Abstract
Objectives
To evaluate the diagnostic performance of proton density fat fraction (PDFF) magnetic resonance imaging (MRI) to differentiate between acute benign and neoplastic vertebral compression fractures (VCFs).
Methods
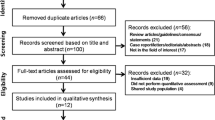
Fifty-seven consecutive patients with 46 acute benign and 41 malignant VCFs were prospectively enrolled in this institutional review board approved study and underwent routine clinical MRI with an additional six-echo modified Dixon sequence of the spine at a clinical 3.0-T scanner. All fractures were categorised as benign or malignant according to either direct bone biopsy or 6-month follow-up MRI. Intravertebral PDFF and PDFFratio (fracture PDFF/normal vertebrae PDFF) for benign and malignant VCFs were calculated using region-of-interest analysis and compared between both groups. Additional receiver operating characteristic and binary logistic regression analyses were performed.
Results
Both PDFF and PDFFratio of malignant VCFs were significantly lower compared to acute benign VCFs [PDFF, 3.48 ± 3.30% vs 23.99 ± 11.86% (p < 0.001); PDFFratio, 0.09 ± 0.09 vs 0.49 ± 0.24 (p < 0.001)]. The areas under the curve were 0.98 for PDFF and 0.97 for PDFFratio, yielding an accuracy of 96% and 95% for differentiating between acute benign and malignant VCFs. PDFF remained as the only imaging-based variable to independently differentiate between acute benign and malignant VCFs on multivariate analysis (odds ratio, 0.454; p = 0.005).
Conclusions
Quantitative assessment of PDFF derived from modified Dixon water-fat MRI has high diagnostic accuracy for the differentiation of acute benign and malignant vertebral compression fractures.
Key Points
• Chemical-shift-encoding based water-fat MRI can reliably assess vertebral bone marrow PDFF
• PDFF is significantly higher in acute benign than in malignant VCFs
• PDFF provides high accuracy for differentiating acute benign from malignant VCFs




Similar content being viewed by others
Abbreviations
- 6E-mDixon:
-
Six-echo modified Dixon
- 95%CI:
-
95 % confidence interval
- mDixon:
-
Modified Dixon
- NPV:
-
Negative predictive value
- PDFF:
-
Proton density fat fraction
- PET/CT:
-
Positron emission tomography/computed tomography
- PPV:
-
Positive predictive value
- ROC:
-
Receiver operating characteristic
- ROI:
-
Region of interest
- SE:
-
Spin echo
- SENSE:
-
Sensitivity encoding
- SPAIR:
-
Spectral attenuated inversion recovery
- TE:
-
Echo time
- TR:
-
Repetition time
- VCF:
-
Vertebral compression fracture
References
Chapman J, Smith JS, Kopjar B et al (2013) The AOSpine North America Geriatric Odontoid Fracture Mortality Study: a retrospective review of mortality outcomes for operative versus nonoperative treatment of 322 patients with long-term follow-up. Spine (Phila Pa 1976) 38:1098–1104
Hansen EJ, Simony A, Carreon L, Andersen MO (2016) Rate of unsuspected malignancy in patients with vertebral compression fracture undergoing percutaneous vertebroplasty. Spine (Phila Pa 1976) 41:549–552
Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH (2003) Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics 23:179–187
Link TM, Guglielmi G, van Kuijk C, Adams JE (2005) Radiologic assessment of osteoporotic vertebral fractures: diagnostic and prognostic implications. Eur Radiol 15:1521–1532
Geith T, Schmidt G, Biffar A et al (2012) Comparison of qualitative and quantitative evaluation of diffusion-weighted MRI and chemical-shift imaging in the differentiation of benign and malignant vertebral body fractures. AJR Am J Roentgenol 199:1083–1092
Disler DG, McCauley TR, Ratner LM, Kesack CD, Cooper JA (1997) In-phase and out-of-phase MR imaging of bone marrow: prediction of neoplasia based on the detection of coexistent fat and water. AJR Am J Roentgenol 169:1439–1447
Zajick DC Jr, Morrison WB, Schweitzer ME, Parellada JA, Carrino JA (2005) Benign and malignant processes: normal values and differentiation with chemical shift MR imaging in vertebral marrow. Radiology 237:590–596
Erly WK, Oh ES, Outwater EK (2006) The utility of in-phase/opposed-phase imaging in differentiating malignancy from acute benign compression fractures of the spine. AJNR Am J Neuroradiol 27:1183–1188
Eito K, Waka S, Naoko N, Makoto A, Atsuko H (2004) Vertebral neoplastic compression fractures: assessment by dual-phase chemical shift imaging. J Magn Reson Imaging 20:1020–1024
Douis H, Davies AM, Jeys L, Sian P (2016) Chemical shift MRI can aid in the diagnosis of indeterminate skeletal lesions of the spine. Eur Radiol 26:932–940
Fischer MA, Nanz D, Shimakawa A et al (2013) Quantification of muscle fat in patients with low back pain: comparison of multi-echo MR imaging with single-voxel MR spectroscopy. Radiology 266:555–563
Ruschke S, Pokorney A, Baum T et al (2017) Measurement of vertebral bone marrow proton density fat fraction in children using quantitative water-fat MRI. MAGMA 30:449–460
