Abstract
Objectives
To evaluate the baseline MRI characteristics for predicting survival outcomes and construct survival models for risk stratification to facilitate personalized treatment and follow-up strategies in patients with MRI-defined T3 (mrT3) locally advanced rectal cancer (LARC).
Methods
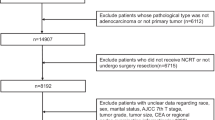
We retrospectively reviewed 256 mrT3 LARC patients evaluated between 2008 and 2012 in our institution, with an average follow-up period of 6.8 ± 1.2 years. The baseline MRI characteristics, clinical data, and follow-up information were evaluated. The patients were randomized into a training cohort (TC, 186 patients) and validation cohort (VC, 70 patients). The TC dataset was used to develop multivariate nomograms for disease-free survival (DFS) and overall survival (OS), while the VC dataset was used for independent validation of the models. Harrell concordance (C) indices and Hosmer-Lemeshow calibration were used to evaluate the performances of the models.
Results
Baseline mrT3 substage, extramural venous invasion (EMVI) grading, mucinous adenocarcinoma, mesorectal fascia involvement, elevated pretreatment carcinoembryonic antigen level, and neoadjuvant chemoradiotherapy (NCRT) were independent predictors of DFS. T3 substage, EMVI grading, and NCRT were also independent predictors of OS. The nomograms constructed permitted the individualized prediction of 3-year and 5-year DFS and 5-year OS with high discrimination (C-index range, 0.833–0.892) and good calibration in the TC and VC.
Conclusions
We have identified baseline MRI characteristics that help independently predict survival outcomes in patients with mrT3 LARC. The survival models based on these characteristics allow for the individualized pretreatment risk stratification in patients with mrT3 LARC.
Key Points
• Baseline MRI characteristics can independently stratify risk and predict survival outcomes in patients with mrT3 LARC.
• The nomograms built using selected baseline MRI characteristics facilitate the individualized pretreatment risk stratification and help with clinical decision-making in patients with mrT3 LARC.
• MR-defined risk factors should, therefore, be carefully reported in the baseline MRI evaluation.





Similar content being viewed by others
Abbreviations
- CEA:
-
Carcinoembryonic antigen
- DFS:
-
Disease-free survival
- EMD:
-
Extramural depth
- EMVI:
-
Extramural venous invasion
- LARC:
-
Locally advanced rectal cancer
- LNM:
-
Lymph node metastasis
- MAC:
-
Mucinous adenocarcinoma
- MRF:
-
Mesorectal fascia
- MRI:
-
Magnetic resonance imaging
- OS:
-
Overall survival
References
Siegel RL, Miller KD, Jemal A (2018) Cancer statistics, 2018. CA Cancer J Clin 68:7–30
Benson AB 3rd, Venook AP, Al-Hawary MM et al (2018) Rectal cancer, Version 2.2018, NCCN Clinical Practice Guidelines in Oncology. J Natl Compr Canc Netw 16:874–901
Kolarich A, George TJ Jr, Hughes SJ et al (2018) Rectal cancer patients younger than 50 years lack a survival benefit from NCCN guideline-directed treatment for stage II and III disease. Cancer 124:3510–3519
Sineshaw HM, Jemal A, Thomas CR Jr, Mitin T (2016) Changes in treatment patterns for patients with locally advanced rectal cancer in the United States over the past decade: an analysis from the National Cancer Data Base. Cancer 122:1996–2003
Zinicola R, Pedrazzi G, Haboubi N, Nicholls RJ (2017) The degree of extramural spread of T3 rectal cancer: an appeal to the American Joint Committee on Cancer. Colorectal Dis 19:8–15
Ma B, Gao P, Wang H et al (2017) What has preoperative radio(chemo)therapy brought to localized rectal cancer patients in terms of perioperative and long-term outcomes over the past decades? A systematic review and meta-analysis based on 41,121 patients. Int J Cancer 141:1052–1065
