Abstract
Objectives
Vertebral invasion is a key prognostic factor and a critical aspect of surgical planning for superior sulcus tumors. This study aims to further evaluate MRI features of vertebral invasion in order to distinguish it from reactive inflammatory changes.
Methods
Between 2000 and 2016, a retrospective study was performed at a single institution. All patients with superior sulcus tumors undergoing surgery, including at least two partial vertebrectomies, were included. An expert radiologist evaluated qualitative and quantitative MRI signal intensity characteristics (contrast-to-noise ratio [CNR]) of suspected involved and non-involved vertebrae. A comparison of CNR of invaded and sane vertebrae was performed using non-parametric tests. Imaging data were correlated with pathological findings.
Results
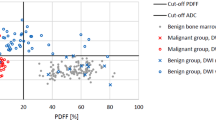
A total of 92 surgical samples of vertebrectomy were analyzed. The most specific sequences for invasion were T1 and T2 weighted (92% and 97%, respectively). The most sensitive sequences were contrast enhanced T1 weighted fat suppressed and T2 weighted fat suppressed (100% and 80%). Loss of extrapleural paravertebral fat on the T1-weighted sequence was highly sensitive (100%) but not specific (63%). Using quantitative analysis, the optimum cut-off (p < 0.05) to distinguish invasion from reactive inflammatory changes was CNR > 11 for the T2-weighted fat-sat sequence (sensitivity 100%), CNR > 9 for contrast-enhanced T1-weighted fat-suppressed sequence (sensitivity 100%), and CNR < − 30 for the T1-weighted sequence (specificity 97%). Combining these criteria, 23 partial vertebrectomies could have been avoided in our cohort.
Conclusion
Qualitative and quantitative MRI analyses are useful to discriminate vertebral invasion from reactive inflammatory changes.
Key Points
• Abnormal signal intensity in a vertebral body adjacent to a superior sulcus tumor may be secondary to direct invasion or reactive inflammatory changes.
• Accurate differentiation between invasion and reactive inflammatory changes significantly impacts surgical planning. T1w and T2w are the best sequences to differentiate malignant versus benign bone marrow changes. The use of quantitative analysis improves MRI specificity.
• Using contrast media improves the sensitivity for the detection of tumor invasion.






Similar content being viewed by others
Abbreviations
- ACCP:
-
American College of Chest Physicians
- CNR:
-
Contrast-to-noise ratio
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- NCNN:
-
National Comprehensive Cancer Network
- NICE:
-
National Institute for Clinical Excellence
- NPV:
-
Negative predictive value
- PACS:
-
Picture Archived Centralized System
- PPV:
-
Positive predictive value
- ROC curve:
-
Receiver operating characteristic curve
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- STIR:
-
Short tau inversion recovery
- T1w:
-
T1-weighted images
- T2w:
-
T1-weighted images
References
Shen KR, Meyers BF, Larner JM et al (2007) Special treatment issues in lung cancer: ACCP evidence-based clinical practice guidelines (2nd edition). Chest 132:290S–305S
Koizumi K, Haraguchi S, Hirata T et al (2004) Surgical treatment of lung cancer with vertebral invasion. Ann Thorac Cardiovasc Surg 10(4):229–234
Foroulis CN, Zarogoulidis P, Darwiche K et al (2013) Superior sulcus (pancoast) tumors: current evidence on diagnosis and radical treatment. J Thorac Dis 5(Suppl 4):S342–S358
Fadel E, Missenard G, Court C et al (2011) Long-term outcomes of en bloc resection of non-small cell lung cancer invading the thoracic inlet and spine. Ann Thorac Surg 92(3):1024–1030 discussion 1030
Chadeyras J-B, Mazel C, Grunenwald D (2006) Vertebral en bloc resection for lung cancer: twelve years’ experience. Ann Chir 131(10):616–622
Deslauriers J, Tronc F, Fortin D (2013) Management of tumors involving the chest wall including pancoast tumors and tumors invading the spine. Thorac Surg Clin 23(3):313–325
Kozower BD, Larner JM, Detterbeck FC, Jones DR (2013) Special treatment issues in non-small cell lung cancer. Chest 143(5):e369S–e399S
Heelan RT, Demas BE, Caravelli JF et al (1989) Superior sulcus tumors: CT and MR imaging. Radiology 170(3 Pt 1):637–641
Ratto GB, Piacenza G, Frola C et al (1991) Chest wall involvement by lung cancer: computed tomographic detection and results of operation. Ann Thorac Surg 51(2):182–188
Haggar AM, Pearlberg JL, Froelich JW et al (1987) Chest-wall invasion by carcinoma of the lung: detection by MR imaging. AJR Am J Roentgenol 148(6):1075–1078
Imaizumi A, Yoshino N, Yamada I et al (2006) A potential pitfall of MR imaging for assessing mandibular invasion of squamous cell carcinoma in the oral cavity. AJNR Am J Neuroradiol 27(1):114–122
Thomas-de-Montpréville V, Chapelier A, Fadel E, Mussot S, Dulmet E, Dartevelle P (2004) Chest wall resection for invasive lung carcinoma, soft tissue sarcoma, and other types of malignancy. Pathologic aspects in a series of 107 patients. Ann Diagn Pathol 8(4):198–206
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics. 44(3):837–845
Haberkorn U, Schoenberg SO (2001) Imaging of lung cancer with CT, MRT and PET. Lung Cancer 34(Suppl 3):S13–S23
Carter BW, Gladish GW (2015) MR imaging of chest wall tumors. Magn Reson Imaging Clin N Am 23(2):197–215
Bonomo L, Ciccotosto C, Guidotti A, Storto ML (1996) Lung cancer staging: the role of computed tomography and magnetic resonance imaging. Eur J Radiol 23(1):35–45
Bruzzi JF, Komaki R, Walsh GL et al (2008) Imaging of non–small cell lung cancer of the superior sulcus: part 2: initial staging and assessment of resectability and therapeutic response1. Radiographics 28(2):561–572
Padovani B, Mouroux J, Seksik L et al (1993) Chest wall invasion by bronchogenic carcinoma: evaluation with MR imaging. Radiology 187(1):33–38
Freundlich IM, Chasen MH, Varma DG (1996) Magnetic resonance imaging of pulmonary apical tumors. J Thorac Imaging 11(3):210–222
Rusch VW, Giroux DJ, Kraut MJ et al (2007) Induction chemoradiation and surgical resection for superior sulcus non-small-cell lung carcinomas: long-term results of Southwest Oncology Group Trial 9416 (Intergroup Trial 0160). J Clin Oncol 25(3):313–318
Acknowledgements
We thank Dr. Celine Denoiseux for editing the manuscript.
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Caramella Caroline.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• Retrospective
• Observational
• Performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 15 kb)
Rights and permissions
About this article
Cite this article
Mihoubi Bouvier, F., Thomas De Montpréville, V., Besse, B. et al. Can MRI differentiate surrounding vertebral invasion from reactive inflammatory changes in superior sulcus tumor?. Eur Radiol 31, 8991–8999 (2021). https://doi.org/10.1007/s00330-021-08001-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-021-08001-w