Abstract
Purpose
This phase 1 study assessed the safety, tolerability, pharmacokinetics, and preliminary antitumor activity of linifanib in Japanese patients with advanced solid tumors.
Methods
Patients were assigned to one of four sequential cohorts (0.05, 0.10, 0.20, or 0.25 mg/kg) of oral, once-daily linifanib on a 21-day cycle. Adverse events (AEs) were assessed per common terminology criteria for adverse events v3.0; tumor responses were assessed by response evaluation criteria in solid tumors.
Results
Eighteen patients were enrolled. Eleven (61%) received ≥3 prior therapies. Dose-limiting toxicities were Grade 3 ALT increase (0.10 mg/kg linifanib) and Grade 1 T-wave inversion (0.25 mg/kg linifanib) requiring dose interruption for >7 days and discontinuation on day 29. The most common linifanib-related AE was hypertension. Other significant treatment-related AEs included proteinuria, fatigue, and palmar-plantar erythrodysaesthesia. Linifanib pharmacokinetics were dose-proportional across 0.10–0.25 mg/kg. Two patients (11.1%) had confirmed partial responses, 12 had a best response of stable disease (11 had stable disease for ≥12 weeks), and four patients were not evaluable due to incomplete data. Four patients (lung cancer, breast cancer, thymic cancer, sarcoma) have continued linifanib for ≥48 weeks (range, 48–96+ weeks).
Conclusion
Linifanib was well tolerated with promising preliminary clinical activity in Japanese patients. Later-phase global studies examining linifanib efficacy will include Japanese patients.
Similar content being viewed by others
Introduction
Angiogenesis is a complex process of vascular network formation essential for growth and metastasis of both normal and tumor cells, supported by vascular endothelial growth factors (VEGF) and platelet-derived growth factors (PDGF) binding to the receptor tyrosine kinases (RTKs) VEGFR and PDGFR [1–4]. Excessive production of VEGF, PDGF, and placental growth factor (PlGF) by solid tumor cells can result in excessive angiogenesis [5], and dysregulation of growth-factor/RTK interactions on tumors and tumor vasculature can result in increased tumor growth and metastasis [4]. Consequently, the inhibition of VEGF, PDGF, and their RTKs is a potential target for cancer therapy [6, 7].
Small-molecule RTK inhibitors constitute the largest category of antiangiogenic anticancer drugs. Three RTK inhibitors, sorafenib, sunitinib, and pazopanib, target multiple receptors including VEGFR and PDGFR, and are approved for treatment in various solid tumor types. Other multiple RTK inhibitors in development for treatment of solid tumors include axitinib, motesanib, vandetanib, cediranib, brivanib, and SU14813. Combined inhibition of VEGFR and PDGFR is hypothesized to have a greater antitumor effect than inhibition of individual receptors [8]. Multiple-targeted RTK inhibitors, however, lack target specificity, which can result in unexpected toxicity, including fatigue, rash, myalgia, and hand-foot syndrome [5].
Linifanib (ABT-869) is a novel, potent inhibitor with selectivity for the VEGFR and PDGFR family of receptor tyrosine kinases. It has specific inhibitory activity against VEGFR-1, VEGFR-2, PDGFRβ, colony-stimulating factor 1 receptor, and fms-related tyrosine kinase 3, with minimal activity against unrelated tyrosine and serine/threonine kinases [9–11]. In preclinical studies with multiple human tumor xenograft models, linifanib demonstrated potent antiangiogenic and antitumor effects [9–13]. In a phase 1 study, single-agent linifanib demonstrated safety and activity in Asian patients with refractory solid malignancies [14]. Linifanib has also shown antitumor activity in phase 2 studies in patients with non-small cell lung cancer [15], hepatocellular carcinoma, or renal cell carcinoma (preliminary results) [16, 17].
This phase 1 study evaluated the pharmacokinetics, safety, and tolerability of linifanib in Japanese patients with solid tumors, at doses similar to those in the phase 1 study in Asian patients [14], and conducted a preliminary assessment of antitumor activity.
Patients and methods
Patients
Eligible patients were aged 20–75 years, with a histologically or cytologically confirmed solid tumor refractory to standard therapies or for which a standard effective therapy did not exist, Eastern Cooperative Oncology Group Performance Status (ECOG PS) 0–2, and adequate renal, hepatic, and bone marrow function (absolute neutrophil count ≥1,000/μL, platelets ≥100,000/μL, and hemoglobin ≥9.0 g/dL). Exclusion criteria included body weight ≤41 kg (0.05 and 0.10 mg/kg cohort) or ≥63 kg (0.05 mg/kg cohort), central nervous system metastasis, proteinuria greater than Grade 1 per the National Cancer Institute Common Terminology Criteria for Adverse Events version 3.0 (CTCAE v3) [18], hypertension (systolic/diastolic blood pressure >150/>95 mmHg), left ventricular ejection fraction <50%, and serum positivity for human immunodeficiency virus, or hepatitis B or C virus.