Gee CS, Nguyen JT, Marquez CJ et al (2015) Validation of bone marrow fat quantification in the presence of trabecular bone using MRI. J Magn Reson Imaging 42:539–544
Karampinos DC, Melkus G, Baum T, Bauer JS, Rummeny EJ, Krug R (2014) Bone marrow fat quantification in the presence of trabecular bone: initial comparison between water-fat imaging and single-voxel MRS. Magn Reson Med 71:1158–1165
Latifoltojar A, Hall-Craggs M, Bainbridge A et al (2017) Whole-body MRI quantitative biomarkers are associated significantly with treatment response in patients with newly diagnosed symptomatic multiple myeloma following bortezomib induction. Eur Radiol 27:5325–5336
Baker LL, Goodman SB, Perkash I, Lane B, Enzmann DR (1990) Benign versus pathologic compression fractures of vertebral bodies: assessment with conventional spin-echo, chemical-shift, and STIR MR imaging. Radiology 174:495–502
Minne HW, Leidig G, Wuster C et al (1988) A newly developed spine deformity index (SDI) to quantitate vertebral crush fractures in patients with osteoporosis. Bone Miner 3:335–349
Mauch JT, Carr CM, Cloft H, Diehn FE (2018) Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. AJNR Am J Neuroradiol. https://doi.org/10.3174/ajnr.A5528
Faul F, Erdfelder E, Buchner A, Lang AG (2009) Statistical power analyses using G*Power 3.1: tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Yoo HJ, Hong SH, Kim DH et al (2017) Measurement of fat content in vertebral marrow using a modified dixon sequence to differentiate benign from malignant processes. J Magn Reson Imaging 45:1534–1544
Schmeel FC, Luetkens JA, Wagenhauser PJ et al (2018) Proton density fat fraction (PDFF) MRI for differentiation of benign and malignant vertebral lesions. Eur Radiol. https://doi.org/10.1007/s00330-017-5241-x
Kim DH, Yoo HJ, Hong SH, Choi JY, Chae HD, Chung BM (2017) Differentiation of acute osteoporotic and malignant vertebral fractures by quantification of fat fraction with a Dixon MRI sequence. AJR Am J Roentgenol 209:1331–1339
Kugel H, Jung C, Schulte O, Heindel W (2001) Age- and sex-specific differences in the 1H-spectrum of vertebral bone marrow. J Magn Reson Imaging 13:263–268
Ragab Y, Emad Y, Gheita T et al (2009) Differentiation of osteoporotic and neoplastic vertebral fractures by chemical shift {in-phase and out-of phase} MR imaging. Eur J Radiol 72:125–133
Baum T, Yap SP, Dieckmeyer M et al (2015) Assessment of whole spine vertebral bone marrow fat using chemical shift-encoding based water-fat MRI. J Magn Reson Imaging 42:1018–1023
Karampinos DC, Ruschke S, Dieckmeyer M et al (2015) Modeling of T2* decay in vertebral bone marrow fat quantification. NMR Biomed 28:1535–1542
Reeder SB, Robson PM, Yu H et al (2009) Quantification of hepatic steatosis with MRI: the effects of accurate fat spectral modeling. J Magn Reson Imaging 29:1332–1339
Karampinos DC, Yu H, Shimakawa A, Link TM, Majumdar S (2011) T(1)-corrected fat quantification using chemical shift-based water/fat separation: application to skeletal muscle. Magn Reson Med 66:1312–1326
Hines CD, Yu H, Shimakawa A, McKenzie CA, Brittain JH, Reeder SB (2009) T1 independent, T2* corrected MRI with accurate spectral modeling for quantification of fat: validation in a fat-water-SPIO phantom. J Magn Reson Imaging 30:1215–1222
Bray TJP, Bainbridge A, Punwani S, Ioannou Y, Hall-Craggs MA (2017) Simultaneous quantification of bone edema/adiposity and structure in inflamed bone using chemical shift-encoded mri in spondyloarthritis. Magn Reson Med 79:1031–1042
Kukuk GM, Hittatiya K, Sprinkart AM et al (2015) Comparison between modified Dixon MRI techniques, MR spectroscopic relaxometry, and different histologic quantification methods in the assessment of hepatic steatosis. Eur Radiol 25:2869–2879
Yokoo T, Serai SD, Pirasteh A et al (2017) Linearity, bias, and precision of hepatic proton density fat fraction measurements by using MR imaging: a meta-analysis. Radiology 286:486–498
Zampa V, Cosottini M, Michelassi C, Ortori S, Bruschini L, Bartolozzi C (2002) Value of opposed-phase gradient-echo technique in distinguishing between benign and malignant vertebral lesions. Eur Radiol 12:1811–1818
Stabler A, Baur A, Bartl R, Munker R, Lamerz R, Reiser MF (1996) Contrast enhancement and quantitative signal analysis in MR imaging of multiple myeloma: assessment of focal and diffuse growth patterns in marrow correlated with biopsies and survival rates. AJR Am J Roentgenol 167:1029–1036
Funding
The authors state that this work has not received any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Priv.-Doz. Dr. med. Guido Matthias Kukuk at Bonn University Hospital.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all patients in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Schmeel, F.C., Luetkens, J.A., Enkirch, S.J. et al. Proton density fat fraction (PDFF) MR imaging for differentiation of acute benign and neoplastic compression fractures of the spine. Eur Radiol 28, 5001–5009 (2018). https://doi.org/10.1007/s00330-018-5513-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5513-0