Abstract
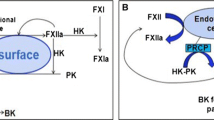
The contact system is a plasma protease cascade that is initiated by coagulation factor XII activation on cardiovascular cells. The system starts procoagulant and proinflammatory reactions, via the intrinsic pathway of coagulation or the kallikrein–kinin system, respectively. The biochemistry of the contact system in vitro is well understood, however, its in vivo functions are just beginning to emerge. Data obtained in genetically engineered mice have revealed an essential function of the contact system for thrombus formation. Severe deficiency in contact system proteases impairs thrombus formation but does not reduce the hemostatic capacity of affected individuals. The system is activated by an inorganic polymer, polyphosphate that is released from activated platelets. Excessive inherited activation of the contact system causes a life-threatening swelling disorder, hereditary angioedema. Activation of the contact system by pathogens contributes to leakage in bacterial infections. Mast-cell-derived heparin triggers contact-system-mediated edema formation with implications for allergic disease states. Here we present an overview about the plasma contact system in occlusive and inflammatory disease and its contribution to health and pathology.



Similar content being viewed by others
References
Mackman N (2008) Triggers, targets and treatments for thrombosis. Nature 451(7181):914–918
Macfarlane RG (1964) An enzyme cascade in the blood clotting mechanism, and its function as a biochemical amplifier. Nature 202:498–499
Colman RW (2006) Contact activation pathway: Inflammatory, fibrinolytic, anticoagulant, antiadhesive, and antiangiogenic activities. Hemostasis and Thormbosis, Basic Principles and Clinical Practice, 5 edn. Lippincott Williams & Wilkins, Philadelphia
Renne T, Gailani D, Meijers JC, Muller-Esterl W (2002) Characterization of the H-kininogen-binding site on factor XI: a comparison of factor XI and plasma prekallikrein. J Biol Chem 277(7):4892–4899. doi:10.1074/jbc.M105221200
Muller F, Renne T (2008) Novel roles for factor XII-driven plasma contact activation system. Curr Opin Hematol 15(5):516–521
Renne T, Dedio J, David G, Muller-Esterl W (2000) High molecular weight kininogen utilizes heparan sulfate proteoglycans for accumulation on endothelial cells. J Biol Chem 275(43):33688–33696
Renne T, Muller-Esterl W (2001) Cell surface-associated chondroitin sulfate proteoglycans bind contact phase factor H-kininogen. FEBS Lett 500(1–2):36–40
Renne T, Schuh K, Muller-Esterl W (2005) Local bradykinin formation is controlled by glycosaminoglycans. J Immunol 175(5):3377–3385
Leeb-Lundberg LM, Marceau F, Muller-Esterl W, Pettibone DJ, Zuraw BL (2005) Classification of the kinin receptor family: from molecular mechanisms to pathophysiological consequences. Pharmacol Rev 57(1):27–77
Raslan F, Schwarz T, Meuth SG, Austinat M, Bader M, Renne T, Roosen K, Stoll G, Siren AL, Kleinschnitz C (2010) Inhibition of bradykinin receptor B1 protects mice from focal brain injury by reducing blood–brain barrier leakage and inflammation. J Cereb Blood Flow Metab 30(8):1477–1486. doi:10.1038/jcbfm.2010.28
