Abstract
Objectives
To assess the association between the enhancement pattern of the pancreatic parenchyma on preoperative multiphasic contrast-enhanced computed tomography (CECT) and the occurrence of postpancreatectomy acute pancreatitis (PPAP) after pancreaticoduodenectomy (PD).
Methods
A total of 513 patients who underwent PD were retrospective enrolled. The CT attenuation values of the nonenhanced (N), arterial (A), portal venous (P), and late (L) phases in the pancreatic parenchyma were measured on preoperative multiphasic CECT. The enhancement pattern was quantized by the CT attenuation value ratios in each phase. Receiver operating characteristic (ROC) curve analyses were computed to evaluate predictive performance. Regression analyses were used to identify independent risk factors for PPAP.
Results
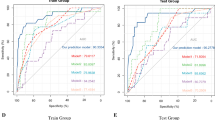
PPAP developed in 102 patients (19.9%) and was associated with increased morbidity and a worse postoperative course. The A/P ratio, P/L ratio, and A/L ratio were significantly higher in the PPAP group. On the ROC analysis, the A/L ratio and A/P ratio both performed well in predicting PPAP (A/L: AUC = 0.7579; A/P: AUC = 0.7497). On multivariate analyses, the A/L ratio > 1.29 (OR 4.30 95% CI: 2.62–7.06, p < 0.001) and A/P ratio > 1.13 (OR 5.02 95% CI: 2.98–8.45, p < 0.001) were both independent risk factors of PPAP in each model.
Conclusions
The enhancement pattern of the pancreatic parenchyma on multiphasic preoperative CECT is a good predictor of the occurrence of PPAP after PD, which could help clinicians identify high-risk patients or enable selective enhance recovery protocols.
Clinical relevance statement
Preoperative identification of patients at high risk for postpancreatectomy acute pancreatitis by enhancement patterns of the pancreatic parenchyma allows surgeons to tailor their perioperative management and take precautions.
Key Points
-
PPAP is associated with increased risk of postoperative complications and a worse postoperative course.
-
A rapid-decrease enhancement pattern of the pancreatic parenchyma is related to the occurrence of PPAP.
-
The A/L and A/P ratios were both independent risk factors of PPAP in each multivariate model.




Similar content being viewed by others
Abbreviations
- A:
-
Artery phase
- CECT:
-
Contrast-enhanced computed tomography
- CP:
-
Chronic pancreatitis
- L:
-
Later phase
- N:
-
Nonenhanced phase
- P:
-
Portal venous phase
- PDAC:
-
Pancreatic ductal adenocarcinoma
- POPF:
-
Postoperative pancreatic fistula
- PPAP:
-
Postpancreatectomy acute pancreatitis
References
Connor S (2016) Defining post-operative pancreatitis as a new pancreatic specific complication following pancreatic resection. HPB (Oxford) 18:642–651
Maggino L, Marchegiani G, Zyromski NJ, Vollmer CM, Jr. (2022) SSAT GI surgery debate: hepatobiliary and pancreas: is post-pancreatectomy acute pancreatitis a relevant clinical entity? J Gastrointest Surg 26:60-63
Loos M, Strobel O, Dietrich M et al (2021) Hyperamylasemia and acute pancreatitis after pancreatoduodenectomy: two different entities. Surgery 169:369-376
Bannone E, Andrianello S, Marchegiani G et al (2021) Postoperative hyperamylasemia (POH) and acute pancreatitis after pancreatoduodenectomy (POAP): state of the art and systematic review. Surgery 169:377-387
Kuhlbrey CM, Samiei N, Sick O, Makowiec F, Hopt UT, Wittel UA (2017) Pancreatitis after pancreatoduodenectomy predicts clinically relevant postoperative pancreatic fistula. J Gastrointest Surg 21:330-338