Study design and treatment
This phase 1, open-label, dose-escalating study [19] was approved by the institutional review boards and ethics committees at the National Cancer Center Hospital (NCCH), and conducted in accordance with the Good Clinical Practice guidelines and the Declaration of Helsinki. All patients gave written informed consent before study-related procedures.
The primary study objective was to evaluate the safety, tolerability, and pharmacokinetics of linifanib in Japanese patients with solid tumors. The secondary objective was to obtain a preliminary assessment of antitumor activity. An exploratory analysis was conducted to identify potential biomarkers that could predict linifanib activity or serve as surrogates for clinic endpoints in future linifanib studies.
A standard 3 + 3 design determined the dose level assignment. Patients were assigned to one of four sequential dose cohorts of once-a-day dose regimen of oral linifanib: 0.05, 0.10, 0.20, or 0.25 mg/kg, administered in the morning. The 0.25 mg/kg dose was the highest dose planned in order to establish a uniform global phase 2 dose, since a prior phase 1 study in non-Japanese resulted in a recommended phase 2 dose of 0.25 mg/kg [14]. Dose-limiting toxicity (DLT) was defined as Grade 4 neutropenia lasting >7 days, Grade 4 thrombocytopenia or decreased hemoglobin, Grade 3 or greater thrombocytopenia (if blood transfusion was required), febrile neutropenia, non-hematological toxicity except for manageable nausea, vomiting, anorexia, diarrhea, constipation or electrolyte abnormality, or a toxicity that required suspension of study drug for >7 days.
Patients self-administered linifanib once daily, on a 21-day cycle after fasting, and treatment continued until disease progression or intolerable toxicity. Patients were discontinued from study participation if they exhibited disease progression, had linifanib-related toxicities requiring >2 weeks of dose interruption, or required alternate antineoplastic therapy. The initial oral dose, 2.5–25.0 mg in increments of 2.5 mg, was determined by the patients’ weights. At each dose reduction, the linifanib dose was generally decreased by 2.5 mg. The dose was reduced by 5.0 mg for patients ≥86 kg in the 0.10 mg/kg cohort, for patients in the 0.20 mg/kg cohort who were ≥81 kg at the first reduction and 61–80 and ≥96 kg at the 2nd reduction, and for patients in the 0.25 mg/kg cohort who were ≥66 kg at the first reduction and ≥86 kg at the second reduction. Patients were discontinued if they required dose reduction, specified by cohort: Any reduction (0.05 mg/kg cohort); >1 reduction (0.10 mg/kg cohort, and patients ≤31 kg in the 0.20 mg/kg cohort with an initial 5 mg dose); >2 reductions (0.25 mg/kg cohort, and patients ≥32 kg in the 0.20 mg/kg cohort with an initial ≥7.5 mg dose).
Tumor response and safety
Baseline evaluations included physical examination, body weight, vital signs, 12-lead electrocardiogram, ECOG PS assessment, pregnancy test, laboratory tests, and multiple-gated acquisition scan/echocardiogram. Tumor response and/or disease progression was assessed by computerized tomography (CT) scan or magnetic resonance imaging (MRI) per RECIST [20] at screening and on Day (D) 1 of every second cycle prior to the subsequent treatment period, until tumor progression or until final visit. Complete response and partial response (PR) were defined according to RECIST [20]; objective response rate (ORR) was defined as the proportion of patients with best response of PR or CR among the study population. Safety assessments included laboratory test results and adverse events (AEs), which were graded according to CTCAE v3 [18] and coded by medical dictionary of regulatory activities (MedDRA) 1.0.
Pharmacokinetic and pharmacodynamic assessments
Pharmacokinetic sampling occurred pre-dose and 0.5, 1, 2, 3, 4, 6, 8, and 24 h after single-dose linifanib on Cycle (C) 1D1, and pre-dose and 0.5, 1, 2, 3, 4, 6, and 8 h after multiple once-daily doses on C1D15. Urine was collected for 24-h after the C1D15 dose. Linifanib and its metabolite concentrations in plasma and urine were determined using a validated method based on triple quadruple tandem mass spectrometry with a lower limit of quantification of 1.0 ng/mL.
