Abstract
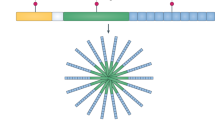
Autoinflammatory diseases are a genetically heterogeneous group of rheumatologic diseases that are driven by abnormal activation of the innate immune system. Patients present with recurrent episodes of systemic inflammation and a spectrum of organ-specific comorbidities. These diseases are mediated by the overproduction of various inflammatory cytokines, such as IL-1, IL-18, IL-6, TNFα, and type I interferon. Treatments with biologic agents that inhibit these cytokines have been very efficient in most patients. During the past 2 years, remarkable progress has been made in the identification of disease-associated genes owing mostly to new technologies. Next generation sequencing technologies (NGS) have become instrumental in finding single-gene defects in undiagnosed patients with early onset symptoms. NGS has advanced the field of autoinflammation by identifying disease-causing genes that point to pathways not known to regulate cytokine signaling or inflammation. They include a protein that has a role in differentiation of myeloid cells, a ubiquitously expressed enzyme that catalyzes the addition of the CCA terminus to the 3-prime end of tRNA precursors, and an enzyme that catalyzes the oxidation of a broad range of substrates. Lastly, newly described mutations have informed a whole new dimension on genotype-phenotype relationships. Mutations in the same gene can give rise to a range of phenotypes with a common inflammatory component. This suggests greater than anticipated contributions by modifying alleles and environmental factors to disease expressivity.

Similar content being viewed by others
References
Ombrello MJ, Sikora KA, Kastner DL (2014) Genetics, genomics, and their relevance to pathology and therapy. Best Pract Res Clin Rheumatol 28:175–189
Zhou Q et al (2014) Early-onset stroke and vasculopathy associated with mutations in ADA2. N Engl J Med 370:911–920
Navon Elkan P et al (2014) Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N Engl J Med 370:921–931
Garg N et al (2014) Novel adenosine deaminase 2 mutations in a child with a fatal vasculopathy. Eur J Pediatr 173:827–830
van Montfrans J, Zavialov A, Zhou Q (2014) Mutant ADA2 in vasculopathies. N Engl J Med 371:478
Van Eyck L, Liston A, Meyts I (2014) Mutant ADA2 in vasculopathies. N Engl J Med 371:478–479
Bras J, Guerreiro R, Santo GC (2014) Mutant ADA2 in vasculopathies. N Engl J Med 371:478–480
Van Eyck L, Liston A, Wouters C (2014) Mutant ADA2 in vasculopathies. N Engl J Med 371:480
Zavialov AV, Yu X, Spillmann D, Lauvau G, Zavialov AV (2010) Structural basis for the growth factor activity of human adenosine deaminase ADA2. J Biol Chem 285:12367–12377
Iijima R et al (2008) The extracellular adenosine deaminase growth factor, ADGF/CECR1, plays a role in Xenopus embryogenesis via the adenosine/P1 receptor. J Biol Chem 283:2255–2264
Dolezal T, Dolezelova E, Zurovec M, Bryant PJ (2005) A role for adenosine deaminase in Drosophila larval development. PLoS Biol 3:e201
Zavialov AV et al (2010) Human adenosine deaminase 2 induces differentiation of monocytes into macrophages and stimulates proliferation of T helper cells and macrophages. J Leukoc Biol 88:279–290
Belot A et al (2014) Mutations in CECR1 associated with a neutrophil signature in peripheral blood. Pediatr Rheumatol Online J 12:44
Van Eyck L Jr et al (2015) Hematopoietic stem cell transplantation rescues the immunologic phenotype and prevents vasculopathy in patients with adenosine deaminase 2 deficiency. J Allergy Clin Immunol 135:283–287, e5
Liu Y et al (2014) Activated STING in a vascular and pulmonary syndrome. N Engl J Med 371:507–518
Jeremiah N et al (2014) Inherited STING-activating mutation underlies a familial inflammatory syndrome with lupus-like manifestations. J Clin Invest 124:5516–5520
Burdette DL et al (2011) STING is a direct innate immune sensor of cyclic di-GMP. Nature 478:515–518
Barber GN (2014) STING-dependent cytosolic DNA sensing pathways. Trends Immunol 35:88–93
Burdette DL, Vance RE (2013) STING and the innate immune response to nucleic acids in the cytosol. Nat Immunol 14:19–26
Ishikawa H, Barber GN (2008) STING is an endoplasmic reticulum adaptor that facilitates innate immune signalling. Nature 455:674–678
Zhang L et al (2014) NLRC3, a member of the NLR family of proteins, is a negative regulator of innate immune signaling induced by the DNA sensor STING. Immunity 40:329–341
