Abstract
Objectives
This study aimed to evaluate the effect of achievable td on the accuracy of microstructural mapping based on simulation and patient experiments, and investigate the feasibility of td-dMRI in distinguishing prognostic factors in breast cancer patients.
Methods
Simulation was performed using different td settings. Patients with breast cancer were enrolled prospectively between November 2020 and January 2021, who underwent oscillating and pulsed gradient encoded dMRI on a 3-T scanner using short-/long-td protocol with oscillating frequency up to 50/33 Hz. Data were fitted with a two-compartment model to estimate cell diameter (d), intracellular fraction (fin), and diffusivities. Estimated microstructural markers were used to differentiate immunohistochemical receptor status and the presence of lymph node (LN), which were correlated with histopathological measurements.
Results
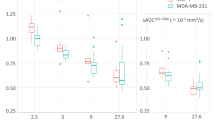
Simulation results showed that d fitted from the short-td protocol significantly reduced estimation error than those from long-td (2.07 ± 1.51% versus 3.05 ± 1.92%, p < 0.0001) while the estimation error of fin was robust to different protocols. Among a total of 37 breast cancer patients, the estimated d was significantly higher in HER2-positive and LN-positive (p < 0.05) groups compared to their negative counterparts only using the short-td protocol. Histopathological validation in a subset of 6 patients with whole slide images showed the estimated d was highly correlated with measurements from H&E staining (r = 0.84, p = 0.03) only using the short-td protocol.
Conclusions
The results indicated the necessity of short-td for accurate microstructural mapping in breast cancer. The current td-dMRI with a total acquisition time of 4.5 min showed its potential in the diagnosis of breast cancer.
Key Points
• Short t d is important for accurate microstructural mapping in breast cancer using the t d -dMRI technique, based on simulation and histological validation.
• The 4.5-min t d -dMRI protocol showed potential clinical value for breast cancer, given the difference in cell diameter between HER2/LN positive and negative groups.





Similar content being viewed by others
Abbreviations
- cGAN:
-
Conditional generative adversarial networks
- DBSI:
-
Diffusion basis spectrum imaging
- DKI:
-
Diffusion kurtosis imaging
- dMRI:
-
Diffusion MRI
- ER:
-
Estrogen receptor
- HER2:
-
Human epidermal growth factor receptor 2
- IHC:
-
Immunohistochemical
- IMPULSED:
-
Imaging microstructural parameters using limited spectrally edited diffusion
- OGSE:
-
Oscillating gradients spin-echo
- PGSE:
-
Pulsed gradients spin-echo
- POMACE:
-
Pulsed and oscillating gradient MRI for assessment of cell size and extracellular space
- PR:
-
Progesterone receptor
- VERDICT:
-
Vascular, extracellular, and restricted diffusion for cytometry in tumors
- WSI:
-
Whole slide image
References
Perou CM, Sørlie T, Eisen MB et al (2000) Molecular portraits of human breast tumours. Nature 406:747–752
Goldhirsch A, Wood WC, Gelber RD, et al. (2003) Meeting highlights: updated international expert consensus on the primary therapy of early breast cancer. J Clin Oncol 21(17):3357–3365
Eifel P, Axelson JA, Costa J et al (2001) National Institutes of Health Consensus Development Conference Statement: adjuvant therapy for breast cancer, November 1–3, 2000. J Natl Cancer Inst 93:979–989
Nielsen TO, Hsu FD, Jensen K et al (2004) Immunohistochemical and clinical characterization of the basal-like subtype of invasive breast carcinoma. Clin Cancer Res 10:5367–5374
Blows FM, Driver KE, Schmidt MK et al (2010) Subtyping of breast cancer by immunohistochemistry to investigate a relationship between subtype and short and long term survival: a collaborative analysis of data for 10,159 cases from 12 studies. PLoS Med 7:e1000279
Goldhirsch A, Wood WC, Coates AS, Gelber RD, Thürlimann B, Senn HJ (2011) Strategies for subtypes–dealing with the diversity of breast cancer: highlights of the St. Gallen International Expert Consensus on the Primary Therapy of Early Breast Cancer 2011. Ann Oncol 22:1736–1747
Martincich L, Deantoni V, Bertotto I et al (2012) Correlations between diffusion-weighted imaging and breast cancer biomarkers. Eur Radiol 22:1519–1528
Iima M, Honda M, Sigmund EE, OhnoKishimoto A, Kataoka M, Togashi K (2020) Diffusion MRI of the breast: current status and future directions. J Magn Reson Imaging 52:70–90
Horvat JV, Bernard-Davila B, Helbich TH et al (2019) Diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) mapping as a quantitative imaging biomarker for prediction of immunohistochemical receptor status, proliferation rate, and molecular subtypes of breast cancer. J Magn Reson Imaging 50:836–846