Pharmacokinetic parameter (defined in Table 3) concentrations were determined by non-compartmental analysis using WinNonlin Professional v.5.2 (Pharsight Corp., Cary, NC). Dose proportionality was evaluated by linear regression analysis for dose-normalized (DN) maximum observed plasma concentration (C max) and DN area under the plasma concentration–time curve 0–24 h (AUC24) on C1D1, and DN C max and DN AUC24 on C1D15 across doses 0.05, 0.1, 0.2, and 0.25 mg/kg. Additional samples were collected at C3D1 (pre-dose) and every second cycle until study completion or until C15D1. Concentrations for samples at C3D1 and subsequent samples, and data from C1D1 to C1D15 were included in the nonlinear mixed effects models to explore covariates such as age, body weight, and gender (data not shown). Following single-dose linifanib at 0.25 mg/kg, a post hoc analysis compared the pharmacokinetics between the Japanese patients in the current study and non-Japanese patients in two phase 1 studies: Caucasian patients receiving 0.25 mg linifanib (Abbott, unpublished) and the non-Japanese segment of Asian patients receiving 0.10–0.30 mg/kg linifanib [14].
Plasma for biomarker analysis was collected before linifanib administration on C1D1, C1D15, C2D1, and at the final visit. Concentration of PlGF was determined using Abbott Architect® kits. The relationship of PlGF levels to outcomes was assessed post hoc. To assess the relationship between PlGF induction and toxicity, patients were grouped into those requiring and not requiring dose interruption during the first 30 days of therapy. Median PlGF increase from baseline to C1D15 was compared as a function of toxicity group. To assess the relationship between PlGF induction and efficacy, patients were segregated into those with progressive disease (PD; N = 6) or stable disease (SD; N = 10) at C6, and PlGF increase from baseline to C1D15 was compared.
Statistical analysis
Continuous variables from clinical data were summarized by the number of observations, mean, standard deviation, median, minimum, and maximum. Discrete variables were summarized by frequency and proportion. Statistical significance for clinical and pharmacodynamic analyses was determined by a 2-sided P value <0.05.
Results
Patient characteristics
From September 2008 to September 2009, 18 patients with various solid tumor types were enrolled at the NCCH in Japan. Initial linifanib doses in each patient were 0.05 mg/kg (n = 3), 0.10 mg/kg (n = 6), 0.20 mg/kg (n = 3), and 0.25 mg/kg (n = 6). Patient baseline and disease characteristics were well balanced across the dose groups (Table 1). The majority were women, had ECOG PS of 0, and had received three or more prior systemic therapies (Table 1). Median (range) treatment duration was 147 days (7–672+). Median (range) dose intensity, defined as the percent of full-dose daily linifanib received from C1D1 to treatment discontinuation, was 91% (33–100).
Safety and tolerability
The most common linifanib-related AEs were hypertension, increased aspartate aminotransferase (AST), rash, neutropenia, and increased blood triglycerides (Table 2). There were no Grade 3 linifanib-related AEs at the 0.05 mg/kg dose, three at 0.10 mg/kg, two at 0.20 mg/kg, and four at 0.25 mg/kg. Grade 3 linifanib-related AEs included proteinuria (n = 4), neutropenia (n = 2), increased alanine aminotransferase (ALT) (n = 2), diarrhea, increased blood magnesium, decreased lymphocyte count, and hypertension. There were no Grade 4 or 5 AEs. Two DLTs were reported. One patient (0.10 mg/kg cohort) had a Grade 3 ALT increase, and one (0.25 mg/kg cohort) had a Grade 1 T-wave inversion requiring dose interruption for >7 days and discontinuation on D29.
Adverse events leading to dose reductions were palmar-plantar erythrodysaesthesia (n = 2), abdominal pain, abdominal pain upper, diarrhea, gastritis, increased ALT, and decreased platelet count. Adverse events leading to dose interruptions in two or more patients were palmar-plantar erythrodysaesthesia (n = 4), decreased platelet count (n = 3), abdominal pain upper (n = 3), diarrhea (n = 2), fatigue (n = 2), increased ALT (n = 2), and proteinuria (n = 2). There were no dose reductions or interruptions for hypertension, neutropenia, or leucopenia. Of 16 patients who discontinued the study, 12 discontinued due to PD, one due to PD and AE, two due to AEs, and one due to an AE and withdrawal of consent.
