Abstract
Objectives
To identify clinical and staging chest CT characteristics predictive of brain metastasis in patients with newly diagnosed NSCLC dichotomized according to resectability.
Methods
Patients newly diagnosed with NSCLC of clinical stages II–IV between November 2017 and October 2018 were enrolled and classified into resectable (stage II+IIIA) and unresectable stages (stage IIIB/C+IV) according to chest CT. Associations of clinicopathological characteristics and CT findings with brain metastasis were analyzed using logistic regression. Predictive models were evaluated using receiver operating characteristics curve analysis. A subgroup analysis for unresectable-stage patients with known epidermal growth factor receptor gene (EGFR) mutation status was performed.
Results
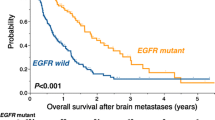
This study included 911 NSCLC patients (mean age, 65 ± 11 years; 620 men), 194 of whom were diagnosed with brain metastasis. For resectable stages, independent predictors for brain metastasis were N2-stage (13 of 25 patients), absence of air-bronchogram/bubble lucency (23 of 25 patients), and presence of spiculation (15 of 25 patients), with a model combining the two imaging features showing an AUC of 0.723. In unresectable stages, independent predictors of brain metastasis were younger age, female sex, extrathoracic metastasis, and adenocarcinoma, with models combining these showing AUCs of 0.675–0.766. In the subgroup with known EGFR-mutation status, extrathoracic metastasis and positive EGFR mutation were independent predictors of brain metastasis, with the model showing AUCs of 0.641–0.732.
Conclusion
CT-derived imaging features, clinical stages, lung cancer subtype, and EGFR mutation were associated with brain metastasis in patients with newly diagnosed NSCLC. The predictors were completely different between resectable and unresectable stages.
Key Points
• In resectable stages of NSCLC, two imaging features (absence of air-bronchogram/bubble lucency and presence of spiculation) and N2 stage were independent predictors of brain metastasis.
• In unresectable stages of NSCLC, younger age, female sex, extrathoracic metastasis, and adenocarcinoma were associated with brain metastasis.
• In the subgroup of NSCLC with known EGFR-mutation status, extrathoracic metastasis and positive EGFR mutation were independent predictors of brain metastasis.






Similar content being viewed by others
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- ALK:
-
Anaplastic lymphoma kinase gene
- CI:
-
Confidence interval
- EGFR:
-
Epidermal growth factor receptor gene
- NSCLC:
-
Non-small cell lung cancer
- OR:
-
Odds ratio
- ROC:
-
Receiver operating characteristics
References
Schouten LJ, Rutten J, Huveneers HA, Twijnstra A (2002) Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer 94:2698–2705
Barnholtz-Sloan JS, Sloan AE, Davis FG, Vigneau FD, Lai P, Sawaya RE (2004) Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. J Clin Oncol 22:2865–2872
Peters S, Bexelius C, Munk V, Leighl N (2016) The impact of brain metastasis on quality of life, resource utilization and survival in patients with non-small-cell lung cancer. Cancer Treat Rev 45:139–162
Kim H, Goo JM, Kim YT, Park CM (2020) Validation of the eighth edition clinical T categorization system for clinical stage IA, resected lung adenocarcinomas: prognostic implications of the ground-glass opacity component. J Thorac Oncol 15:580–588
ES AMB, Greene F et al (eds) (2017) AJCC cancer staging manual, 8th edn. Springer, New York
Shi AA, Digumarthy SR, Temel JS, Halpern EF, Kuester LB, Aquino SL (2006) Does initial staging or tumor histology better identify asymptomatic brain metastases in patients with non-small cell lung cancer? J Thorac Oncol 1:205–210
Ando T, Kage H, Saito M et al (2018) Early stage non-small cell lung cancer patients need brain imaging regardless of symptoms. Int J Clin Oncol 23:641–646
Mujoomdar A, Austin JH, Malhotra R et al (2007) Clinical predictors of metastatic disease to the brain from non-small cell lung carcinoma: primary tumor size, cell type, and lymph node metastases. Radiology 242:882–888
Shin DY, Na II, Kim CH, Park S, Baek H, Yang SH (2014) EGFR mutation and brain metastasis in pulmonary adenocarcinomas. J Thorac Oncol 9:195–199
Mitra D, Chen YH, Li R et al (2019) EGFR mutant locally advanced non-small cell lung cancer is at increased risk of brain metastasis. Clin Transl Radiat Oncol 18:32–38
Wang H, Wang Z, Zhang G et al (2020) Driver genes as predictive indicators of brain metastasis in patients with advanced NSCLC: EGFR, ALK, and RET gene mutations. Cancer Med 9:487–495
Liu Y, Kim J, Qu F et al (2016) CT features associated with epidermal growth factor receptor mutation status in patients with lung adenocarcinoma. Radiology 280:271–280