Partridge SC, Zhang Z, Newitt DC et al (2018) Diffusion-weighted MRI findings predict pathologic response in neoadjuvant treatment of breast cancer: The ACRIN 6698 multicenter trial. Radiology 289(3):618–627
Kamitani T, Matsuo Y, Yabuuchi H et al (2013) Correlations between apparent diffusion coefficient values and prognostic factors of breast cancer. Magn Reson Med Sci 12:193–199
Aydin H, Guner B, EsenBostanci I et al (2018) Is there any relationship between adc values of diffusion-weighted imaging and the histopathological prognostic factors of invasive ductal carcinoma? Br J Radiol 91:20170705
Tezcan Ş, Uslu N, Öztürk FU, Akçay EY, Tezcaner T (2019) Diffusion-weighted imaging of breast cancer: correlation of the apparent diffusion coefficient value with pathologic prognostic factors. Eur J Breast Health 15:262–267
Jiang X, Li H, Xie J et al (2017) In vivo imaging of cancer cell size and cellularity using temporal diffusion spectroscopy. Magn Reson Med 78(1):156–164
Xu J, Jiang X, Li H et al (2020) Magnetic resonance imaging of mean cell size in human breast tumors. Magn Reson Med 83:2002–2014
Panagiotaki E, Walker-Samuel S, Siow B et al (2014) Noninvasive quantification of solid tumor microstructure using VERDICT MRI. Cancer Res 74:1902–1912
Reynaud O, Winters KV, Hoang DM, Wadghiri YZ, Novikov DS, Kim SG (2016) Pulsed and oscillating gradient MRI for assessment of cell size and extracellular space (POMACE) in mouse gliomas. NMR Biomed 29:1350–1363
Xu J, Does MD, Gore JC (2009) Quantitative characterization of tissue microstructure with temporal diffusion spectroscopy. J Magn Reson 200:189–197
Cohen Y, Assaf Y (2002) High b-value q-space analyzed diffusion-weighted MRS and MRI in neuronal tissues - a technical review. NMR Biomed 15:516–542
Senn N, Masannat Y, Husain E, Siow B, Heys SD, He J (2019) q-Space imaging yields a higher effect gradient to assess cellularity than conventional diffusion-weighted imaging methods at 3.0 T: a pilot study with freshly excised whole-breast tumors. Radiol Imaging Cancer 1:e190008
Reynaud O (2017) Time-dependent diffusion MRI in cancer: Tissue modeling and applications. Front Phys 5. https://doi.org/10.3389/fphy.2017.00058
Stepišnik J (1993) Time-dependent self-diffusion by NMR spin-echo. Physica B 183:343–350
Gore JC, Xu J, Colvin DC, Yankeelov TE, Parsons EC, Does MD (2010) Characterization of tissue structure at varying length scales using temporal diffusion spectroscopy. NMR Biomed 23:745–756
Colvin DC, Yankeelov TE, Does MD, Yue Z, Quarles C, Gore JC (2008) New insights into tumor microstructure using temporal diffusion spectroscopy. Cancer Res 68:5941–5947
Panagiotaki E, Walker-Samuel S, Siow B et al (2014) Noninvasive quantification of solid tumor microstructure using VERDICT MRI. Can Res 74:1902–1912
Jiang X, Li H, Xie J, Zhao P, Gore JC, Xu J (2016) Quantification of cell size using temporal diffusion spectroscopy. Magn Reson Med 75:1076–1085
Wu D, Jiang K, Li H et al (2022) Time-dependent diffusion MRI for quantitative microstructural mapping of prostate cancer. Radiology 303:578–587
Iima M, Kataoka M, Honda M et al (2021) The rate of apparent diffusion coefficient change with diffusion time on breast diffusion-weighted imaging depends on breast tumor types and molecular prognostic biomarker expression. Invest Radiol 56(8):501–508
Solomon E, Lemberskiy G, Baete S et al (2022) DTime-dependent diffusivity and kurtosis in phantoms and patients with head and neck cancer. Magn Reson Med 89(2):522–535
Gore JC, Xu J, Colvin DC, et al (2010) Characterization of tissue structure at varying length scales using temporal diffusion spectroscopy. NMR Biomed 23:745–756
Baron CA, Beaulieu C (2014) Oscillating gradient spin-echo (OGSE) diffusion tensor imaging of the human brain. Magn Reson Med 72:726–736
Cook PA, Bai Y, Nedjati-Gilani S et al (2006) Camino: open-source diffusion-MRI reconstruction and processing. 14th Scientific Meeting of the International Society for Magnetic Resonance in Medicine, Seattle, WA, USA, p 2759, May 2006
Vranes V, Rajković N, Li X et al (2019) Size and shape filtering of malignant cell clusters within breast tumors identifies scattered individual epithelial cells as the most valuable histomorphological clue in the prognosis of distant metastasis risk. Cancers (Basel) 11(10):1615
Li H, Jiang X, Xie J et al (2017) Impact of transcytolemmal water exchange on estimates of tissue microstructural properties derived from diffusion MRI. Magn Reson Med 77(6):2239–224977
Fujii T, Kogawa T, Dong W et al (2017) Revisiting the definition of estrogen receptor positivity in HER2-negative primary breast cancer. Ann Oncol 28:2420–2428
Gradishar WJ, Anderson BO, Abraham J et al (2020) Breast Cancer, Version 3.2020, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 18:452–478
Isola P, Zhu J-Y, Zhou T, Efros A (2017) Image-to-image translation with conditional adversarial networks 2017 IEEE Conference on Computer Vision and Pattern Recognition (CVPR), Honolulu, HI, USA, 2017, pp 5967–5976