Pharmacokinetics
Pharmacokinetic data were available for 18 and 16 patients on C1D1 and C1D15, respectively. Table 3 shows the pharmacokinetic parameters following linifanib single dose or multiple daily doses. Linifanib was rapidly absorbed, with average T max approximately 2 h across all dose levels. Patients receiving the lowest dose had slightly higher DN exposures over 24-h post-administration (DN AUC24). Comparison of DN pharmacokinetic data across the 0.10, 0.20, and 0.25 mg/kg cohorts revealed no significant trend with dose level in peak serum concentration (DN C max) or DN AUC24 on C1D1 or C1D15 (P > 0.05). The DN AUC24 on C1D15 was approximately 1.5-fold of the DN AUC24 on C1D1 for each dose level (accumulation ratio approximately 1.5). The effective half-life of linifanib after repeated daily dosing associated with this value is 15 h (Table 3). Of 13 patients with available urine data, <15% of the dose was recovered as unchanged drug and metabolite across doses. Post hoc analysis showed that the pharmacokinetics for the Japanese patients following a single dose in the current study were similar to those of non-Japanese subjects in historical linifanib studies (Table 4).
Efficacy
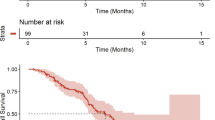
Two patients had confirmed PRs. One of these had breast cancer and received treatment in the 0.20 mg/kg cohort for 147 days. The other had lung cancer and received treatment in the 0.25 mg/kg cohort for 131 days. Figure 1 shows representative CT scans for these two patients. The ORR was 2 of 18 patients, 11.1%. Twelve patients had SD. Of these, 11 had SD for ≥12 weeks, including patients with lung cancer, breast cancer, sarcoma, thymic cancer, and colon cancer. Tumor response was not evaluable in four patients; one had tumors that were not measurable at baseline, one had tumors that were not measurable after treatment, and two had early discontinuation due to AEs or clinical deterioration. Median (range) progression-free survival (PFS) was 5.7 months (2.8–9.8). Median (range) duration of response was 3.2 months (2.8–3.5). The best tumor response at imaging assessments for each patient is illustrated in Fig. 2. A reduction in summed tumor dimensions of ≥5% was seen in 12 of the 18 patients on study and in cohorts 0.10, 0.20, and 0.25 mg/kg.
CT images for two patients with confirmed partial responses following linifanib treatment. a A 39-year-old female patient with lung cancer who received prior chemotherapy had lesions in the lung, pleura, and lymph nodes. This patient had a confirmed PR in C4, following linifanib treatment at 0.25 mg/kg. Arrows indicate tumor location at screening and at C5D1. b A 42-year-old female patient with breast cancer who received prior chemotherapy had target lesions in the mediastinal lymph nodes. This patient had a confirmed PR in C2, following linifanib treatment at 0.20 mg/kg. Arrows indicate tumor location at screening and at C6D21. Abbreviations: CT computerized tomography; PR partial response; C cycle; D day
Four patients continued linifanib with clinical benefit for ≥48 weeks (range, 48–96+ weeks). These patients had sarcoma, breast cancer, lung cancer, and thymic cancer. All had a best tumor response of SD. A post hoc analysis showed that pharmacokinetic parameter values and PlGF levels for these four patients were not notably different from the levels for the other patients in the study (data not shown).
Pharmacodynamics
Induction of PlGF was observed on C1D15 and C2D1 upon treatment with linifanib at a dose-dependent fashion. Concentration of PlGF returned to near baseline levels at the final visit when patients were no longer on therapy, indicating PlGF increase is reversible (Fig. 3a).
To explore relationships between PlGF induction and toxicity, PlGF changes from baseline to C1D15 were compared in patients who required a dose interruption during the first 30 days of therapy and those who did not. The median (±SD) increase from baseline to C1D15 PlGF was 22.8 pg/mL (±16.2) for the five patients who did not need a dose interruption and was 79.9 (±55.0) for the 11 patients who did (Fig. 3b). Taken together, these data indicate PlGF induction is dose-dependent. To examine a relationship between PlGF induction and efficacy, patients were segregated into those with PD (n = 6) or SD (n = 10) at C6. No statistically significant difference in PlGF change from baseline to C1D15 as a function of response classification (p = 0.7) was observed.
