Abstract
Objectives
New PET data-processing tools allow for automatic lesion selection and segmentation by a convolution neural network using artificial intelligence (AI) to obtain total metabolic tumor volume (TMTV) and total lesion glycolysis (TLG) routinely at the clinical workstation. Our objective was to evaluate an AI implemented in a new version of commercial software to verify reproducibility of results and time savings in a daily workflow.
Methods
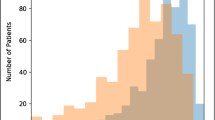
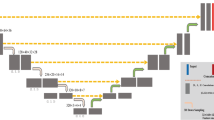
Using the software to obtain TMTV and TLG, two nuclear physicians applied five methods to retrospectively analyze data for 51 patients. Methods 1 and 2 were fully automated with exclusion of lesions ≤ 0.5 mL and ≤ 0.1 mL, respectively. Methods 3 and 4 were fully automated with physician review. Method 5 was semi-automated and used as reference. Time and number of clicks to complete the measurement were recorded for each method. Inter-instrument and inter-observer variation was assessed by the intra-class coefficient (ICC) and Bland-Altman plots.
Results
Between methods 3 and 5, for the main user, the ICC was 0.99 for TMTV and 1.0 for TLG. Between the two users applying method 3, ICC was 0.97 for TMTV and 0.99 for TLG. Mean processing time (± standard deviation) was 20 s ± 9.0 for method 1, 178 s ± 125.7 for method 3, and 326 s ± 188.6 for method 5 (p < 0.05).
Conclusion
AI-enabled lesion detection software offers an automated, fast, reliable, and consistently performing tool for obtaining TMTV and TLG in a daily workflow.
Key Points
• Our study shows that artificial intelligence lesion detection software is an automated, fast, reliable, and consistently performing tool for obtaining total metabolic tumor volume and total lesion glycolysis in a daily workflow.





Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.Abbreviations
- AI:
-
Artificial intelligence
- CIER :
-
Internal Ethics and Research Committee
- CNN:
-
Convolution neural network
- DICOM:
-
Digital Imaging and COmmunications in Medicine
- DLBCL :
-
Diffuse large cell lymphoma
- FDG :
-
Fluorodeoxyglucose
- GHICL:
-
Groupement des Hôpitaux de l'Institut Catholique de Lille
- ICC :
-
Intra-class correlation coefficient
- ICL:
-
Institut Catholique de Lille
- IPI:
-
International Prognostic Index
- MIP:
-
Maximum intensity projection
- NCCN-IPI:
-
National Comprehensive Cancer Network- International Prognostic Index
- NHL:
-
Non-Hodgkin’s lymphoma
- PERCIST :
-
PET response criteria in solid tumors
- PET:
-
Positron emission tomography
- PFS:
-
Progression-free survival
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- SUV:
-
Standardized uptake value
- TLG:
-
Total lesion glycolysis
- TMTV:
-
Total metabolic tumor volume
References
Flodr P, Latalova P, Tichy M, et al (2014) Diffuse large B-cell lymphoma: the history, current view and new perspectives. Neoplasma 62:491–504. https://doi.org/10.4149/neo_2014_062
Cottereau A-S, Lanic H, Mareschal S et al (2016) Molecular profile and FDG-PET/CT total metabolic tumor volume improve risk classification at diagnosis for patients with diffuse large B-cell lymphoma. Clin Cancer Res 22:3801–3809. https://doi.org/10.1158/1078-0432.CCR-15-2825
Shagera QA, Cheon GJ, Koh Y et al (2019) Prognostic value of metabolic tumour volume on baseline 18F-FDG PET/CT in addition to NCCN-IPI in patients with diffuse large B-cell lymphoma: further stratification of the group with a high-risk NCCN-IPI. Eur J Nucl Med Mol Imaging 46:1417–1427. https://doi.org/10.1007/s00259-019-04309-4
Wight JC, Chong G, Grigg AP, Hawkes EA (2018) Prognostication of diffuse large B-cell lymphoma in the molecular era: moving beyond the IPI. Blood Rev 32:400–415. https://doi.org/10.1016/j.blre.2018.03.005
Nowakowski GS, Feldman T, Rimsza LM et al (2019) Integrating precision medicine through evaluation of cell of origin in treatment planning for diffuse large B-cell lymphoma. Blood Cancer J 9:48. https://doi.org/10.1038/s41408-019-0208-6
Barrington SF, Mikhaeel NG, Kostakoglu L et al (2014) Role of imaging in the staging and response assessment of lymphoma: Consensus of the International Conference on Malignant Lymphomas Imaging Working Group. J Clin Oncol 32:3048–3058. https://doi.org/10.1200/JCO.2013.53.5229
Vercellino L, Cottereau A-S, Casasnovas O et al (2020) High total metabolic tumor volume at baseline predicts survival independent of response to therapy. Blood 135:1396–1405. https://doi.org/10.1182/blood.2019003526
Schindelin J, Arganda-Carreras I, Frise E et al (2012) Fiji - an Open Source platform for biological image analysis. Nat Methods 9. https://doi.org/10.1038/nmeth.2019
Barrington SF, Zwezerijnen BGJC, de Vet HCW et al (2021) Automated segmentation of baseline metabolic total tumor burden in diffuse large B-cell lymphoma: which method is most successful? A Study on Behalf of the PETRA Consortium. J Nucl Med 62:332–337. https://doi.org/10.2967/jnumed.119.238923
Ilyas H, Mikhaeel NG, Dunn JT et al (2018) Defining the optimal method for measuring baseline metabolic tumour volume in diffuse large B cell lymphoma. Eur J Nucl Med Mol Imaging 45:1142–1154. https://doi.org/10.1007/s00259-018-3953-z
