Abstract
Aim
We investigated if loop characteristics correlate with audio-vestibular symptoms or hemifacial spasm in patients with a vascular loop in the root entry zone (VII and VIII) and in the internal auditory canal.
Materials and methods
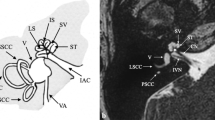
A retrospective, multicenter study analyzed 2622 consecutive magnetic resonance imaging (MRI) scans of the cerebellopontine angle of patients with asymmetric audio-vestibular symptom or hemifacial spasm; patients’ symptoms were confirmed by clinical tests. MRIs displaying vascular loops visible in the axial view were analyzed using multiplanar reconstruction. We evaluated (1) depth of penetration of the loop into the internal auditory canal (IAC); (2) largest diameter of the vessel; (3) nerve(s) involved in the vascular impingement, position of the loop relative to such nerve(s) and number of contacts between vessel and nerve(s); (4) length of such contact. The loop metrics described above were correlated with the patients’ audio-vestibular symptoms and hemifacial spasm.
Results
Three hundred ninety-nine patients displayed a loop visible in the MRI axial view and out of them only 118 displayed a direct contact between loop and nerve. The cochlear nerve was involved in a contact in 57.7%. Loops in direct nerve contact had a calibre > 0.85 mm, were located in the middle portion of the IAC, and correlated with vertigo (p = 0.002), tinnitus (p = 0.003), and hemifacial spasm (p < 0.001). Asymmetric sensorineural hearing loss (SNHL) correlated with number of contacts (p < 0.001) and length of contact (p < 0.05). The contact was asymptomatic in 41.5% of patients.
Conclusion
Loop characteristics may help predict whether a vascular impingement is responsible for a symptom and guide the physician to select the best treatment.
Key Points
• A vascular loop in the internal auditory canal was observed in 18–20% of the patients in this study; whether a loop can be responsible for a compressive syndrome is still unclear in particular referred to the vestibulocochlear nerve.
• Compression by a loop on the facial nerve causes hemifacial spasm; compression by a loop on the cochlear or vestibular nerve may cause audio-vestibular symptoms.
• In patients with a loop, the loop calibre, the loop position, and the number of loop-nerve(s) assessed via the multiplanar MRI reconstruction technique may help assess whether the patient will manifest audio-vestibular symptoms or hemifacial spasm.







Similar content being viewed by others
Abbreviations
- CI:
-
Confidence interval
- CISS:
-
Constructive interference steady state
- CPA:
-
Cerebellum-pontine angle
- FOV:
-
Field of view
- FT:
-
Fourier transformation
- IAC:
-
Internal auditory canal
- IRB:
-
Institutional Review Board
- MRI:
-
Magnetic resonance imaging
- NEX:
-
Number of excitations
- PTA:
-
Pure tone average
- REZ:
-
Root entry zone
- SD:
-
Standard deviation
- SNHL:
-
Sensorineural hearing loss
- TE:
-
Echo time
- TR:
-
Repetition time
- v-HIT:
-
Video head impulse test
References
Reisser C, Schuknecht HF (1991) The anterior inferior cerebellar artery in the internal auditory canal. Laryngoscope 101:761–766
Mazzoni A, Hansen CC (1970) Surgical anatomy of the arteries of the internal auditory canal. Arch Otolaryngol 91:128–135
Ryu H, Tanaka T, Yamamoto S, Uemura K, Takehara Y, Isoda H (1999) Magnetic resonance cisternography used to determine precise topography of the facial nerve and three components of the eighth cranial nerve in the internal auditory canal and cerebellopontine cistern. J Neurosurg 90:624–634
Hoekstra CE, Prijs VF, van Zanten GA (2015) Diagnostic yield of a routine magnetic resonance imaging in tinnitus and clinical relevance of the anterior inferior cerebellar artery loops. Otol Neurotol 36:359–365
Jannetta PJ (1967) Arterial compression of the trigeminal nerve at the pons in patients with trigeminal neuralgia. J Neurosurg 26:159–162
Okamura T, Kurokawa Y, Ikeda N et al (2000) Microvascular decompression for cochlear symptoms. J Neurosurg 93:421–426
Levine R, Oron Y (2015) Tinnitus. In: Celesia G, Hickok G (Eds) Handbook of clinical neurology. Elsevier, Amsterdam
Jannetta PJ (1975) Neurovascular cross-compression in patients with hyperactive dysfunction symptoms of the eighth cranial nerve. Surg Forum 26:467–469
Brackmann DE, Kesser BW, Day JD (2001) Microvascular decompression of the vestibulocochlear nerve for disabling positional vertigo: the House Ear Clinic experience. Otol Neurotol 22:882–887
Borghei-Razavi H, Darvish O, Schick U (2014) Disabling vertigo and tinnitus caused by intrameatal compression of the anterior inferiorcerebellar artery on the vestibulocochlear nerve: a case report, surgical considerations, and review of the literature. J Neurol Surg Rep 75:e 47–e 51
Bae YJ, Jeon YJ, Choi BS, Koo JW, Song JJ (2017) The role of MRI in diagnosing neurovascular compression of the cochlear nerve resulting in typewriter tinnitus. AJNR Am J Neuroradiol 38(6):1212–1217
