Abstract
Objective
This study compared the performance between ultrasound (US)- and contrast-enhanced US (CEUS)–guided liver biopsies and evaluated the benefit of CEUS in percutaneous biopsy for focal liver lesions (FLLs).
Methods
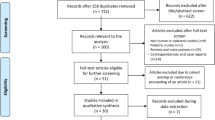
We performed a retrospective study of 820 patients with FLLs, who underwent percutaneous liver biopsy in our center between 2017 and 2019. The patients were divided into two groups based on whether US (n = 362) or CEUS (n = 458) used before a biopsy. The two groups were compared based on specimen adequacy for pathological diagnosis and diagnostic accuracy of liver biopsy. Stratification analysis was performed based on lesion and protocol characteristics to provide detailed information for selecting the imaging guidance for biopsy.
Results
Compared with the US group, the CEUS group yielded more acceptable samples (97.6% vs. 99.4%, p < 0.05) and improved diagnostic accuracy (92.6% vs. 96.4%, p < 0.05), and achieved better sensitivity (92.5% vs. 96.2%, p < 0.05) for liver biopsies, especially in FLLs ≥ 5 cm, heterogeneous hypoechoic FLLs, or FLLs with an obscure boundary. The CEUS group showed significantly higher accuracy compared with the US group pertaining to single-puncture biopsies (100% vs. 92.7%, p < 0.05) or biopsies with punctures ≤ 2 (97.6% vs. 94.3%, p < 0.05).
Conclusion
CEUS achieved an enhanced success rate for sampling and diagnostic accuracy of liver biopsies, especially in FLLs ≥ 5 cm, heterogeneous hypoechoic FLLs, or FLLs with an obscure boundary. CEUS can be used to decrease the number of punctures needed, which might increase the safety of liver biopsy.
Key Points
• CEUS can help confirm an adequate biopsy site, increasing the sampling success rate and diagnostic accuracy of the liver biopsy.
• CEUS can be used to decrease the number of punctures needed to improve the safety of liver biopsy.
• It is recommended to use CEUS guidance for liver biopsies, especially with FLLs ≥ 5 cm, heterogeneous hypoechoic FLLs, or FLLs with an obscure boundary.





Similar content being viewed by others
Abbreviations
- AFSUMB:
-
Asian Federation of Societies for Ultrasound in Medicine and Biology
- CDFI:
-
Color Doppler flow imaging
- CEUS:
-
Contrast-enhanced ultrasound
- CT:
-
Computed tomography
- EFSUMB:
-
European Federation of Societies for Ultrasound in Medicine and Biology
- FLLs:
-
Focal liver lesions
- FNH:
-
Focal nodular hyperplasia
- HCC:
-
Hepatocellular carcinoma
- ICC:
-
Intrahepatic cholangiocarcinoma
- M:
-
Male
- MI:
-
Mechanical index
- MRI:
-
Magnetic resonance imaging
- SD:
-
Standard deviation
- US:
-
Ultrasonography
References
Spârchez Z, Radu P, Kacso G et al (2015) Prospective comparison between real time contrast enhanced and conventional ultrasound guidance in percutaneous biopsies of liver tumors. Med Ultrason 17(4):456-63. https://doi.org/10.11152/mu.2013.2066.174.deu
Devi CRB (2014) Enlightened oncologists can provide quality cancer care at reduced costs. J Surg Oncol 110(6):643–644. https://doi.org/10.1002/jso.23746
Lee JY, Minami Y, Choi BI et al (2020) The AFSUMB consensus statements and recommendations for the clinical practice of contrast-enhanced ultrasound using Sonazoid. Ultrasonography 39(3):191–220. https://doi.org/10.14366/usg.20057
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69(1):182–236. https://doi.org/10.1016/j.jhep.2018.03.019
Aubé C, Oberti F, Lonjon J et al (2017) EASL and AASLD recommendations for the diagnosis of HCC to the test of daily practice. Liver Int 37(10):1515–1525. https://doi.org/10.1111/liv.13429
Hakime A, Deschamps F, De Carvalho EG et al (2012) Electromagnetic-tracked biopsy under ultrasound guidance: preliminary results. Cardiovasc Intervent Radiol 35(4):898–905. https://doi.org/10.1007/s00270-011-0278-8
Dietrich CF, Nolsøe CP, Barr RG et al (2020) Guidelines and good clinical practice recommendations for contrast-enhanced ultrasound (CEUS) in the Liver-Update 2020 WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol 46(10):2579–2604. https://doi.org/10.1016/j.ultrasmedbio.2020.04.030
Schlottmann K, Klebl F, Zorger N et al (2004) Contrast-enhanced ultrasound allows for interventions of hepatic lesions which are invisible on conventional B-mode. Z Gastroenterol 42(04):303–310. https://doi.org/10.1055/s-2004-812712
Kang TW, Lee MW, Song KD et al (2017) Added value of contrast-enhanced ultrasound on biopsies of focal hepatic lesions invisible on fusion imaging guidance. Korean J Radiol 18(1):152–161. https://doi.org/10.3348/kjr.2017.18.1.152
Chung YE, Kim KW (2015) Contrast-enhanced ultrasonography: advance and current status in abdominal imaging. Ultrasonography 34:3-18. https://doi.org/10.14366/usg.14034