Schulze-Topphoff U, Prat A, Prozorovski T, Siffrin V, Paterka M, Herz J, Bendix I, Ifergan I, Schadock I, Mori MA, Van Horssen J, Schroter F, Smorodchenko A, Han MH, Bader M, Steinman L, Aktas O, Zipp F (2009) Activation of kinin receptor B1 limits encephalitogenic T lymphocyte recruitment to the central nervous system. Nat Med 15(7):788–793. doi:10.1038/nm.1980
Ratnoff OD, Colopy JE (1955) A familial hemorrhagic trait associated with a deficiency of a clot-promoting fraction of plasma. J Clin Invest 34(4):602–613
Gailani D, Renne T (2007) The intrinsic pathway of coagulation: a target for treating thromboembolic disease? J Thromb Haemost 5(6):1106–1112. doi:10.1111/j.1538-7836.2007.02446.x
Gailani D, Broze GJ Jr (1991) Factor XI activation in a revised model of blood coagulation. Science 253(5022):909–912
Mackman N (2004) Role of tissue factor in hemostasis, thrombosis, and vascular development. Arterioscler Thromb Vasc Biol 24(6):1015–1022, Epub 2004 Apr 1029
Pauer HU, Renne T, Hemmerlein B, Legler T, Fritzlar S, Adham I, Muller-Esterl W, Emons G, Sancken U, Engel W, Burfeind P (2004) Targeted deletion of murine coagulation factor XII gene—a model for contact phase activation in vivo. Thromb Haemost 92(3):503–508
Renne T, Pozgajova M, Gruner S, Schuh K, Pauer HU, Burfeind P, Gailani D, Nieswandt B (2005) Defective thrombus formation in mice lacking coagulation factor XII. J Exp Med 202(2):271–281, Epub 2005 Jul 2011
Doolittle RF (2011) Coagulation in vertebrates with a focus on evolution and inflammation. J Innate Immun 3(1):9–16. doi:10.1159/000321005
Kleinschnitz C, Stoll G, Bendszus M, Schuh K, Pauer HU, Burfeind P, Renne C, Gailani D, Nieswandt B, Renne T (2006) Targeting coagulation factor XII provides protection from pathological thrombosis in cerebral ischemia without interfering with hemostasis. J Exp Med 203(3):513–518
Hagedorn I, Schmidbauer S, Pleines I, Kleinschnitz C, Kronthaler U, Stoll G, Dickneite G, Nieswandt B (2010) Factor XIIa inhibitor recombinant human albumin Infestin-4 abolishes occlusive arterial thrombus formation without affecting bleeding. Circulation 121(13):1510–1517. doi:10.1161/CIRCULATIONAHA.109.924761
Renne T, Gailani D (2007) Role of Factor XII in hemostasis and thrombosis: clinical implications. Expert Rev Cardiovasc Ther 5(4):733–741
Muller F, Mutch NJ, Schenk WA, Smith SA, Esterl L, Spronk HM, Schmidbauer S, Gahl WA, Morrissey JH, Renne T (2009) Platelet polyphosphates are proinflammatory and procoagulant mediators in vivo. Cell 139(6):1143–1156. doi:10.1016/j.cell.2009.11.001
Cheng Q, Tucker EI, Pine MS, Sisler I, Matafonov A, Sun MF, White-Adams TC, Smith SA, Hanson SR, McCarty OJ, Renne T, Gruber A, Gailani D (2010) A role for factor XIIa-mediated factor XI activation in thrombus formation in vivo. Blood. doi:10.1182/blood-2010-02-270918
Kravtsov DV, Matafonov A, Tucker EI, Sun MF, Walsh PN, Gruber A, Gailani D (2009) Factor XI contributes to thrombin generation in the absence of factor XII. Blood 114(2):452–458. doi:10.1182/blood-2009-02-203604
Meijers JC (2009) Feedback controversy stops here. Blood 114(2):235. doi:10.1182/blood-2009-04-217117
Ratnoff OD (1968) The demise of John Hageman. N Engl J Med 279:760–761