Cho SH, Kim SH, Bae JH et al (2014) Prognostic stratification by extramural depth of tumor invasion of primary rectal cancer based on the Radiological Society of North America proposal. AJR Am J Roentgenol 202:1238–1244
Chand M, Bhangu A, Wotherspoon A et al (2014) EMVI-positive stage II rectal cancer has similar clinical outcomes as stage III disease following preoperative chemoradiotherapy. Ann Oncol 25:858–863
Son IT, Kim YH, Lee KH et al (2017) Oncologic relevance of magnetic resonance imaging-detected threatened mesorectal fascia for patients with mid or low rectal cancer: a longitudinal analysis before and after long-course, concurrent chemoradiotherapy. Surgery 162:152–163
Nougaret S, Rouanet P, Molinari N et al (2012) MR volumetric measurement of low rectal cancer helps predict tumor response and outcome after combined chemotherapy and radiation therapy. Radiology 263:409–418
Chi YK, Zhang XP, Li J, Sun YS (2011) To be or not to be: significance of lymph nodes on pretreatment CT in predicting survival of rectal cancer patients. Eur J Radiol 77:473–477
Lee ES, Kim MJ, Park SC et al (2018) Magnetic resonance imaging-detected extramural venous invasion in rectal cancer before and after preoperative chemoradiotherapy: diagnostic performance and prognostic significance. Eur Radiol 28:496–505
Patel UB, Brown G, Machado I et al (2017) MRI assessment and outcomes in patients receiving neoadjuvant chemotherapy only for primary rectal cancer: long-term results from the GEMCAD 0801 trial. Ann Oncol 28:344–353
Sun Y, Lin H, Lu X et al (2017) A nomogram to predict distant metastasis after neoadjuvant chemoradiotherapy and radical surgery in patients with locally advanced rectal cancer. J Surg Oncol 115:462–469
Valentini V, van Stiphout RG, Lammering G et al (2011) Nomograms for predicting local recurrence, distant metastases, and overall survival for patients with locally advanced rectal cancer on the basis of European randomized clinical trials. J Clin Oncol 29:3163–3172
Li ZH, Xie PY, Zhang DF et al (2019) Nomogram for predicting disease-free survival among a multicenter cohort of Chinese patients with locally advanced rectal cancer. Cancer Manag Res 11:2471–2483
Ye F, Zhang H, Liang X, Ouyang H, Zhao X, Zhou C (2016) JOURNAL CLUB: preoperative MRI evaluation of primary rectal cancer: intrasubject comparison with and without rectal distention. AJR Am J Roentgenol 207:32–39
Nougaret S, Reinhold C, Mikhael HW, Rouanet P, Bibeau F, Brown G (2013) The use of MR imaging in treatment planning for patients with rectal carcinoma: have you checked the “DISTANCE”? Radiology 268:330–344
Smith NJ, Barbachano Y, Norman AR, Swift RI, Abulafi AM, Brown G (2008) Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg 95:229–236
Taylor FG, Quirke P, Heald RJ et al (2014) Preoperative magnetic resonance imaging assessment of circumferential resection margin predicts disease-free survival and local recurrence: 5-year follow-up results of the MERCURY study. J Clin Oncol 32:34–43
Park SH, Lim JS, Lee J, et al (2017) Rectal mucinous adenocarcinoma: MR imaging assessment of response to concurrent chemotherapy and radiation therapy-a hypothesis-generating study. Radiology 162657
Akiyoshi T, Matsueda K, Hiratsuka M et al (2015) Indications for lateral pelvic lymph node dissection based on magnetic resonance imaging before and after preoperative chemoradiotherapy in patients with advanced low-rectal cancer. Ann Surg Oncol 22(Suppl 3):S614–S620
Brown G, Richards CJ, Bourne MW et al (2003) Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology 227:371–377
Amin MB, Greene FL, Edge SB et al (2017) AJCC Cancer Staging Manual, 8th edn. Springer, Chicago
Meng WJ, Sun XF, Tian C et al (2007) Microsatellite instability did not predict individual survival in sporadic stage II and III rectal cancer patients. Oncology 72:82–88
Russell MC, You YN, Hu CY et al (2013) A novel risk-adjusted nomogram for rectal cancer surgery outcomes. JAMA Surg 148:769–777