Strobel D, Seitz K, Blank W et al (2008) Contrast-enhanced ultrasound for the characterization of focal liver lesions diagnostic accuracy in clinical practice (DEGUM multicenter trial). Ultraschall Med 29:99–505. https://doi.org/10.1055/s-2008-1027806
Sporea I, Badea R, Popescu A et al (2014) Contrast-enhanced ultrasound (CEUS) for the evaluation of focal liver lesions – a prospective multicenter study of its usefulness in clinical practice. Ultraschall Med 35:259–266. https://doi.org/10.1055/s-0033-1355728
Xie LM, Yang G, Ding HL et al (2011) Diagnostic value of contrast-enhanced ultrasound, computed tomography and magnetic resonance imaging for focal liver lesions: a meta-analysis. Ultrasound Med Biol 37:854–861. https://doi.org/10.1016/j.ultrasmedbio.2011.03.006
Claudon M, Dietrich CF, Choi BI et al (2013) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) in the liver–update 2012. Ultraschall Med 34(01):11–29. https://doi.org/10.1055/s-0032-1325499
Lorentzen T, Nolsoe CP, Ewertsen C et al (2015) EFSUMB guidelines on Interventional Ultrasound (INVUS), Part I. general aspects (long version). Ultraschall Med 36(5):E1–E14. https://doi.org/10.1055/s-0035-1553593
Yoon SH, Lee KH, Kim SY et al (2010) Real-time contrast-enhanced ultrasound-guided biopsy of focal hepatic lesions not localised on B-mode ultrasound. Eur Radiol 20(8):2047–2056. https://doi.org/10.1007/s00330-010-1757-z
Bravo AA, Sheth SG, Chopra S (2001) Liver biopsy. N Engl J Med 344:495–500. https://doi.org/10.1056/NEJM200102153440706
Sparchez Z, Mocan T, Hagiu C et al (2019) Real-time contrast-enhanced-guided biopsy compared with conventional ultrasound-guided biopsy in the diagnosis of hepatic tumors on a background of advanced chronic liver disease: a prospective, randomized, clinical trial. Ultrasound Med Biol 45(11):2915–2924. https://doi.org/10.1016/j.ultrasmedbio.2019.07.678
Colecchia A, Scaioli E, Montrone L et al (2011) Pre-operative liver biopsy in cirrhotic patients with early hepatocellular carcinoma represents a safe and accurate diagnostic tool for tumour grading assessment. J Hepatol:54300–54305. https://doi.org/10.1016/j.jhep.2010.06.037
Cartier V, Crouan A, Esvan M et al (2018) Suspicious liver nodule in chronic liver disease: usefulness of second biopsy. Diagn Interv Imaging 99:493–499. https://doi.org/10.1016/j.diii.2017.12.014
Lipnik AJ, Brown DB (2015) Image-guided percutaneous abdominal mass biopsy: technical and clinical considerations. Radiol Clin North Am 53(5):1049–1059. https://doi.org/10.1016/j.rcl.2015.05.007
Cadranel JF, Rufat P, Degos F (2000) Practices of liver biopsy in France: results of a prospective nationwide survey. For the Group of Epidemiology of the French Association for the Study of the Liver (AFEF). J Hepatol 32(3):477–481. https://doi.org/10.1053/jhep.2000.16602
Porter TR, Abdelmoneim S, Belcik JT et al (2014) Guidelines for the cardiac sonographer in the performance of contrast echocardiography: a focused update from the American Society of Echocardiography. J Am Soc Echocardiog 27(8):797–810. https://doi.org/10.1016/j.echo.2014.05.011
Wei K, Mulvagh SL, Carson L et al (2008) The safety of deFinity and Optison for ultrasound image enhancement: a retrospective analysis of 78,383 administered contrast doses. J Am Soc Echocardiog 21(11):1202–1206. https://doi.org/10.1016/j.echo.2008.07.019
Herzog CA (2008) Incidence of adverse events associated with use of perflutren contrast agents for echocardiography. JAMA 299(17):2023–2025. https://doi.org/10.1001/jama.299.17.2023
Main ML, Ryan AC, Davis TE et al (2008) Acute mortality in hospitalized patients undergoing echocardiography with and without an ultrasound contrast agent (multicenter registry results in 4,300,966 consecutive patients). Am J Cardiol 102(12):1742–1746. https://doi.org/10.1016/j.amjcard.2008.08.019
Wu W, Chen MH, Yin SS et al (2006) The role of contrast-enhanced sonography of focal liver lesions before percutaneous biopsy. AJR Am J Roentgenol 187(3):752–761. https://doi.org/10.2214/AJR.05.0535
Acknowledgements
The authors would like to express their gratitude to EditSprings (https://www.editsprings.com/en?type = com/) for the expert linguistic services provided. We also thank all of the patients involved in the study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xiao-Qing Pei.
Conflict of interest
The authors declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical method was necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board for this retrospective study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, JX., Shi, CG., Xu, YF. et al. The benefit of contrast-enhanced ultrasound in biopsies for focal liver lesions: a retrospective study of 820 cases. Eur Radiol 32, 6830–6839 (2022). https://doi.org/10.1007/s00330-022-08988-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-022-08988-w