Girolami A, Morello M, Girolami B, Lombardi AM, Bertolo C (2005) Myocardial infarction and arterial thrombosis in severe (homozygous) FXII deficiency: no apparent causative relation. Clin Appl Thromb Hemost 11(1):49–53
Koster T, Rosendaal FR, Briet E, Vandenbroucke JP (1994) John Hageman’s factor and deep-vein thrombosis: Leiden thrombophilia Study. Br J Haematol 87(2):422–424
Zeerleder S, Schloesser M, Redondo M, Wuillemin WA, Engel W, Furlan M, Lammle B (1999) Reevaluation of the incidence of thromboembolic complications in congenital factor XII deficiency—a study on 73 subjects from 14 Swiss families. Thromb Haemost 82(4):1240–1246
Seligsohn U (2009) Factor XI deficiency in humans. J Thromb Haemost 7(Suppl 1):84–87. doi:10.1111/j.1538-7836.2009.03395.x
Salomon O, Steinberg DM, Koren-Morag N, Tanne D, Seligsohn U (2008) Reduced incidence of ischemic stroke in patients with severe factor XI deficiency. Blood 111(8):4113–4117
Salomon O, Zivelin A, Tamarin I, Steinberg DM, Varon D, Seligsohn U (2009) Patients with severe Factor XI deficiency have a reduced incidence of venous thromboembolism. Blood 114(22):3491A
Mangal AK, Naiman SC (1980) Hageman factor deficiency and oral contraceptives. Lancet 1(8171):774
Pluthero FG, Ryan C, Williams S, Brandao LR, Kahr WH (2011) Decreased in vitro thrombin generation and clot stability in human FXII-null blood and plasma. Br J Haematol 152(1):111–112. doi:10.1111/j.1365-2141.2010.08382.x
Endler G, Marsik C, Jilma B, Schickbauer T, Quehenberger P, Mannhalter C (2007) Evidence of a U-shaped association between factor XII activity and overall survival. J Thromb Haemost 5(6):1143–1148. doi:10.1111/j.1538-7836.2007.02530.x
Ghebrehiwet B, Silverberg M, Kaplan AP (1981) Activation of the classical pathway of complement by Hageman factor fragment. J Exp Med 153(3):665–676
Zuraw BL (2008) Hereditary angiodema: a current state-of-the-art review, IV: short- and long-term treatment of hereditary angioedema: out with the old and in with the new? Ann Allergy Asthma Immunol 100(1 Suppl 2):S13–S18
Davis AE 3rd (2008) Hereditary angioedema: a current state-of-the-art review, III: mechanisms of hereditary angioedema. Ann Allergy Asthma Immunol 100(1 Suppl 2):S7–S12
Bork K, Barnstedt SE, Koch P, Traupe H (2000) Hereditary angioedema with normal C1-inhibitor activity in women. Lancet 356(9225):213–217
Han ED, MacFarlane RC, Mulligan AN, Scafidi J, Davis AE 3rd (2002) Increased vascular permeability in C1 inhibitor-deficient mice mediated by the bradykinin type 2 receptor. J Clin Invest 109(8):1057–1063
Cugno M, Cicardi M, Bottasso B, Coppola R, Paonessa R, Mannucci PM, Agostoni A (1997) Activation of the coagulation cascade in C1-inhibitor deficiencies. Blood 89(9):3213–3218
Nussberger J, Cugno M, Cicardi M (2002) Bradykinin-mediated angioedema. N Engl J Med 347(8):621–622
Zuraw BL, Busse PJ, White M, Jacobs J, Lumry W, Baker J, Craig T, Grant JA, Hurewitz D, Bielory L, Cartwright WE, Koleilat M, Ryan W, Schaefer O, Manning M, Patel P, Bernstein JA, Friedman RA, Wilkinson R, Tanner D, Kohler G, Gunther G, Levy R, McClellan J, Redhead J, Guss D, Heyman E, Blumenstein BA, Kalfus I, Frank MM (2010) Nanofiltered C1 inhibitor concentrate for treatment of hereditary angioedema. N Engl J Med 363(6):513–522. doi:10.1056/NEJMoa0805538
