Abstract
Objectives
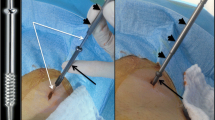
In long bones, cementoplasty alone does not provide sufficient stability, which may cause secondary fractures. This study reviewed the safety and efficacy of reinforced cementoplasty (RC) (percutaneous internal fixation using dedicated spindles combined with cementoplasty) for unstable malignant lesions of the cervicotrochanteric region (CTR) of the proximal femur.
Methods
Eighteen consecutive patients (nine women [50%] and nine men [50%]; mean age 55.1 ± 16.2 years; range 22–85) underwent RC for 19 unstable lesions of the CTR (16/19 [84.2%] bone metastases, 3/19 [15.8%] multiple myeloma lesions). All the patients were considered unsuitable for surgery. Clinical outcome was judged with a mean follow-up of 8.8 ± 7.2 months (range 1–27). The primary endpoints were occurrence of secondary fractures during the follow-up period and local pain relief measured by a visual analogue scale (VAS).
Results
No secondary fracture occurred. Mean VAS improved from 5.9 ± 3.1 (range 0–10) to 2.3 ± 2.4 (range 0–7) at 1 month (p = 0.001) to 1.6 ± 1.7 (range 0-5) at final follow-up (p = 0.0002). One symptomatic cement pulmonary embolism was recorded.
Conclusion
RC is an original minimally invasive technique providing pain relief and effective bone stability for unstable malignant lesions of the cervicotrochanteric region in patients unsuitable for open surgery.
Key Points
• Reinforced cementoplasty (RC) combines intralesional spindling with cementoplasty.
• RC provides effective bone stability and pain relief.
• RC is a suitable minimally invasive option for patients in poor general condition.





Similar content being viewed by others
Abbreviations
- AP:
-
Anteroposterior
- CT:
-
Computed tomography
- CTR:
-
Cervicotrochanteric region
- ECOG:
-
Eastern Cooperative Oncology Group
- IQR:
-
Interquartile range
- MBD:
-
Metastatic bone disease
- MM:
-
Multiple myeloma
- MRI:
-
Magnetic resonance imaging
- PC:
-
Percutaneous cementoplasty
- PMMA:
-
Poly-methyl-methacrylate
- RC:
-
Reinforced cementoplasty
- VAS:
-
Visual analogue scale
- WHO:
-
World Health Organization
References
Harrington KD (1995) Orthopaedic management of extremity and pelvic lesions. Clin Orthop 136–147
Schneiderbauer MM, Sierra RJ, Schleck C et al (2005) Dislocation rate after hip hemiarthroplasty in patients with tumor-related conditions. J Bone Joint Surg Am 87:1810–1815
Nathan SS, Healey JH, Mellano D et al (2005) Survival in patients operated on for pathologic fracture: implications for end-of-life orthopedic care. J Clin Oncol Off J Am Soc Clin Oncol 23:6072–6082
Popken F, Schmidt J, Oegur H et al (2002) Treatment outcome after surgical management of osseous breast carcinoma metastases. Preventive stabilization vs. management after pathological fracture. Unfallchirurg 105:338–343
Mirels H (1989) Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop 256–264
Swanson KC, Pritchard DJ, Sim FH (2000) Surgical treatment of metastatic disease of the femur. J Am Acad Orthop Surg 8:56–65
Weill A, Chiras J, Simon JM et al (1996) Spinal metastases: indications for and results of percutaneous injection of acrylic surgical cement. Radiology. doi:10.1148/radiology.199.1.8633152
Anselmetti GC, Manca A, Ortega C et al (2008) Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Intervent Radiol 31:1165–1173
Tian Q-H, He C-J, Wu C-G et al (2015) Comparison of percutaneous cementoplasty with and without interventional internal fixation for impending malignant pathological fracture of the proximal femur. Cardiovasc Intervent Radiol 39:81–89
Liu X-W, Jin P, Liu K et al (2017) Comparison of percutaneous long bone cementoplasty with or without embedding a cement-filled catheter for painful long bone metastases with impending fracture. Eur Radiol 27:120–127
Deschamps F, Farouil G, Hakime A et al (2012) Cementoplasty of metastases of the proximal femur: is It a safe palliative option? J Vasc Interv Radiol 23:1311–1316