Bannone E, Andrianello S, Marchegiani G et al (2018) Postoperative acute pancreatitis following pancreaticoduodenectomy: a determinant of fistula potentially driven by the intraoperative fluid management. Ann Surg 268:815-822
Ryska M, Rudis J (2014) Pancreatic fistula and postoperative pancreatitis after pancreatoduodenectomy for pancreatic cancer. Hepatobiliary Surg Nutr 3:268-275
Marchegiani G, Barreto SG, Bannone E et al (2022) Postpancreatectomy acute pancreatitis (PPAP): definition and grading from the International Study Group for Pancreatic Surgery (ISGPS). Ann Surg 275:663-672
Chen H, Wang C, Shen Z et al (2023) Post-pancreatectomy acute pancreatitis after pancreaticoduodenectomy: a distinct clinical entity. Ann Surg 278:e278–e283
Hashimoto Y, Sclabas GM, Takahashi N et al (2011) Dual-phase computed tomography for assessment of pancreatic fibrosis and anastomotic failure risk following pancreatoduodenectomy. J Gastrointest Surg 15:2193-2204
Shi Y, Gao F, Qi Y et al (2020) Computed tomography-adjusted fistula risk score for predicting clinically relevant postoperative pancreatic fistula after pancreatoduodenectomy: training and external validation of model upgrade. EBioMedicine 62:103096
Tang B, Lin Z, Ma Y et al (2021) A modified alternative fistula risk score (a-FRS) obtained from the computed tomography enhancement pattern of the pancreatic parenchyma predicts pancreatic fistula after pancreatoduodenectomy. HPB (Oxford) 23:1759-1766
Maehira H, Iida H, Mori H et al (2019) Computed tomography enhancement pattern of the pancreatic parenchyma predicts postoperative pancreatic fistula after pancreaticoduodenectomy. Pancreas 48:209-215
Chen H, Wang W, Ying X et al (2020) Predictive factors for postoperative pancreatitis after pancreaticoduodenectomy: a single-center retrospective analysis of 1465 patients. Pancreatology 20:211-216
Takahashi N, Fletcher JG, Hough DM et al (2009) Autoimmune pancreatitis: differentiation from pancreatic carcinoma and normal pancreas on the basis of enhancement characteristics at dual-phase CT. AJR Am J Roentgenol 193:479-484
Schanaider A, de Carvalho TP, de Oliveira Coelho S et al (2015) Ischemia-reperfusion rat model of acute pancreatitis: protein carbonyl as a putative early biomarker of pancreatic injury. Clin Exp Med 15:311-320
Doussot A, Decrock M, Calame P et al (2021) Fluorescence-based pancreas stump perfusion is associated with postoperative acute pancreatitis after pancreatoduodenectomy a prospective cohort study. Pancreatology. https://doi.org/10.1016/j.pan.2021.05.009
Schuh F, Mihaljevic AL, Probst P et al (2023) A simple classification of pancreatic duct size and texture predicts postoperative pancreatic fistula: a classification of the International Study Group of Pancreatic Surgery. Ann Surg 277:e597-e608
Bassi C, Marchegiani G, Dervenis C et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 years after. Surgery 161:584-591
Dindo D, Demartines N, Clavien PA (2004) Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg 240:205-213
Fluss R, Faraggi D, Reiser B (2005) Estimation of the Youden Index and its associated cutoff point. Biom J 47:458-472
Cappelli C, Boggi U, Mazzeo S et al (2015) Contrast enhancement pattern on multidetector CT predicts malignancy in pancreatic endocrine tumours. Eur Radiol 25:751-759
Ren A, Cai F, Shang YN et al (2015) Differentiation of renal oncocytoma and renal clear cell carcinoma using relative CT enhancement ratio. Chin Med J (Engl) 128:175-179
Kim SJ, Lee JM, Lee JY et al (2008) Analysis of enhancement pattern of flat gallbladder wall thickening on MDCT to differentiate gallbladder cancer from cholecystitis. AJR Am J Roentgenol 191:765-771