Sastre-Garau X, Genin P, Rousseau A et al (2004) Increased cell size and Akt activation in HER-2/neu-overexpressing invasive ductal carcinoma of the breast. Histopathology 45:142–147
Macchini M, Ponziani M, Iamurri AP et al (2018) Role of DCE-MR in predicting breast cancer subtypes. Radiol Med (Torino) 123:753–764
Park SH, Choi H-Y, Hahn SY (2015) Correlations between apparent diffusion coefficient values of invasive ductal carcinoma and pathologic factors on diffusion weighted MRI at 3.0 Tesla. J Magn Reson Imaging 41(1):175–82
Choi SY, Chang YW, Park HJ, Kim HJ, Hong SS, Seo DY (2012) Correlation of the apparent diffusion coefficiency values on diffusion-weighted imaging with prognostic factors for breast cancer. Br J Radiol 85:e474-479
Kitajima K, Yamano T, Fukushima K et al (2016) Correlation of the SUVmax of FDG-PET and ADC values of diffusion-weighted MR imaging with pathologic prognostic factors in breast carcinoma. Eur J Radiol 85:943–949
Nakajo M, Kajiya Y, Kaneko T et al (2010) FDG PET/CT and diffusion-weighted imaging for breast cancer: prognostic value of maximum standardized uptake values and apparent diffusion coefficient values of the primary lesion. Eur J Nucl Med Mol Imaging 37:2011–2020
Kim SH, Cha ES, Kim HS et al (2009) Diffusion-weighted imaging of breast cancer: Correlation of the apparent diffusion coefficient value with prognostic factors. J Magn Reson Imag 30:615–620
Cho GY, Moy L, Kim SG et al (2016) Evaluation of breast cancer using intravoxel incoherent motion (IVIM) histogram analysis: comparison with malignant status, histological subtype, and molecular prognostic factors. Eur Radiol 26:2547–2558
Liang J, Zeng S, Li Z et al (2020) Intravoxel incoherent motion diffusion-weighted imaging for quantitative differentiation of breast tumors: a meta-analysis. Front Oncol 10:585486
Kang HS, Kim JY, Kim JJ et al (2022) Diffusion kurtosis MR imaging of invasive breast cancer: correlations with prognostic factors and molecular subtypes. J Magn Reson Imaging 56:110–120
Wang W, Zhang X, Zhu L et al (2022) Prediction of prognostic factors and genotypes in patients with breast cancer using multiple mathematical models of MR diffusion imaging. Front Oncol 12:825264
Qin Y, Tang C, Hu Q et al (2023) Quantitative assessment of restriction spectrum MR imaging for the diagnosis of breast cancer and association with prognostic factors. J Magn Reson Imag. https://doi.org/10.1002/jmri.28468
Jones DK, Knösche TR, Turner R (2013) White matter integrity, fiber count, and other fallacies: the do’s and don’ts of diffusion MRI. Neuroimage 73:239–254
Montemurro F, Martincich L, Sarotto I et al (2007) Relationship between DCE-MRI morphological and functional features and histopathological characteristics of breast cancer. Eur Radiol 17:1490–1497
Acknowledgements
This work is supported by the Ministry of Science and Technology of the People’s Republic of China (2018YFE0114600), the National Natural Science Foundation of China (61801424, 81971606, and 82122032), the Science and Technology Department of Zhejiang Province (2020R01003 and 2022C03057), the Natural Science Foundation of Chongqing municipality (cstc2021jcyj-msxmX0387), Medical Scientific Research Project of Chongqing Municipal Health Commission (2022WSJK027), and the 2021 SKY Imaging Research Fund of the Chinese International Medical Foundation (Z-2014-07-2101).
Funding
This study has received funding from the Ministry of Science and Technology of the People’s Republic of China (2018YFE0114600), the National Natural Science Foundation of China (61801424, 81971606, and 82122032), the Science and Technology Department of Zhejiang Province (2020R01003 and 2022C03057), the Natural Science Foundation of Chongqing municipality (cstc2021jcyj-msxmX0387), Medical Scientific Research Project of Chongqing Municipal Health Commission (2022WSJK027), and the 2021 SKY Imaging Research Fund of the Chinese International Medical Foundation (Z-2014–07-2101).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantors of this publication are Dan Wu and Jiuquan Zhang.
Conflict of interest
The authors Qing Li and Yi Sun are employees of the Siemens Healthineers Ltd. (Shangai, China). These authors were not involved in data collection and/or management in any way that would influence the study. The remaining authors declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Not applicable.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ba, R., Wang, X., Zhang, Z. et al. Diffusion-time dependent diffusion MRI: effect of diffusion-time on microstructural mapping and prediction of prognostic features in breast cancer. Eur Radiol 33, 6226–6237 (2023). https://doi.org/10.1007/s00330-023-09623-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-023-09623-y