Cicardi M, Banerji A, Bracho F, Malbran A, Rosenkranz B, Riedl M, Bork K, Lumry W, Aberer W, Bier H, Bas M, Greve J, Hoffmann TK, Farkas H, Reshef A, Ritchie B, Yang W, Grabbe J, Kivity S, Kreuz W, Levy RJ, Luger T, Obtulowicz K, Schmid-Grendelmeier P, Bull C, Sitkauskiene B, Smith WB, Toubi E, Werner S, Anne S, Bjorkander J, Bouillet L, Cillari E, Hurewitz D, Jacobson KW, Katelaris CH, Maurer M, Merk H, Bernstein JA, Feighery C, Floccard B, Gleich G, Hebert J, Kaatz M, Keith P, Kirkpatrick CH, Langton D, Martin L, Pichler C, Resnick D, Wombolt D, Fernandez Romero DS, Zanichelli A, Arcoleo F, Knolle J, Kravec I, Dong L, Zimmermann J, Rosen K, Fan WT (2010) Icatibant, a new bradykinin-receptor antagonist, in hereditary angioedema. N Engl J Med 363(6):532–541. doi:10.1056/NEJMoa0906393
Cicardi M, Levy RJ, McNeil DL, Li HH, Sheffer AL, Campion M, Horn PT, Pullman WE (2010) Ecallantide for the treatment of acute attacks in hereditary angioedema. N Engl J Med 363(6):523–531. doi:10.1056/NEJMoa0905079
Cichon S, Martin L, Hennies HC, Muller F, Van Driessche K, Karpushova A, Stevens W, Colombo R, Renne T, Drouet C, Bork K, Nothen MM (2006) Increased activity of coagulation Factor XII (Hageman Factor) causes hereditary angioedema type III. Am J Hum Genet 79(6):1098–1104, Epub 2006 Oct 1018
Dewald G, Bork K (2006) Missense mutations in the coagulation factor XII (Hageman factor) gene in hereditary angioedema with normal C1 inhibitor. Biochem Biophys Res Commun 343(4):1286–1289
Bork K, Kleist R, Hardt J, Witzke G (2009) Kallikrein–kinin system and fibrinolysis in hereditary angioedema due to factor XII gene mutation Thr309Lys. Blood Coagul Fibrinolysis 20(5):325–332. doi:10.1097/MBC.0b013e32832811f8
Briseid K, Hoem NO, Johannesen S, Fossum S (1991) Contact activation factors in plasma from pregnant women—increased level of an association between factor XII and kallikrein. Thromb Res 61(2):123–133
Bouillet L, Longhurst H, Boccon-Gibod I, Bork K, Bucher C, Bygum A, Caballero T, Drouet C, Farkas H, Massot C, Nielsen EW, Ponard D, Cicardi M (2008) Disease expression in women with hereditary angioedema. Am J Obstet & Gynecol 199(5):484.e1–484.e4
Gailani D, Renne T (2007) Intrinsic pathway of coagulation and arterial thrombosis. Arterioscler Thromb Vasc Biol 27(12):2507–2513
Proud D, Kaplan AP (1988) Kinin formation: mechanisms and role in inflammatory disorders. Annu Rev Immunol 6:49–83
Proud D, Togias A, Naclerio RM, Crush SA, Norman PS, Lichtenstein LM (1983) Kinins are generated in vivo following nasal airway challenge of allergic individuals with allergen. J Clin Invest 72(5):1678–1685
Noga O, Brunnee T, Schaper C, Kunkel G (1999) Heparin, derived from the mast cells of human lungs is responsible for the generation of kinins in allergic reactions due to the activation of the contact system. Int Arch Allergy Immunol 120(4):310–316
Brunnee T, Reddigari SR, Shibayama Y, Kaplan AP, Silverberg M (1997) Mast cell derived heparin activates the contact system: a link to kinin generation in allergic reactions. Clin Exp Allergy 27(6):653–663
Hojima Y, Cochrane CG, Wiggins RC, Austen KF, Stevens RL (1984) In vitro activation of the contact (Hageman factor) system of plasma by heparin and chondroitin sulfate E. Blood 63(6):1453–1459