Discussion
The results of this phase 1 study showed that linifanib had a favorable safety profile in this Japanese population. Patients had minimal DLTs (two) and no Grade 4 AEs. Toxicities were mild to moderate and were manageable. The most frequently observed toxicity was hypertension, which occurred in 17 of the 18 patients across all dose groups. All events of hypertension were Grade 1 or 2, except for one instance of Grade 3 (0.20 mg/kg dose). Although other phase 1 TKI studies in Japanese patient populations have reported Grade 3 hypertension as an adverse event [21–23], a direct comparison with the current study is difficult due to the small number of patients in the other studies, and differences to the current study in their dose escalation designs. In the phase 1 linifanib study in non-Japanese Asian patients [14], Grade 3 hypertension was observed in 8% of patients at the recommended phase 2 dose, and in other, mixed-population, TKI phase 1 studies, including cediranib [24], motesanib [25], and brivanib [26], Grade 3 hypertension was observed in 14–20% of patients at the phase 2 recommended dose levels. The most common linifanib-related AEs in the present study (hypertension, rash, neutropenia, proteinuria, weight decreased, leukopenia, fatigue, palmar-plantar erythrodysaesthesia) as well as linifanib-related Grade 3 AEs (proteinuria, diarrhea, neutropenia, increased ALT, and increased blood magnesium) were comparable to the most common drug-related AEs in other phase 1, dose-escalating studies in multi-targeted TKIs [14, 21–32]. The phase 1 linifanib trial in Asian patients showed that linifanib-related toxicities increased in frequency and intensity with increasing doses, hypertension was dose-dependent, patients responded to antihypertensive therapy, and proteinuria and skin blisters resolved after reduction or stopping linifanib dosing. In the present study, dose interruption or reduction was seen for Grade 2 palmar-plantar erythrodysaesthesia and Grade 3 proteinuria; however, a relationship between the linifanib dose level and AE incidence could not be established due to the small number of patients in each dose group.
The 18 Japanese patients in this study received oral linifanib daily at escalating doses of 0.05, 0.10, 0.20, and 0.25 mg/kg. Linifanib was rapidly absorbed with an average T max of approximately 2 h across all dose levels. After 15 days of repeated daily dosing, linifanib accumulated 1.5-fold and the effective half-life was approximately 15 h. The urinary excretion of linifanib was a minor pathway following oral administration. Similar T max and half-life were seen in non-Japanese linifanib phase 1 studies [14, 33]. Daily doses ≥0.1 mg/kg used in the current study achieved the efficacious plasma exposures at steady state (≥2.7 μg h/mL) predicted based on a preclinical murine HT1080 fibrosarcoma model [10]. The pharmacokinetics following single-dose administration at 0.25 mg/kg from this Japanese study are similar to those from the non-Japanese phase 1 studies [14, 33]. Linifanib pharmacokinetics were dose-proportional over the 0.10–0.25 mg/kg single and once-daily dose range, also reported in the linifanib phase 1 dose-escalating trial in non-Japanese patients [14].
Circulating levels of PlGF, which increase with VEGFR inhibition, have the potential to act as a pharmacodynamic biomarker [34]. In a previous phase 1 linifanib study, PlGF increased dose-dependently [35]. This study confirmed the dose-dependent increase in PlGF following linifanib therapy and demonstrated that larger increases in PlGF concentrations were observed in patients requiring a dose reduction. In a post hoc analysis of the four patients on this study ≥48 weeks, PlGF was not notably different compared with the other study patients.
Conclusions regarding efficacy in phase 1 studies are necessarily limited. Although tumor evaluation was not the primary objective of this study, linifanib demonstrated encouraging preliminary antitumor activity across a range of tumor types (lung cancer, breast cancer, colon cancer, and others). Tumor reduction >5% by RECIST was observed in the majority of patients (12/18, 67%), and PRs were observed in two patients at the 0.20 mg/kg and 0.25 mg/kg dose levels. The four patients participating in the present study for ≥48 weeks have received 0.05 mg/kg, 0.10 mg/kg, or 0.20 mg/kg linifanib; three had a decrease in tumor size from baseline, and none had Grade 3 or 4 linifanib-related AEs. Substantial conclusions about clinical efficacy cannot be made due to the small size of the population. Preliminary antitumor activity was also demonstrated in a phase 1 trial of linifanib for solid tumors in Asian patients [14] and in three phase 2 trials of linifanib for solid tumors [15, 16, 36]. Similar, preliminary, antitumor efficacy has been seen in phase 1 studies of other TKIs [21–28, 30, 32].
In summary, linifanib was well tolerated in Japanese patients with solid tumors at the dose range 0.05–0.25 mg/kg. Linifanib pharmacokinetics were dose-proportional at the 0.10–0.25 mg/kg dose range following single and multiple once-daily oral administration. The pharmacokinetics of Japanese patients following single-dose administration at 0.25 mg/kg are similar to those seen in non-Japanese patients. Dose-dependent increases in PlGF were observed, but did not demonstrate a clear association with patient response to linifanib.