Kim Y, Kang HG, Kim TS et al (2014) Palliative percutaneous stabilization of lower extremity for bone metastasis using flexible nails and bone cement. Surg Oncol 23:192–198
Deschamps F, Farouil G, Hakime A et al (2011) Percutaneous stabilization of impending pathological fracture of the proximal femur. Cardiovasc Intervent Radiol 35:1428–1432
Young J, Badgery-Parker T, Dobbins T et al (2015) Comparison of ECOG/WHO performance status and ASA score as a measure of functional status. J Pain Symptom Manag 49:258–264
Singh RK, Chaturvedi JP, Agrawal HS, Agrawal N (2016) Lower limb orthopedic surgery in geriatric patients under paravertebral blocks: a prospective feasibility study. Med J Armed Forces India 72:215–219
Lin PP, Kang HG, Kim Y et al (2015) Minimally invasive surgery for femoral neck fractures using bone cement infusible hollow-perforated screw in high-risk patients with advanced cancer. Surg Oncol 24:226–231
Kang HG, Roh YW, Kim HS (2009) The treatment of metastasis to the femoral neck using percutaneous hollow perforated screws with cement augmentation. J Bone Joint Surg (Br) 91:1078–1082
Ristevski B, Jenkinson RJ, Stephen DJG et al (2009) Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Can J Surg J Can Chir 52:302–308
Thien TM, Chatziagorou G, Garellick G et al (2014) Periprosthetic femoral fracture within two years after total hip replacement: analysis of 437,629 operations in the nordic arthroplasty register association database. J Bone Joint Surg Am 96:e167
Kim Y, Kang HG, Kim S et al (2013) Clinical outcome prediction of percutaneous cementoplasty for metastatic bone tumor using (18)F-FDG PET-CT. Ann Nucl Med 27:916–923
Galibert P, Deramond H, Rosat P, Le Gars D (1987) Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty. Neurochirurgie 33:166–168
Clarençon F, Jean B, Pham H-P et al (2011) Value of percutaneous radiofrequency ablation with or without percutaneous vertebroplasty for pain relief and functional recovery in painful bone metastases. Skelet Radiol 42:25–36
Cazzato RL, Buy X, Eker O et al (2014) Percutaneous long bone cementoplasty of the limbs: experience with fifty-one non-surgical patients. Eur Radiol 24:3059–3068
Deschamps F, de Baere T, Hakime A et al (2016) Percutaneous osteosynthesis in the pelvis in cancer patients. Eur Radiol 26:1631–1639
Gao H, Liu Z, Wang B, Guo A (2016) Clinical and functional comparison of endoprosthetic replacement with intramedullary nailing for treating proximal femur metastasis. Chin J Cancer Res Chung-Kuo Yen Cheng Yen Chiu 28:209–214
Venmans A, Lohle PNM, van Rooij WJ et al (2008) Frequency and outcome of pulmonary polymethylmethacrylate embolism during percutaneous vertebroplasty. AJNR Am J Neuroradiol 29:1983–1985
Baroud G, Crookshank M, Bohner M (2006) High-viscosity cement significantly enhances uniformity of cement filling in vertebroplasty: an experimental model and study on cement leakage. Spine 31:2562–2568
Tins BJ, Cassar-Pullicino VN, Lalam R, Haddaway M (2012) Venous air embolism in consecutive balloon kyphoplasties visualised on CT imaging. Skelet Radiol 41:1093–1098
Andersen KH, Nielsen JM (1998) Heat of polymerization of bone cement can induce cardiac arrest. Ugeskr Laeger 160:4905–4906
Acknowledgements
The authors thank Mr Pierre Grare for his kind assistance with the English editing of the manuscript.
The scientific guarantor of this publication is Jacques Chiras. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. The design of the study and its content were approved by our local Institutional Review Board. The need for patient informed consent for retrospective analyses of records and imaging data was waived. Methodology: retrospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Premat, K., Clarençon, F., Bonaccorsi, R. et al. Reinforced cementoplasty using dedicated spindles in the management of unstable malignant lesions of the cervicotrochanteric region. Eur Radiol 27, 3973–3982 (2017). https://doi.org/10.1007/s00330-017-4774-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4774-3