Marshall JS (2004) Mast-cell responses to pathogens. Nat Rev Immunol 4(10):787–799
Galli SJ, Grimbaldeston M, Tsai M (2008) Immunomodulatory mast cells: negative, as well as positive, regulators of immunity. Nat Rev Immunol 8(6):478–486
Humphries DE, Wong GW, Friend DS, Gurish MF, Qiu WT, Huang C, Sharpe AH, Stevens RL (1999) Heparin is essential for the storage of specific granule proteases in mast cells. Nature 400(6746):769–772
Forsberg E, Pejler G, Ringvall M, Lunderius C, Tomasini-Johansson B, Kusche-Gullberg M, Eriksson I, Ledin J, Hellman L, Kjellen L (1999) Abnormal mast cells in mice deficient in a heparin-synthesizing enzyme. Nature 400(6746):773–776
Oschatz C, Maas C, Lecher B, Jansen T, Bjorkqvist J, Tradler T, Sedlmeier R, Burfeind P, Cichon S, Hammerschmidt S, Muller-Esterl W, Wuillemin WA, Nilsson G, Renne T (2011) Mast cells increase vascular permeability by heparin-initiated bradykinin formation in vivo. Immunity 34(2):258–268. doi:10.1016/j.immuni.2011.02.008
Kilinc E, van Oerle R, Borissoff JI, Oschatz C, Gerlofs-Nijland ME, Janssen NA, Cassee FR, Sandstrom T, Renne T, Ten Cate H, Spronk HM (2011) Factor XII activation is essential to sustain the procoagulant effects of particulate matter. J Thromb Haemost. doi:10.1111/j.1538-7836.2011.04280.x
Herwald H, Morgelin M, Olsen A, Rhen M, Dahlback B, Muller-Esterl W, Bjorck L (1998) Activation of the contact-phase system on bacterial surfaces—a clue to serious complications in infectious diseases. Nat Med 4(3):298–302
Persson K, Morgelin M, Lindbom L, Alm P, Bjorck L, Herwald H (2000) Severe lung lesions caused by Salmonella are prevented by inhibition of the contact system. J Exp Med 192(10):1415–1424
Gao BB, Clermont A, Rook S, Fonda SJ, Srinivasan VJ, Wojtkowski M, Fujimoto JG, Avery RL, Arrigg PG, Bursell SE, Aiello LP, Feener EP (2007) Extracellular carbonic anhydrase mediates hemorrhagic retinal and cerebral vascular permeability through prekallikrein activation. Nat Med 13(2):181–188
Zuraw BL (2008) Clinical practice. Hereditary angioedema. N Engl J Med 359(10):1027–1036
Guerrini M, Beccati D, Shriver Z, Naggi A, Viswanathan K, Bisio A, Capila I, Lansing JC, Guglieri S, Fraser B, Al-Hakim A, Gunay NS, Zhang Z, Robinson L, Buhse L, Nasr M, Woodcock J, Langer R, Venkataraman G, Linhardt RJ, Casu B, Torri G, Sasisekharan R (2008) Oversulfated chondroitin sulfate is a contaminant in heparin associated with adverse clinical events. Nat Biotechnol 26(6):669–675. doi:10.1038/nbt1407
Kishimoto TK, Viswanathan K, Ganguly T, Elankumaran S, Smith S, Pelzer K, Lansing JC, Sriranganathan N, Zhao G, Galcheva-Gargova Z, Al-Hakim A, Bailey GS, Fraser B, Roy S, Rogers-Cotrone T, Buhse L, Whary M, Fox J, Nasr M, Dal Pan GJ, Shriver Z, Langer RS, Venkataraman G, Austen KF, Woodcock J, Sasisekharan R (2008) Contaminated heparin associated with adverse clinical events and activation of the contact system. N Engl J Med 358(23):2457–2467
Samuel M, Pixley RA, Villanueva MA, Colman RW, Villanueva GB (1992) Human factor XII (Hageman factor) autoactivation by dextran sulfate. Circular dichroism, fluorescence, and ultraviolet difference spectroscopic studies. J Biol Chem 267(27):19691–19697