References
Dvorak HF (2002) Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J Clin Oncol 20:4368–4380
Carmeliet P (2003) Angiogenesis in health and disease. Nat Med 9:653–660
Benjamin LE, Golijanin D, Itin A, Pode D, Keshet E (1999) Selective ablation of immature blood vessels in established human tumors follows vascular endothelial growth factor withdrawal. J Clin Invest 103:159–165
Cook KM, Figg WD (2010) Angiogenesis inhibitors: current strategies and future prospects. CA Cancer J Clin 60:222–243
Feng X, Ofstad W, Hawkins D (2010) Antiangiogenesis therapy: a new strategy for cancer treatment. US Pharm 35:4–9
Perona R (2006) Cell signalling: growth factors and tyrosine kinase receptors. Clin Transl Oncol 8:77–82
Homsi J, Daud A (2007) Spectrum of activity and mechanism of action of VEGF/PDGF inhibitors. Cancer Control 14:285–294
Erber R, Thurnher A, Katsen A, Groth G, Kerger H, Hammes H, Menger M, Ullrich A, Vajkoczy P (2004) Combined inhibition of VEGF and PDGF signaling enforces tumor vessel regression by interfering with pericyte-mediated endothelial cell survival mechanisms. FASEB J 18:338–340
Dai Y, Hartandi K, Ji Z, Ahmed AA, Albert DH, Bauch JL, Bouska JJ, Bousquet PF, Cunha GA, Glaser KB, Harris CM, Hickman D, Guo J, Li J, Marcotte PA, Marsh KC, Moskey MD, Martin RL, Olson AM, Osterling DJ, Pease LJ, Soni NB, Stewart KD, Stoll VS, Tapang P, Reuter DR, Davidsen SK, Michaelides MR (2007) Discovery of N-(4-(3-amino-1H-indazol-4-yl)phenyl)-N’-(2-fluoro-5-methylphenyl)urea (ABT-869), a 3-aminoindazole-based orally active multitargeted receptor tyrosine kinase inhibitor. J Med Chem 50:1584–1597
Albert DH, Tapang P, Magoc TJ, Pease LJ, Reuter DR, Wei RQ, Li J, Guo J, Bousquet PF, Ghoreishi-Haack NS, Wang B, Bukofzer GT, Wang YC, Stavropoulos JA, Hartandi K, Niquette AL, Soni N, Johnson EF, McCall JO, Bouska JJ, Luo Y, Donawho CK, Dai Y, Marcotte PA, Glaser KB, Michaelides MR, Davidsen SK (2006) Preclinical activity of ABT-869, a multitargeted receptor tyrosine kinase inhibitor. Mol Cancer Ther 5:995–1006
Guo J, Marcotte PA, McCall JO, Dai Y, Pease LJ, Michaelides MR, Davidsen SK, Glaser KB (2006) Inhibition of phosphorylation of the colony-stimulating factor-1 receptor (c-Fms) tyrosine kinase in transfected cells by ABT-869 and other tyrosine kinase inhibitors. Mol Cancer Ther 5:1007–1013
Shankar DB, Li J, Tapang P, Owen McCall J, Pease LJ, Dai Y, Wei RQ, Albert DH, Bouska JJ, Osterling DJ, Guo J, Marcotte PA, Johnson EF, Soni N, Hartandi K, Michaelides MR, Davidsen SK, Priceman SJ, Chang JC, Rhodes K, Shah N, Moore TB, Sakamoto KM, Glaser KB (2007) ABT-869, a multitargeted receptor tyrosine kinase inhibitor: inhibition of FLT3 phosphorylation and signaling in acute myeloid leukemia. Blood 109:3400–3408
Zhou N, Moradei O, Raeppel S, Leit S, Frechette S, Gaudette F, Paquin I, Bernstein N, Bouchain G, Vaisburg A, Jin Z, Gillespie J, Wang J, Fournel M, Yan PT, Trachy-Bourget MC, Kalita A, Lu A, Rahil J, MacLeod AR, Li Z, Besterman JM, Delorme D (2008) Discovery of N-(2-aminophenyl)-4-[(4-pyridin-3-ylpyrimidin-2-ylamino)methyl]benzamide (MGCD0103), an orally active histone deacetylase inhibitor. J Med Chem 51:4072–4075
Wong C-I, Koh T-S, Soo R, Hartono S, Thng C-H, McKeegan E, Yong W-P, Chen C-S, Lee S-C, Wong J, Lim R, Sukri N, Lim S-E, Ong A-B, Steinberg J, Gupta N, Pradhan R, Humerickhouse R, Goh B-C (2009) Phase I and biomarker study of ABT-869, a multiple receptor tyrosine kinase inhibitor, in patients with refractory solid malignancies. J Clin Oncol 27:4718–4726