Kim SA, Lee JM, Lee KB et al (2011) Intrahepatic mass-forming cholangiocarcinomas: enhancement patterns at multiphasic CT, with special emphasis on arterial enhancement pattern--correlation with clinicopathologic findings. Radiology 260:148-157
Park VY, Choi JY, Chung YE et al (2014) Dynamic enhancement pattern of HCC smaller than 3 cm in diameter on gadoxetic acid-enhanced MRI: comparison with multiphasic MDCT. Liver Int 34:1593-1602
Shin DW, Park J, Lee JC, Kim J, Kim YH, Hwang JH (2022) Multi-phase, contrast-enhanced computed tomography-based radiomic prognostic marker of non-metastatic pancreatic ductal adenocarcinoma. Cancers (Basel) 14
Nahm CB, Lui I, Naidoo CS et al (2019) Density and enhancement of the pancreatic tail on computer tomography predicts acinar score and pancreatic fistula after pancreatoduodenectomy. HPB (Oxford) 21:604-611
Shi HY, Lu ZP, Li MN, Ge YQ, Jiang KR, Xu Q (2022) Dual-energy CT iodine concentration to evaluate postoperative pancreatic fistula after pancreatoduodenectomy. Radiology 304:65-72
McGuire SP, Maatman TK, Keller SL et al (2022) Early postoperative serum hyperamylasemia: harbinger of morbidity hiding in plain sight? Surgery 171:469-475
Laaninen M, Sand J, Nordback I, Vasama K, Laukkarinen J (2016) Perioperative hydrocortisone reduces major complications after pancreaticoduodenectomy: a randomized controlled trial. Ann Surg 264:696-702
Andrianello S, Bannone E, Marchegiani G et al (2021) Characterization of postoperative acute pancreatitis (POAP) after distal pancreatectomy. Surgery 169:724-731
Partelli S, Andreasi V, Schiavo Lena M et al (2021) The role of acinar content at pancreatic resection margin in the development of postoperative pancreatic fistula and acute pancreatitis after pancreaticoduodenectomy. Surgery 170:1215-1222
Hattori Y, Gabata T, Matsui O et al (2009) Enhancement patterns of pancreatic adenocarcinoma on conventional dynamic multi-detector row CT: correlation with angiogenesis and fibrosis. World J Gastroenterol 15:3114-3121
Sugimoto M, Takahashi S, Kobayashi T et al (2015) Pancreatic perfusion data and post-pancreaticoduodenectomy outcomes. J Surg Res 194:441-449
Cuthbertson CM, Christophi C (2006) Disturbances of the microcirculation in acute pancreatitis. Br J Surg 93:518-530
Acknowledgements
The authors would like to thank Weimin Chai, Naiyi Zhu, and Qingrou Wang from the Department of Radiology for helpful interpretation of postoperative images through the MDT meetings.
Funding
This study has received funding by Yangfan Project of Science and Technology Commission of Shanghai Municipality (22YF1442400); and Research Fund of Tongren Hospital, Shanghai Jiao Tong University School of Medicine (TRKYRC-XX202204). They played no role in the study design, data collection or analysis, decision to publish, or manuscript preparation.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Baiyong Shen.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained by Ruijin Hospital Ethics Committee.
Study subjects or cohorts overlap
Some study subjects or cohorts have been previously reported in a prior study entitled “Post-pancreatectomy Acute Pancreatitis after Pancreaticoduodenectomy: A Distinct Clinical Entity.” on Annal of Surgery, doi: 10.1097/SLA.0000000000005605
Methodology
-
retrospective
-
observational
-
performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, H., Fu, N., Zhong, J. et al. Enhancement pattern of the pancreatic parenchyma predicts postpancreatectomy acute pancreatitis after pancreaticoduodenectomy. Eur Radiol 34, 6–15 (2024). https://doi.org/10.1007/s00330-023-09927-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09927-z