3%, 25.9%, and 24.1% of the features displayed an area under the ROC curve (AUC) ≥ 0.800 when derived from 1, 2, and 3 slices, respectively. Calculating feature values from two slices with the 1st and 2nd smallest tracheal lumen area were considered appropriate. Six final features, including 3 geometric moments and 3 bounding shape features, were selected to determine the tracheal invasion status of DTC and displayed AUCs of 0.875–0.918, accuracies of 0.821–0.891, sensitivities of 0.813–0.893, and specificities of 0.818–0.932, outperforming the visual evaluation results.
Conclusions
Geometric moments and bounding shape features can quantify the tracheal shape and are reliable for identifying DTC tracheal invasion. The selected features quantified the extent of tracheal deformity in DTC patients with and without tracheal invasion.
Clinical relevance statement
Six geometric features provide a non-invasive, semi-automated evaluation of the tracheal invasion status of thyroid cancer.
Key Points
• A novel method for quantifying tracheal shape using 56 geometric moments and 60 bounding shape features was developed.
• Six features identify tracheal invasion by thyroid carcinoma.
• The selected features quantified the extent of tracheal deformity in differentiated thyroid carcinoma patients with and without tracheal invasion.





Similar content being viewed by others
Abbreviations
- ATA:
-
American Thyroid Association
- AUC:
-
Area under the receiver operating characteristics curve
- CT:
-
Computed tomography
- DTC:
-
Differentiated thyroid carcinoma
- MRI:
-
Magnetic resonance imaging
- PET:
-
Positron emission tomography
- ROC:
-
Receiver operating characteristics
- TNM:
-
Tumor, lymph node, metastasis staging system
References
Ito Y, Fukushima M, Yabuta T et al (2009) Local prognosis of patients with papillary thyroid carcinoma who were intra-operatively diagnosed as having minimal invasion of the trachea: a 17-year experience in a single institute. Asian J Surg 32:102–108
Kim H, Jung HJ, Lee SY et al (2016) Prognostic factors of locally invasive well-differentiated thyroid carcinoma involving the trachea. Eur Arch Otorhinolaryngol 273:1919–1926
Avenia N, Vannucci J, Monacelli M et al (2016) Thyroid cancer invading the airway: diagnosis and management. Int J Surg 28(Suppl 1):S75–S78
Kanazawa Y, Takeuchi M, Tateya I, Omori K, Kawakami K (2017) Clinical epidemiology of tracheal invasion from thyroid cancer in Japanese population: Functional outcomes and effect of aging. Cancer Epidemiol 50:107–112
Perrier ND, Brierley JD, Tuttle RM (2018) Differentiated and anaplastic thyroid carcinoma: major changes in the American Joint Committee on Cancer eighth edition cancer staging manual. CA Cancer J Clin 68:55–63
Matsumoto F, Ikeda K (2021) Surgical management of tracheal invasion by well-differentiated thyroid cancer. Cancers (Basel):13
Shimamoto K, Satake H, Sawaki A, Ishigaki T, Funahashi H, Imai T (1998) Preoperative staging of thyroid papillary carcinoma with ultrasonography. Eur J Radiol 29:4–10
Tomoda C, Uruno T, Takamura Y et al (2005) Ultrasonography as a method of screening for tracheal invasion by papillary thyroid cancer. Surg Today 35:819–822
Lee JY, Kim JH, Yeon EK et al (2022) Computed tomography complements ultrasound for the differential diagnosis of traumatic neuroma from recurrent tumor in patients with postoperative thyroid cancer. Eur Radiol 32:2760–2768
Chung SR, Baek JH, Choi YJ et al (2022) Risk factors for metastasis in indeterminate lymph nodes in preoperative patients with thyroid cancer. Eur Radiol 32:3863–3868
Lin Y, Lai S, Wang P et al (2022) Performance of current ultrasound-based malignancy risk stratification systems for thyroid nodules in patients with follicular neoplasms. Eur Radiol 32:3617–3630
Seo YL, Yoon DY, Lim KJ et al (2010) Locally advanced thyroid cancer: can CT help in prediction of extrathyroidal invasion to adjacent structures? AJR Am J Roentgenol 195:W240–W244
Griscom NT (1982) Computed tomographic determination of tracheal dimensions in children and adolescents. Radiology 145:361–364
Griscom NT (1991) CT measurement of the tracheal lumen in children and adolescents. AJR Am J Roentgenol 156:371–372