Siebeck M, Cheronis JC, Fink E, Kohl J, Spies B, Spannagl M, Jochum M, Fritz H (1994) Dextran sulfate activates contact system and mediates arterial hypotension via B2 kinin receptors. J Appl Physiol 77(6):2675–2680
Schwartz LB (2008) Heparin comes clean. N Engl J Med 358(23):2505–2509
Fareed J, Walenga JM, Hoppensteadt D, Huan X, Nonn R (1989) Biochemical and pharmacologic inequivalence of low molecular weight heparins. Ann N Y Acad Sci 556:333–353
Wilner GD, Nossel HL, LeRoy EC (1968) Activation of Hageman factor by collagen. J Clin Invest 47(12):2608–2615
van der Meijden PE, Munnix IC, Auger JM, Govers-Riemslag JW, Cosemans JM, Kuijpers MJ, Spronk HM, Watson SP, Renne T, Heemskerk JW (2009) Dual role of collagen in factor XII-dependent thrombus formation. Blood 114(4):881–890. doi:10.1182/blood-2008-07-171066
Reininger AJ, Bernlochner I, Penz SM, Ravanat C, Smethurst P, Farndale RW, Gachet C, Brandl R, Siess W (2010) A 2-step mechanism of arterial thrombus formation induced by human atherosclerotic plaques. J Am Coll Cardiol 55(11):1147–1158. doi:10.1016/j.jacc.2009.11.051
Castaldi PA, Larrieu MJ, Caen J (1965) Availability of platelet Factor 3 and activation of factor XII in thrombasthenia. Nature 207(995):422–424
Walsh PN, Griffin JH (1981) Contributions of human platelets to the proteolytic activation of blood coagulation factors XII and XI. Blood 57(1):106–118
Ruiz FA, Lea CR, Oldfield E, Docampo R (2004) Human platelet dense granules contain polyphosphate and are similar to acidocalcisomes of bacteria and unicellular eukaryotes. J Biol Chem 279(43):44250–44257
Smith SA, Mutch NJ, Baskar D, Rohloff P, Docampo R, Morrissey JH (2006) Polyphosphate modulates blood coagulation and fibrinolysis. Proc Natl Acad Sci U S A 103(4):903–908, Epub 2006 Jan 2012
Muller F, Renne T (2011) Platelet polyphosphates: the nexus of primary and secondary hemostasis. Scand J Clin Lab Invest 71(2):82–86. doi:10.3109/00365513.2010.550312
Maas C, Govers-Riemslag JW, Bouma B, Schiks B, Hazenberg BP, Lokhorst HM, Hammarstrom P, ten Cate H, de Groot PG, Bouma BN, Gebbink MF (2008) Misfolded proteins activate factor XII in humans, leading to kallikrein formation without initiating coagulation. J Clin Invest 118(9):3208–3218
van der Meijden PE, Heemskerk JW (2010) Polyphosphates: a link between platelet activation, intrinsic coagulation and inflammation? Expert Rev Hematol 3(3):269–272. doi:10.1586/ehm.10.26
Acknowledgments
This work was supported in part by grants from Vetenskapsrådet (K2010-64X-21462-01-3), Hjärt Lungfonden (20090642), Stockholms läns landsting (ALF, 20090540), Cancerfonden (100615), and the Federal Ministry of Education and Research (BMBF)-funded ERARE and 01EO1003 programs to TR. Dr. Felicitas Müller, Stockholm is acknowledged for carefully revising the manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is published as part of the Special Issue on Coagulation & Inflammation [34:1]
Rights and permissions
About this article
Cite this article
Renné, T. The procoagulant and proinflammatory plasma contact system. Semin Immunopathol 34, 31–41 (2012). https://doi.org/10.1007/s00281-011-0288-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00281-011-0288-2