Tan E-H, Goss GD, Salgia R, Besse B, Gandara DR, Hanna NH, Yang JC-H, Thertulien R, Wertheim M, Mazieres J, Hensing T, Lee C, Gupta N, Pradhan R, Qian J, Qin Q, Scappaticci FA, Ricker JL, Carlson DM, Soo RA (2011) Phase 2 trial of linifanib (ABT-869) in patients with advanced non-small cell lung cancer. J Thor Oncol 6:1418–1425
Toh HC, Chen PJ, Carr B, Knox JJ, Gill S, Qian J, Qin Q, Ricker JL, Carlson DM, Yong WP (2010) Linifanib treatment in advanced hepatocellular carcinoma (HCC) patients: a phase 2 trial. Hepatology 52(Suppl 1):1166A (abstract 1777)
Tannir NM, Wong YN, Kollmannsberger CK, Ernstoff MS, Perry DJ, Appleman LJ, Posadas EM, Cho D, Choueiri TK, Coates A, Gupta N, Pradhan R, Qian J, Chen J, Scappaticci FA, Ricker JL, Carlson DM, Michaelson MD (2011) Phase 2 trial of linifanib (ABT-869) in patients with advanced renal cell cancer after sunitinib failure. Eur J Cancer 47:2706–2714
NCI (2006) Common terminology criteria for adverse events v3.0 (CTCAE). http://ctep.cancer.gov
National Institutes of Health: An open label, phase 1 study evaluating pharmacokinetics, safety and tolerability of ABT-869 in subjects with solid tumors. Protocol: (NCT00718380). http://clinicaltrials.gov/
Therasse P, Arbuck SG, Eisenhauer EA (2000) New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst 92:205–216
Fujisaka Y, Yamada Y, Yamamoto N, Shimizu T, Fujiwara Y, Yamada K, Tamura T, Watanabe H, Sun Y-N, Bass MB, Seki M (2010) Phase 1 study of the investigational, oral angiogenesis inhibitor motesanib in Japanese patients with advanced solid tumors. Cancer Chemother Pharmacol 66:935–943
Minami H, Kawada K, Ebi H, Kitagawa K, Kim Y-I, Araki K, Mukai H, Tahara M, Nakajima H, Nakajima K (2008) Phase I and pharmacokinetic study of sorafenib, an oral multikinase inhibitor, in Japanese patients with advanced refractory solid tumors. Cancer Sci 99:1492–1498
Mukohara T, Nakajima H, Mukai H, Nagai S, Itoh K, Umeyama Y, Hashimoto J, Minami H (2010) Effect of axitinib (AG-013736) on fatigue, thyroid-stimulating hormone, and biomarkers: a phase I study in Japanese patients. Cancer Sci 101:963–968
Drevs J, Siegert P, Medinger M, Mross K, Strecker R, Zirrgiebel U, Harder J, Blum H, Robertson J, Jürgensmeier JM, Puchalski TA, Young H, Saunders O, Unger C (2007) Phase I clinical study of AZD2171, an oral vascular endothelial growth factor signaling inhibitor, in patients with advanced solid tumors. J Clin Oncol 25:3045–3054
Rosen LS, Kurzrock R, Mulay M, Vugt AV, Purdom M, Ng C, Silverman J, Koutsoukos A, Sun Y-N, Bass MB, Xu RY, Polverino A, Wiezorek JS, Chang DD, Benjamin R, Herbst RS (2007) Safety, pharmacokinetics, and efficacy of AMG 706, an oral multikinase inhibitor, in patients with advanced solid tumors. J Clin Oncol 25:2369–2376
Jonker DJ, Rosen LS, Sawyer MB, de Braud F, Wilding G, Sweeney CJ, Jayson GC, McArthur GA, Rustin G, Goss G, Kantor J, Velasquez L, Syed S, Mokliatchouk O, Feltquate DM, Kollia G, Nuyten DSA, Galbraith S (2011) A phase I study to determine the safety, pharmacokinetics and pharmacodynamics of a dual VEGFR and FGFR inhibitor, brivanib, in patients with advanced or metastatic solid tumors. Annals Oncol 22:1413–1419
Strumberg D, Clark JW, Awada A, Moore MJ, Richly H, Hendlisz A, Hirte HW, Eder JP, Lenz H-J, Schwartz B (2007) Safety, pharmacokinetics, and preliminary antitumor activity of sorafenib: a review of four phase I trials in patients with advanced refractory solid tumors. Oncologist 12:426–437
Rugo HS, Herbst RS, Liu G, Park JW, Kies MS, Steinfeldt HM, Pithavala YK, Reich SD, Freddo JL, Wilding G (2005) Phase I trial of the oral antiangiogenesis agent AG-013736 in patients with advanced solid tumors: pharmacokinetic and clinical results. J Clin Oncol 23:5474–5483