Barrington SF, Meignan M (2019) Time to prepare for risk adaptation in lymphoma by standardizing measurement of metabolic tumor burden. J Nucl Med 60:1096–1102. https://doi.org/10.2967/jnumed.119.227249
Sibille L, Seifert R, Avramovic N et al (2020) 18F-FDG PET/CT uptake classification in lymphoma and lung cancer by using deep convolutional neural networks. Radiology 294:445–452. https://doi.org/10.1148/radiol.2019191114
Hans CP, Weisenburger DD, Greiner TC et al (2004) Confirmation of the molecular classification of diffuse large B-cell lymphoma by immunohistochemistry using a tissue microarray. Blood 103:275–282. https://doi.org/10.1182/blood-2003-05-1545
Wahl RL, Jacene H, Kasamon Y, Lodge MA (2009) From RECIST to PERCIST: evolving considerations for PET response criteria in solid tumors. J Nucl Med 50:122S–150S. https://doi.org/10.2967/jnumed.108.057307
Meignan M, Sasanelli M, Casasnovas RO et al (2014) Metabolic tumour volumes measured at staging in lymphoma: methodological evaluation on phantom experiments and patients. Eur J Nucl Med Mol Imaging 41:1113–1122. https://doi.org/10.1007/s00259-014-2705-y
Boellaard R, Delgado-Bolton R, Oyen WJG et al (2015) FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging 42:328–354. https://doi.org/10.1007/s00259-014-2961-x
Guo B, Tan X, Ke Q, Cen H (2019) Prognostic value of baseline metabolic tumor volume and total lesion glycolysis in patients with lymphoma: a meta-analysis. PLoS One 14:e0210224. https://doi.org/10.1371/journal.pone.0210224
Blanc-Durand P, Jégou S, Kanoun S et al (2021) Fully automatic segmentation of diffuse large B cell lymphoma lesions on 3D FDG-PET/CT for total metabolic tumour volume prediction using a convolutional neural network. Eur J Nucl Med Mol Imaging 48:1362–1370. https://doi.org/10.1007/s00259-020-05080-7
Tout M, Casasnovas O, Meignan M et al (2017) Rituximab exposure is influenced by baseline metabolic tumor volume and predicts outcome of DLBCL patients: a Lymphoma Study Association report. Blood 129:2616–2623. https://doi.org/10.1182/blood-2016-10-744292
Capobianco N, Meignan M, Cottereau A-S et al (2021) Deep-learning 18F-FDG uptake classification enables total metabolic tumor volume estimation in diffuse large B-cell lymphoma. J Nucl Med 62:30–36. https://doi.org/10.2967/jnumed.120.242412
Pinochet P, Eude F, Becker S et al (2021) Evaluation of an automatic classification algorithm using convolutional neural networks in oncological positron emission tomography. Front Med (Lausanne) 8:628179. https://doi.org/10.3389/fmed.2021.628179
Burggraaff CN, Rahman F, Kaßner I et al (2020) Optimizing workflows for fast and reliable metabolic tumor volume measurements in diffuse large B cell lymphoma. Mol Imaging Biol 22:1102–1110. https://doi.org/10.1007/s11307-020-01474-z
Nguyen NC, Vercher-Conejero J, Faulhaber P (2019) Tumor volume delineation: a pilot study comparing a digital positron-emission tomography prototype with an analog positron-emission tomography system. World J Nucl Med 18:45–51. https://doi.org/10.4103/wjnm.WJNM_22_18
de Jong TL, Koopman D, van Dalen JA et al (2022) Performance of digital PET/CT compared with conventional PET/CT in oncologic patients: a prospective comparison study. Ann Nucl Med 36:756–764. https://doi.org/10.1007/s12149-022-01758-0
Koopman D, van Dalen JA, Stevens H et al (2020) Performance of digital PET compared with high-resolution conventional PET in patients with cancer. J Nucl Med 61:1448–1454. https://doi.org/10.2967/jnumed.119.238105
Cottereau A-S, Buvat I, Kanoun S et al (2018) Is there an optimal method for measuring baseline metabolic tumor volume in diffuse large B cell lymphoma? Eur J Nucl Med Mol Imaging 45:1463–1464. https://doi.org/10.1007/s00259-018-4005-4
Sun R, Deutsch E, Fournier L (2022) Intelligence artificielle et imagerie médicale. Bull Cancer 109:83–88. https://doi.org/10.1016/j.bulcan.2021.09.009
Iacoboni G, Simó M, Villacampa G et al (2021) Prognostic impact of total metabolic tumor volume in large B-cell lymphoma patients receiving CAR T-cell therapy. Ann Hematol 100:2303–2310. https://doi.org/10.1007/s00277-021-04560-6
Schmidkonz C, Cordes M, Schmidt D et al (2018) 68Ga-PSMA-11 PET/CT-derived metabolic parameters for determination of whole-body tumor burden and treatment response in prostate cancer. Eur J Nucl Med Mol Imaging 45:1862–1872. https://doi.org/10.1007/s00259-018-4042-z
Capobianco N, Sibille L, Chantadisai M et al (2022) Whole-body uptake classification and prostate cancer staging in 68Ga-PSMA-11 PET/CT using dual-tracer learning. Eur J Nucl Med Mol Imaging 49:517–526. https://doi.org/10.1007/s00259-021-05473-2
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Mourtaza Karimdjee.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
One of the authors has significant statistical expertise. No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study. Written informed consent was waived by the Institutional Review Board.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Methodology
• retrospective
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Karimdjee, M., Delaby, G., Huglo, D. et al. Evaluation of a convolution neural network for baseline total tumor metabolic volume on [18F]FDG PET in diffuse large B cell lymphoma. Eur Radiol 33, 3386–3395 (2023). https://doi.org/10.1007/s00330-022-09375-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-09375-1