Boyce BF, Xing L (2007) The RANKL/RANK/OPG pathway. Curr Osteoporos Rep 5:98–104
Walsh MC, Choi Y (2014) Biology of the RANKL-RANK-OPG system in immunity, bone, and beyond. Front Immunol 5:511
Soysa NS, Alles N, Aoki K, Ohya K (2012) Osteoclast formation and differentiation: an overview. J Med Dent Sci 59:65–74
Whyte MP (2006) Paget's disease of bone and genetic disorders of RANKL/OPG/RANK/NF-kappaB signaling. Ann N Y Acad Sci 1068:143–164
Hanada R et al (2009) Central control of fever and female body temperature by RANKL/RANK. Nature 462:505–509
Jeru I et al (2014) Brief Report: Involvement of TNFRSF11A molecular defects in autoinflammatory disorders. Arthritis Rheumatol 66:2621–2627
Anderson DM et al (1997) A homologue of the TNF receptor and its ligand enhance T-cell growth and dendritic-cell function. Nature 390:175–179
Dougall WC et al (1999) RANK is essential for osteoclast and lymph node development. Genes Dev 13:2412–2424
Canna SW et al (2014) An activating NLRC4 inflammasome mutation causes autoinflammation with recurrent macrophage activation syndrome. Nat Genet 46:1140–1146
Romberg N et al (2014) Mutation of NLRC4 causes a syndrome of enterocolitis and autoinflammation. Nat Genet 46:1135–1139
Kitamura A, Sasaki Y, Abe T, Kano H, Yasutomo K (2014) An inherited mutation in NLRC4 causes autoinflammation in human and mice. J Exp Med 211:2385–2396
Franchi L et al (2006) Cytosolic flagellin requires Ipaf for activation of caspase-1 and interleukin 1beta in salmonella-infected macrophages. Nat Immunol 7:576–582
Vance RE (2015) The NAIP/NLRC4 inflammasomes. Curr Opin Immunol 32C:84–89
Sellin ME et al (2014) Epithelium-intrinsic NAIP/NLRC4 inflammasome drives infected enterocyte expulsion to restrict Salmonella replication in the intestinal mucosa. Cell Host Microbe 16:237–248
Zhao Y et al (2011) The NLRC4 inflammasome receptors for bacterial flagellin and type III secretion apparatus. Nature 477:596–600
Nordlander S, Pott J, Maloy KJ (2014) NLRC4 expression in intestinal epithelial cells mediates protection against an enteric pathogen. Mucosal Immunol 7:775–785
Wiseman DH et al (2013) A novel syndrome of congenital sideroblastic anemia, B-cell immunodeficiency, periodic fevers, and developmental delay (SIFD). Blood 122:112–123
Chakraborty PK et al (2014) Mutations in TRNT1 cause congenital sideroblastic anemia with immunodeficiency, fevers, and developmental delay (SIFD). Blood 124:2867–2871
Sasarman F, et al (2015) The 3' addition of CCA to mitochondrial tRNASer(AGY) is specifically impaired in patients with mutations in the tRNA nucleotidyl transferase TRNT1. Hum Mol Genet
Xiong Y, Steitz TA (2006) A story with a good ending: tRNA 3'-end maturation by CCA-adding enzymes. Curr Opin Struct Biol 16:12–17
Cimaz R, Von Scheven A, Hofer M (2012) Systemic-onset juvenile idiopathic arthritis: the changing life of a rare disease. Swiss Med Wkly 142:w13582
Pascual V et al (2008) How the study of children with rheumatic diseases identified interferon-alpha and interleukin-1 as novel therapeutic targets. Immunol Rev 223:39–59
Pascual V, Allantaz F, Arce E, Punaro M, Banchereau J (2005) Role of interleukin-1 (IL-1) in the pathogenesis of systemic onset juvenile idiopathic arthritis and clinical response to IL-1 blockade. J Exp Med 201:1479–1486
Wakil SM et al (2015) Association of a mutation in LACC1 with a monogenic form of systemic juvenile idiopathic arthritis. Arthritis Rheumatol 67:288–295
Wong SH, Hill AV, Vannberg FO, India-Africa-United Kingdom Leprosy Genetics, C (2010) Genomewide association study of leprosy. N Engl J Med 362:1446–7, author reply 1447-8
Zhang FR et al (2009) Genomewide association study of leprosy. N Engl J Med 361:2609–2618
Sales-Marques C et al (2014) NOD2 and CCDC122-LACC1 genes are associated with leprosy susceptibility in Brazilians. Hum Genet 133:1525–1532
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is a contribution to the Special Issue on The Inflammasome and Autoinflammatory Diseases - Guest Editors: Seth L. Masters, Tilmann Kallinich and Seza Ozen
Rights and permissions
About this article
Cite this article
Aksentijevich, I. Update on genetics and pathogenesis of autoinflammatory diseases: the last 2 years. Semin Immunopathol 37, 395–401 (2015). https://doi.org/10.1007/s00281-015-0478-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-015-0478-4