De Wever W, Vandecaveye V, Lanciotti S, Verschakelen JA (2004) Multidetector CT-generated virtual bronchoscopy: an illustrated review of the potential clinical indications. Eur Respir J 23:776–782
Beigelman-Aubry C, Brillet PY, Grenier PA (2009) MDCT of the airways: technique and normal results. Radiol Clin N Am 47:185–201
Bradski G (2000) The OpenCV library. Dr Dobb’s J Softw Tools 25:120–125
Coelho LP (2013) Mahotas: open source software for scriptable computer vision. J Open Res Softw 1:e3
Hu M (1962) Visual pattern recognition by moment invariants. IEEE Transac Inform Theory 8:179–187
Khotanzad A, Hong YH (1990) Invariant image recognition by Zernike moments. IEEE Transac Patt Analy Machine Intel 12:489–497
Kong Z, Jiang C, Liu D et al (2021) Quantitative features from CHO PET distinguish the WHO grades of primary diffuse glioma. Clin Nucl Med 46:103–110
Kong Z, Zhang Y, Liu D et al (2021) Role of traditional CHO PET parameters in distinguishing IDH, TERT and MGMT alterations in primary diffuse gliomas. Ann Nucl Med 35:493–503
Liu L, Klein SA, Xue F, Zhang JY, Yu C (2009) Using geometric moments to explain human letter recognition near the acuity limit. J Vis 9(26):21–18
Hickman MS (2011) Geometric moments and their invariants. J Math Imaging Vis 44:223–235
Mo H, Hao H, Li H (2021) Geometric moment invariants to spatial transform and N-fold symmetric blur. Pattern Recogn 115:107887
Singh C, Mittal N, Walia E (2011) Face recognition using Zernike and complex Zernike moment features. Patt Recognit Image Anal 21:71–81
Ren Y, Yang J, Zhang Q, Guo Z (2021) Ship recognition based on Hu invariant moments and convolutional neural network for video surveillance. Multimed Tools Appl 80:1343–1373
Chen S, Xia R, Zhao J, Chen Y, Hu M (2017) A hybrid method for ellipse detection in industrial images. Pattern Recogn 68:82–98
Cupec R, Vidović I, Filko D, Đurović P (2020) Object recognition based on convex hull alignment. Pattern Recogn 102:107199
Ha T, Kim W, Cha J et al (2022) Differentiating pulmonary metastasis from benign lung nodules in thyroid cancer patients using dual-energy CT parameters. Eur Radiol 32:1902–1911
Haugen BR, Alexander EK, Bible KC et al (2016) 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: The American Thyroid Association Guidelines Task Force on Thyroid Nodules and Differentiated Thyroid Cancer. Thyroid 26:1–133
Takashima S, Takayama F, Wang Q et al (2000) Differentiated thyroid carcinomas. Prediction of tumor invasion with MR imaging. Acta Radiol 41:377–383
Wang JC, Takashima S, Takayama F et al (2001) Tracheal invasion by thyroid carcinoma: prediction using MR imaging. AJR Am J Roentgenol 177:929–936
Kong Z, Li Z, Chen J et al (2022) Metabolic characteristics of [(18)F]fluoroboronotyrosine (FBY) PET in malignant brain tumors. Nuclear Med Bio 106-107:80–87
Kong Z, Li Z, Chen J et al (2022) Larger (18)F-fluoroboronotyrosine (FBY) active volume beyond MRI contrast enhancement in diffuse gliomas than in circumscribed brain tumors. EJNMMI Res 12:22
Acknowledgements
The authors thank the American Journal Experts for providing language help.
Funding
This study was supported by the National Natural Science Foundation of China (Grant No. 32301152), the Beijing Natural Science Foundation (Grant No. 7232351), the Special Research Fund for Central Universities, Peking Union Medical College (Grant No. 3332022024 and 2019XK320073), the CAMS Initiative for Innovative Medicine (Grant No. 2021-I2M-1-015), and the Beijing Hope Run Special Fund of Cancer Foundation of China (Grant No. LC2017L04).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Shaoyan Liu.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional review board (Cancer Hospital, Chinese Academy of Medical Sciences and Peking Union Medical College) approval was obtained.
Study subjects or cohorts overlap
No study subjects or cohorts have been previously reported.
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(PDF 716 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kong, Z., Wang, J., Ni, S. et al. CT-based quantification of trachea shape to detect invasion by thyroid cancer. Eur Radiol (2023). https://doi.org/10.1007/s00330-023-10301-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00330-023-10301-2