Yamamoto N, Tamura T, Yamamoto N, Yamada K, Yamada Y, Nokihara H, Fujiwara Y, Takahashi T, Murakami H, Boku N, Yamazaki K, Puchalski T, Shin E (2009) Phase I, dose escalation and pharmacokinetic study of cediranib (RECENTIN™), a highly potent and selective VEGFR signaling inhibitor, in Japanese patients with advanced solid tumors. Cancer Chemother Pharmacol 64:1165–1172
Fiedler W, Giaccone G, Lasch P, van der Horst I, Brega N, Courtney R, Abbattista A, Shalinsky DR, Bokemeyer C, Boven E (2011) Phase I trial of SU14813 in patients with advanced solid malignancies. Annals Oncol 22:195–201
Holden SN, Eckhardt SG, Basser R, de Boer R, Rischin D, Green M, Rosenthal MA, Wheeler C, Barge A, Hurwitz HI (2005) Clinical evaluation of ZD6474, an orally active inhibitor of VEGF and EGF receptor signaling, in patients with solid, malignant tumors. Annals Oncol 16:1391–1397
Faivre S, Delbaldo C, Vera K, Robert C, Lozahic S, Lassau N, Bello C, Deprimo S, Brega N, Massimini G, Armand J-P, Scigalla P, Raymond E (2006) Safety, pharmacokinetic, and antitumor activity of SU11248, a novel oral multitarget tyrosine kinase inhibitor, in patients with cancer. J Clin Oncol 24:25–35
Gupta N, Yan Z, LoRusso P, Ricker J, Carlson D, Pradhan R (2009) Assessment of the effect of food on the oral bioavailability and assessment of diurnal variation in the pharmacokinetics of linifanib. Mol Cancer Ther 8; (abstract B53)
Jain RK, Duda DG, Willett CG, Sahani DV, Zhu AX, Loeffler JS, Batchelor TT, Sorensen AG (2009) Biomarkers of response and resistance to antiangiogenic therapy. Nat Rev Clin Oncol 6:327–338
Soo RA, McKeegan E, Chen CS, Thng CH, Koh TS, Laird D, Zhang K, Wong CI, Gupta N, Goh BC (2008) The effect of varying doses of ABT-869 on biomarkers of angiogenesis and their correlation with pharmacodynamic outcome J Clin Oncol 26(Suppl 20); (abstract 14535)
Posadas EM, Tannir NM, Wong Y, Ernstoff MS, Kollmannsberger CK, Qian J, Ansell PJ, McKeegan EM, McKee MD, Ricker JL, Carlson DM, Michaelson MD (2011) Phase II trial of linifanib in patients (pts) with advanced renal cell carcinoma (RCC): Analysis of pts receiving extended therapy. ASCO Meet Abstr 29:2543
Acknowledgments
The authors would like to thank Yutaka Yamamura and Masanao Akiyama, both of Abbott Japan, for their contributions to the scope, content revisions, and critical review of this manuscript; Susumu Matsuki, Abbott Japan, for contributions to data review and content revisions; and Jody Bennett, Abbott, USA, for writing and editorial assistance. This support was funded by Abbott. This work was supported by Abbott Laboratories, IL.
Conflicts of interest
A. Coates, Y-L. Chiu, X. Li, R. Pradhan, P. J. Ansell, E. M. McKeegan, M. D. McKee, and D. M. Carlson are Abbott employees. Y-L. Chiu, R. Pradhan, P. J. Ansell, E. M. McKeegan, M. D. McKee, and D. M. Carlson own Abbott stock. All other authors declared no conflicts of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
Trial Registration: ClinicalTrials.gov. Number, NCT00718380.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License (https://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Asahina, H., Tamura, Y., Nokihara, H. et al. An open-label, phase 1 study evaluating safety, tolerability, and pharmacokinetics of linifanib (ABT-869) in Japanese patients with solid tumors. Cancer Chemother Pharmacol 69, 1477–1486 (2012). https://doi.org/10.1007/s00280-012-1846-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-012-1846-6