van Gijn W, van Stiphout RG, van de Velde CJ et al (2015) Nomograms to predict survival and the risk for developing local or distant recurrence in patients with rectal cancer treated with optional short-term radiotherapy. Ann Oncol 26:928–935
Yu J, Huang DY, Xu HX, Li Y, Xu Q (2016) Correlation between magnetic resonance imaging-based evaluation of extramural vascular invasion and prognostic parameters of T3 stage rectal cancer. J Comput Assist Tomogr 40:537–542
Zhang XY, Wang S, Li XT et al (2018) MRI of extramural venous invasion in locally advanced rectal cancer: relationship to tumor recurrence and overall survival. Radiology 289:677–685
Taylor FG, Quirke P, Heald RJ et al (2011) Preoperative high-resolution magnetic resonance imaging can identify good prognosis stage I, II, and III rectal cancer best managed by surgery alone: a prospective, multicenter, European study. Ann Surg 253:711–719
Yu SK, Chand M, Tait DM, Brown G (2014) Magnetic resonance imaging defined mucinous rectal carcinoma is an independent imaging biomarker for poor prognosis and poor response to preoperative chemoradiotherapy. Eur J Cancer 50:920–927
Prampolini F, Taschini S, Pecchi A, et al (2020) Magnetic resonance imaging performed before and after preoperative chemoradiotherapy in rectal cancer: predictive factors of recurrence and prognostic significance of MR-detected extramural venous invasion. Abdom Radiol (NY) 45:2941–2949
McCawley N, Clancy C, O'Neill BD, Deasy J, McNamara DA, Burke JP (2016) Mucinous rectal adenocarcinoma is associated with a poor response to neoadjuvant chemoradiotherapy: a systematic review and meta-analysis. Dis Colon Rectum 59:1200–1208
Tarantino I, Warschkow R, Worni M et al (2012) Elevated preoperative CEA is associated with worse survival in stage I-III rectal cancer patients. Br J Cancer 107:266–274
Beets-Tan RGH, Lambregts DMJ, Maas M et al (2018) Magnetic resonance imaging for clinical management of rectal cancer: updated recommendations from the 2016 European Society of Gastrointestinal and Abdominal Radiology (ESGAR) consensus meeting. Eur Radiol 28:1465–1475
Kim S, Han K, Seo N et al (2018) T2-weighted signal intensity-selected volumetry for prediction of pathological complete response after preoperative chemoradiotherapy in locally advanced rectal cancer. Eur Radiol 28:5231–5240
Zhang H, Zhang C, Zheng Z et al (2017) Chemical shift effect predicting lymph node status in rectal cancer using high-resolution MR imaging with node-for-node matched histopathological validation. Eur Radiol 27:3845–3855
Shin R, Jeong SY, Yoo HY et al (2012) Depth of mesorectal extension has prognostic significance in patients with T3 rectal cancer. Dis Colon Rectum 55:1220–1228
Acknowledgements
We appreciate Shangying Hu for her statistical advice for this manuscript.
Funding
This study has received funding from the National Nature Science Foundation of China (Grant 81971589); the Peking Union Medical College Youth Fund, the Fundamental Research Funds for the Central Universities (No. 3332018078); and the Beijing Hope Run Special Fund of the Cancer Foundation of China (No. LC2017B18).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Hongmei Zhang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Shangying Hu kindly provided statistical advice for this manuscript.
Informed consent
Only if the study is on human subjects: Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• retrospective
• diagnostic or prognostic study/observational
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 17 kb)
Rights and permissions
About this article
Cite this article
Zhao, Q., Wan, L., Zou, S. et al. Prognostic risk factors and survival models for T3 locally advanced rectal cancer: what can we learn from the baseline MRI?. Eur Radiol 31, 4739–4750 (2021). https://doi.org/10.1007/s00330-021-08045-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08045-y