Beyazal Celiker F, Dursun E, Celiker M et al (2017) Evaluation of vascular variations at cerebellopontine angle by 3D T2WI magnetic-resonance imaging in patients with vertigo. J Vestib Res 27:147–153
Gultekin S, Celik H, Akpek S, Oner Y, Gumus T, Tokgoz N (2008) Vascular loops at the cerebellopontine angle: is there a correlation with tinnitus? AJNR Am J Neuroradiol 29:1746–1749
Casselman JW, Kuhweide R, Deimling M, Ampe W, Dehaene I, Meeus L (1993) Constructive interference in steady state-3DFT MR imaging of the inner ear and cerebellopontine angle. AJNR Am J Neuroradiol 14:47–57
McDermott AL, Dutt SN, Irving RM, Pahor AL, Chavda SV (2003) Anterior inferior cerebellar artery syndrome: fact or fiction. Clin Otolaryngol Allied Sci 28:75–80
Nowe V, De Ridder D, Van de Heyning PH et al (2004) Does the location of a vascular loop in the cerebellopontine angle explain pulsatile and non-pulsatile tinnitus? Eur Radiol 14:2282–2289
Chung SS, Chang JW, Kim SH, Chang JH, Park YG, Kim DI (2000) Microvascular decompression of the facial nerve for the treatment of hemifacial spasm: preoperative magnetic resonance imaging related to clinical outcomes. Acta Neurochir (Wien) 142:901–907
Suthipongchai S, Chawalparit O, Churojana A, Poungvarin N (2004) Vascular loop compressing facial nerve in hemifacial spasm: demonstrated by 3D-phase contrast magnetic resonance angiography in 101 patients. J Med Assoc Thai 87:219–224
Wen MH, Cheng PW, Young YH (2017) Dysequilibrium in a 5-year-old child with intrameatal vascular loops bilaterally. Int J Pediatr Otorhinolaryngol 94:8–10
Loader B, Linauer I, Korkesch S et al (2016) A connection between neurovascular conflicts within the cerebellopontine angle and vestibular neuritis, a case controlled cohort study. Acta Otorhinolaryngol Ital 36:421–427
de Abreu Junior L, Kuniyoshi CH, Wolosker AB et al (2016) Vascular loops in the anterior inferior cerebellar artery, as identified by magnetic resonance imaging, and their relationship with otologic symptoms. Radiol Bras 49:300–304
Ezerarslan H, Sanhal EO, Kurukahvecioğlu S, Ataç GK, Kocatürk S (2017) Presence of vascular loops entering internal acoustic channel may increase risk of sudden sensorineural hearing loss and reduce recovery of these patients. Laryngoscope. 127:210–215
Clark JG (1981) Uses and abuses of hearing loss classification. ASHA 23:493–500
Erkoç MF, Imamoglu H, Okur A, Gümüş C, Dogan M (2012) Normative size evaluation of internal auditory canal with magnetic resonance imaging: review of 3786 patients. Folia Morphol (Warsz) 71:217–220
Raminsky M (1984) Ectopic impulse generation in pathologic nerve fibers. In: Dyck P (Eds) Peripheral neuropathy. WB Saunders, Philadelphia
Friede RL (1984) Cochlear axon calibres are adjusted to characteristic frequencies. J Neurol Sci 66:193–200
Thompson TL, Amedee R (2009) Vertigo:a review of common peripheral and central vestibular disorders. Ochsner J 9:20–26
Girard N, Poncet M, Caces F et al (1997) Three-dimensional MRI of hemifacial spasm with surgical correlation. Neuroradiology. 39:46–51
Ricci G, Di Stadio A, D’Ascanio L et al (2018) Endoscope-assisted retrosigmoid approach in hemifacial spasm: our experience. Braz J Otorhinolaryngol
Di Stadio A, Colangeli R, Dipietro L et al (2018) Microsurgical decompression of the cochlear nerve to treat disabling tinnitus via an endoscope-assisted retrosigmoid approach: the Padua experience. World Neurosurg 113:232–237
Abele TA, Besachio DA, Quigley EP et al (2014) Diagnostic accuracy of screening MR imaging using unenhanced axial CISS and coronal T2WI for detection of small internal auditory canal lesions. AJNR Am J Neuroradiol 35:2366–2370
Gorrie A, Warren FM 3rd, de la Garza AN, Shelton C, Wiggins RH 3rd (2010) Is there a correlation between vascular loops in the cerebellopontine angle and unexplained unilateral hearing loss? Otol Neurotol 31:48–52
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Dr. Arianna Di Stadio.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Statistics and biometry
Two of the authors have significant statistical expertise.
Informed consent
Written informed consent was not required for this study because this is a retrospective study and all patients previously signed a written consent before performing their tests and exams.
Ethical approval
Institutional Review Board approval was obtained without the release of a number because this is a retrospective study.
Methodology
• Retrospective
• Diagnostic or prognostic study
• Multicenter study
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Di Stadio, A., Dipietro, L., Ralli, M. et al. Loop characteristics and audio-vestibular symptoms or hemifacial spasm: is there a correlation? A multiplanar MRI study. Eur Radiol 30, 99–109 (2020). https://doi.org/10.1007/s00330-019-06309-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06309-2