Rizzo S, Petrella F, Buscarino V et al (2016) CT radiogenomic characterization of EGFR, K-RAS, and ALK mutations in non-small cell lung cancer. Eur Radiol 26:32–42
Kim M, Suh CH, Lee SM et al (2020) Diagnostic yield of staging brain MRI in patients with newly diagnosed non–small cell lung cancer. Radiology 297:419–427
Lynch DA, Austin JHM, Hogg JC et al (2015) CT-definable subtypes of chronic obstructive pulmonary disease: a statement of the Fleischner Society. Radiology 277:192–205
Suh CH, Jung SC, Kim KW, Pyo J (2016) The detectability of brain metastases using contrast-enhanced spin-echo or gradient-echo images: a systematic review and meta-analysis. J Neurooncol 129:363–371
Travis WD, Brambilla E, Nicholson AG et al (2015) The 2015 World Health Organization classification of lung tumors: impact of genetic, clinical and radiologic advances since the 2004 classification. J Thorac Oncol 10:1243–1260
Mok TS, Wu Y-L, Thongprasert S et al (2009) Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 361:947–957
Soda M, Isobe K, Inoue A et al (2012) A prospective PCR-based screening for the EML4-ALK oncogene in non-small cell lung cancer. Clin Cancer Res 18:5682–5689
Wong DW, Leung EL, So KK et al (2009) The EML4-ALK fusion gene is involved in various histologic types of lung cancers from nonsmokers with wild-type EGFR and KRAS. Cancer 115:1723–1733
Riley RD, Snell KI, Ensor J et al (2019) Minimum sample size for developing a multivariable prediction model: PART II - binary and time-to-event outcomes. Stat Med 38:1276–1296
Hosmer DW, Lemeshow S (2000) Assessing the fit of the model. In: Applied Logistic Regression, 2nd edn. Wiley, New York, pp 143–202
Zwirewich CV, Vedal S, Miller RR, Müller NL (1991) Solitary pulmonary nodule: high-resolution CT and radiologic-pathologic correlation. Radiology 179:469–476
McWilliams A, Tammemagi MC, Mayo JR et al (2013) Probability of cancer in pulmonary nodules detected on first screening CT. N Engl J Med 369:910–919
Yoshino I, Ichinose Y, Nagashima A et al (2006) Clinical characterization of node-negative lung adenocarcinoma: results of a prospective investigation. J Thorac Oncol 1:825–831
Hattori A, Suzuki K, Maeyashiki T et al (2013) The presence of air bronchogram is a novel predictor of negative nodal involvement in radiologically pure-solid lung cancer†. Eur J Cardiothorac Surg 45:699–702
Yoshino I, Nakanishi R, Kodate M et al (2000) Pleural retraction and intra-tumoral air-bronchogram as prognostic factors for stage I pulmonary adenocarcinoma following complete resection. Int Surg 85:105–112
Kondo T, Yamada K, Noda K, Nakayama H, Kameda Y (2002) Radiologic-prognostic correlation in patients with small pulmonary adenocarcinomas. Lung Cancer 36:49–57
Bajard A, Westeel V, Dubiez A et al (2004) Multivariate analysis of factors predictive of brain metastases in localised non-small cell lung carcinoma. Lung Cancer 45:317–323
Wang S, Zhou M, Liu Z et al (2017) Central focused convolutional neural networks: developing a data-driven model for lung nodule segmentation. Med Image Anal 40:172–183
Hsu F, De Caluwe A, Anderson D, Nichol A, Toriumi T, Ho C (2016) EGFR mutation status on brain metastases from non-small cell lung cancer. Lung Cancer 96:101–107
Kang HJ, Lim HJ, Park JS et al (2014) Comparison of clinical characteristics between patients with ALK-positive and EGFR-positive lung adenocarcinoma. Respir Med 108:388–394
Fallet V, Cadranel J, Doubre H et al (2014) Prospective screening for ALK: clinical features and outcome according to ALK status. Eur J Cancer 50:1239–1246
Acknowledgements
We are grateful to Jungbok Lee, who is a statistician in our institution, for help with statistical modeling.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Sang Min Lee.
Conflict of Interest
The authors declare no competing interests.
Statistics and Biometry
Jungbok Lee, who is a statistician in Asan Medical Center, helped with statistical modeling.
Informed Consent
Written informed consent was waived by the Institutional Review Board.
Ethical Approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
All of our study patients (911 out of 911) were reported in a previous retrospective study, which evaluated the diagnostic yield of brain MRI in the initial evaluation of non-small cell lung cancer (reference 14, Diagnostic Yield of Staging Brain MRI in Patients with Newly Diagnosed Non–Small Cell Lung Cancer. Radiology 297419-427).
Methodology
• retrospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
ESM 1
(DOCX 253 kb)
Rights and permissions
About this article
Cite this article
Park, S., Lee, S.M., Ahn, Y. et al. Identification of predictors for brain metastasis in newly diagnosed non-small cell lung cancer: a single-center cohort study. Eur Radiol 32, 990–1001 (2022). https://doi.org/10.1007/s00330-021-08215-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08215-y