Abstract
Purpose
To evaluate prospectively duration and effectiveness of aperistalsis achieved by glucagon(GLU) or hyoscine N-butylbromide(HBB) following various administration routes.
Materials and methods
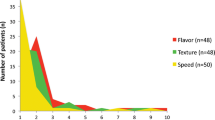
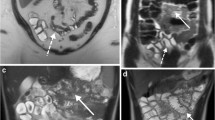
Six volunteers underwent Magnetic Resonance Imaging (MRI) after standardized oral preparation in random order five separate MR examinations with both spasmolytic agents (HBB intravenous(i.v.) or intramuscular(i.m.), GLU i.v. or i.m., and a combined scheme). The MR protocol included a sagittal 2D cross-section of the small bowel with a temporal resolution of 0.55 s acquired over 60 to 90 min. To quantify bowel motility, small bowel cross-sectional areas were summated over time.
Results
The anti-peristaltic i.v. effects of HBB and glucagon started on average after 85 s/65 s and ended after 21 min/23.3 min, respectively. By comparison, the anti-peristaltic effects of i.m. HBB and glucagon started significantly later 5.1/11.6 min (P = 0.001; Wilcoxon signed ranks test) and lasted for 17.7/28.2 min with greater inter-individual differences (P = 0.012; Brown-Forsythe test). The combined scheme resulted in a rapid onset after 65 s with effect duration of 31 min.
Conclusion
Anti-peristaltic effects on the small bowel are drug dependant, i.e., their onset is faster and more reliable when administering i.v. than i.m.. Combining i.v. GLU with i.m. HBB provides an early onset of effect, sustained spasmolysis and the highest degree of motility impairment.
Key Points
• Anti-persitaltic agents are widely used before various diagnostic procedures of the abdomen.
• The combination of iv-glucagon with im-hyoscine provides reliable spasmolysis with early onset.
• Intravenous spasmolysis is more reliable compared to intramuscular administration.
• Intravenous glucagon has a prolonged spasmolytic effect compared to intravenous hyoscine.





Similar content being viewed by others
References
Husebye E (1999) The patterns of small bowel motility: physiology and implications in organic disease and functional disorders. Neurogastroenterol Motil 11:141–161
Kozak RI, Bennett JD, Brown TC, Lee TY (1994) Reduction of bowel motion artifact during digital subtraction angiography: a comparison of hyoscine butylbromide and glucagon. Can Assoc Radiol J 45:209–211
Laniado M, Grönewäller E, Kopp AF et al (1997) The value of hyoscine butylbromide in abdominal MR imaging with and without oral magnetic particles. Abdom Imaging 22:381–388
Johnson W, Taylor MB, Carrington BM, Bonington SC, Swindell R (2007) The value of hyoscine butylbromide in pelvic MRI. Clin Radiol 62:1087–1093
Martí-Bonmatí L, Graells M, Ronchera-Oms CL (1996) Reduction of peristaltic artifacts on magnetic resonance imaging of the abdomen: a comparative evaluation of three drugs. Abdom Imaging 2:309–313
Wagner M, Klessen C, Rief M et al (2008) High-resolution T2-weighted abdominal magnetic resonance imaging using respiratory triggering: impact of butylscopolamine on image quality. Acta Radiol 49:376–382
Mayo KE, Miller LJ, Bataille D et al (2003) International Union of Pharmacology. XXXV. The glucagon receptor family. Pharmacol Rev 55:167–194
Dubé PE, Brubaker PL (2007) Frontiers in glucagon-like peptide-2: multiple actions, multiple mediators. Am J Physiol Endocrinol Metab 293:E460–E465
Tytgat GN (2008) Hyoscine butylbromide—a review on its parenteral use in acute abdominal spasm and as an aid in abdominal diagnostic and therapeutic procedures. Curr Med Res Opin 24:3159–3173
Huizinga JD, McKay CM, White EJ (2006) The many facets of intestinal peristalsis. Am J Physiol Gastrointest Liver Physiol 290:G1347–G1349
Stone AJ, Browne JE, Lennon B, Meaney JF, Fagan AJ (2011) Stone Quantification of accuracy of ADC measurements from Whole-body DWIBS. Proc Intl Soc Mag Reson Med 19:836
Rowland-Hill CA, Loveday EJ, Thomas ML (1989) A comparison of the value of hyoscine butylbromide and glucagon on aorto iliac intravenous digital subtraction. Vasa 18:301–303
Rogalla P, Lembcke A, Rückert JC et al (2005) Spasmolysis at CT colonography: butyl scopolamine versus glucagon. Radiology 236:184–188
Gutzeit A, Patak MA, von Weymarn C et al (2010) Feasibility of small bowel flow rate measurement with MRI. J Magn Reson Imaging 32:345–351
Froehlich JM, Daenzer M, von Weymarn C et al (2009) Aperistaltic effect of hyoscine N-butylbromide versus glucagon on the small bowel assessed by magnetic resonance imaging. Eur Radiol 19:1387–1393
Froehlich JM, Patak MA, von Weymarn C, Juli CF, Zollikofer CL, Wentz KU (2005) Small bowel motility assessment with magnetic resonance imaging. J Magn Reson Imaging 21:370–375
Wakamiya M, Furukawa A, Kanasaki S, Murata K (2011) Assessment of small bowel motility function with cine-MRI using balanced steady-state free precession sequence. J Magn Reson Imaging 33:1235–1240
Acknowledgement
We would like to thank Philips Healthcare Switzerland for their valuable technical support. We also thank Mr. Hofmann and Mr. Hartmann at our photography department of the Cantonal Hospital Winterthur for their well appreciated assistance in the production of illustrations and photographs. Moreover, we would like to acknowledge the help provided by Selina Froehlich supporting us in the post-processing of the data. Finally, our special thanks go as well to Dr. Eric Schoch, who performed the DSA images.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gutzeit, A., Binkert, C.A., Koh, DM. et al. Evaluation of the anti-peristaltic effect of glucagon and hyoscine on the small bowel: comparison of intravenous and intramuscular drug administration. Eur Radiol 22, 1186–1194 (2012). https://doi.org/10.1007/s00330-011-2366-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-011-2366-1