Abstract
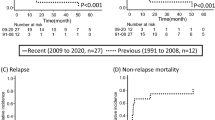
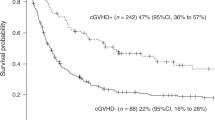
This study aimed to compare the effect of disease status at the time of allogeneic hematopoietic cell transplantation (HCT) on post-transplant outcomes between acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL). Japanese nationwide registry data for 6901 patients with AML and 2469 patients with ALL were analyzed. In this study, 2850 (41%), 937 (14%), 62 (1%), and 3052 (44%) AML patients and 1751 (71%), 265 (11%), 23 (1%), and 430 (17%) ALL patients underwent transplantation in first complete remission (CR1), second CR (CR2), third or subsequent CR (CR3 +), and non-CR, respectively. The probabilities of overall survival at 5 years for patients transplanted in CR1, CR2, CR3 + , and non-CR were 58%, 61%, 41%, and 26% for AML patients and 67%, 45%, 20%, and 21% for ALL patients, respectively. Multivariate analyses revealed that the risks of relapse and overall mortality were similar for AML patients transplanted in CR1 and CR2 (P = 0.672 and P = 0.703), whereas they were higher for ALL patients transplanted in CR2 than for those transplanted in CR1 (P < 0.001 for both). The risks of relapse and overall mortality for those transplanted in CR3 + and non-CR increased in a stepwise manner for both diseases, with the relevance being stronger for ALL than for AML patients. These results suggest a significant difference in the effect of disease status at HCT on post-transplant outcomes in AML and ALL. Further investigation to incorporate measurable residual disease data is warranted.


Similar content being viewed by others
References
Hahn T, McCarthy PL Jr, Hassebroek A, Bredeson C, Gajewski JL, Hale GA, Isola LM, Lazarus HM, Lee SJ, Lemaistre CF, Loberiza F, Maziarz RT, Rizzo JD, Joffe S, Parsons S, Majhail NS (2013) Significant improvement in survival after allogeneic hematopoietic cell transplantation during a period of significantly increased use, older recipient age, and use of unrelated donors. J Clin Oncol 31:2437–2449
Iida M, Kodera Y, Dodds A, Ho AYL, Nivison-Smith I, Akter MR, Wu T, Lie AKW, Ghavamzadeh A, Kang HJ, Ong TC, Gyi AA, Farzana T, Baylon H, Gooneratne L, Tang JL, Bunworasate U, Huynh VM, Srivastava A, Okamoto S, Atsuta Y, Registry Committee of the Asia-Pacific B, Marrow Transplantation G (2019) Advances in hematopoietic stem cell transplantation in the Asia-Pacific region: the second report from APBMT 2005-2015. Bone Marrow Transplant 54:1973-1986
Passweg JR, Baldomero H, Chabannon C, Basak GW, Corbacioglu S, Duarte R, Dolstra H, Lankester AC, Mohty M, Montoto S, Peffault de Latour R, Snowden JA, Styczynski J, Yakoub-Agha I, Kroger N, European Society for B, Marrow T (2020) The EBMT activity survey on hematopoietic-cell transplantation and cellular therapy 2018: CAR-T's come into focus. Bone Marrow Transplant 55:1604-1613
Atsuta Y (2016) Introduction of Transplant Registry Unified Management Program 2 (TRUMP2): scripts for TRUMP data analyses, part I (variables other than HLA-related data). Int J Hematol 103:3–10
Yanada M, Konuma T, Kuwatsuka Y, Kondo T, Kawata T, Takahashi S, Uchida N, Miyakoshi S, Tanaka M, Ozawa Y, Sawa M, Nakamae H, Aotsuka N, Kanda J, Takanashi M, Kanda Y, Atsuta Y, Yano S (2019) Unit selection for umbilical cord blood transplantation for adults with acute myeloid leukemia in complete remission: a Japanese experience. Bone Marrow Transplant 54:1789–1798
Yanada M, Mori J, Aoki J, Harada K, Mizuno S, Uchida N, Kurosawa S, Toya T, Kanamori H, Ozawa Y, Ogawa H, Henzan H, Iwato K, Sakura T, Ota S, Fukuda T, Ichinohe T, Atsuta Y, Yano S (2018) Effect of cytogenetic risk status on outcomes for patients with acute myeloid leukemia undergoing various types of allogeneic hematopoietic cell transplantation: an analysis of 7812 patients. Leuk Lymphoma 59:601–609
Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, Carbone PP (1982) Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol 5:649–655
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, Storer B (2005) Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood 106:2912–2919
Ibrahim JG, Chu H, Chen MH (2012) Missing data in clinical studies: issues and methods. J Clin Oncol 30:3297–3303
Cornelissen JJ, Gratwohl A, Schlenk RF, Sierra J, Bornhauser M, Juliusson G, Racil Z, Rowe JM, Russell N, Mohty M, Lowenberg B, Socie G, Niederwieser D, Ossenkoppele GJ (2012) The European LeukemiaNet AML Working Party consensus statement on allogeneic HSCT for patients with AML in remission: an integrated-risk adapted approach. Nat Rev Clin Oncol 9:579–590
Dohner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Buchner T, Dombret H, Ebert BL, Fenaux P, Larson RA, Levine RL, Lo-Coco F, Naoe T, Niederwieser D, Ossenkoppele GJ, Sanz M, Sierra J, Tallman MS, Tien HF, Wei AH, Lowenberg B, Bloomfield CD (2017) Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood 129:424–447
DeFilipp Z, Advani AS, Bachanova V, Cassaday RD, Deangelo DJ, Kebriaei P, Rowe JM, Seftel MD, Stock W, Tallman MS, Fanning S, Inamoto Y, Kansagra A, Johnston L, Nagler A, Sauter CS, Savani BN, Perales MA, Carpenter PA, Larson RA, Weisdorf D (2019) Hematopoietic cell transplantation in the treatment of adult acute lymphoblastic leukemia: updated 2019 evidence-based review from the American Society for Transplantation and Cellular Therapy. Biol Blood Marrow Transplant 25:2113–2123
Czyz A, Labopin M, Giebel S, Socie G, Apperley J, Volin L, Remenyi P, Yakoub-Agha I, Orchard K, Michallet M, Stuhler G, Chaganti S, Murray M, Aljurf M, Bloor A, Passweg J, Finke J, Mohty M, Nagler A (2018) Cyclophosphamide versus etoposide in combination with total body irradiation as conditioning regimen for adult patients with Ph-negative acute lymphoblastic leukemia undergoing allogeneic stem cell transplant: On behalf of the ALWP of the European Society for Blood and Marrow Transplantation. Am J Hematol 93:778–785
Pavlu J, Labopin M, Niittyvuopio R, Socie G, Yakoub-Agha I, Wu D, Remenyi P, Passweg J, Beelen DW, Aljurf M, Kroger N, Labussiere-Wallet H, Peric Z, Giebel S, Nagler A, Mohty M (2019) Measurable residual disease at myeloablative allogeneic transplantation in adults with acute lymphoblastic leukemia: a retrospective registry study on 2780 patients from the acute leukemia working party of the EBMT. J Hematol Oncol 12:108
Nagler A, Labopin M, Houhou M, Aljurf M, Mousavi A, Hamladji RM, Al Zahrani M, Bondarenko S, Arat M, Angelucci E, Koc Y, Gulbas Z, Sica S, Bourhis JH, Canaani J, Brissot E, Giebel S, Mohty M (2021) Outcome of haploidentical versus matched sibling donors in hematopoietic stem cell transplantation for adult patients with acute lymphoblastic leukemia: a study from the Acute Leukemia Working Party of the European Society for Blood and Marrow Transplantation. J Hematol Oncol 14:53
Lazaryan A, Dolan M, Zhang MJ, Wang HL, Kharfan-Dabaja MA, Marks DI, Bejanyan N, Copelan E, Majhail NS, Waller EK, Chao N, Prestidge T, Nishihori T, Kebriaei P, Inamoto Y, Hamilton B, Hashmi SK, Kamble RT, Bacher U, Hildebrandt GC, Stiff PJ, McGuirk J, Aldoss I, Beitinjaneh AM, Muffly L, Vij R, Olsson RF, Byrne M, Schultz KR, Aljurf M, Seftel M, Savoie ML, Savani BN, Verdonck LF, Cairo MS, Hossain N, Bhatt VR, Frangoul HA, Abdel-Azim H, Malki MA, Munker R, Rizzieri D, Khera N, Nakamura R, Ringden O, van der Poel M, Murthy HS, Liu H, Mori S, De Oliveira S, Bolanos-Meade J, Elsawy M, Barba P, Nathan S, George B, Pawarode A, Grunwald M, Agrawal V, Wang Y, Assal A, Caro PC, Kuwatsuka Y, Seo S, Ustun C, Politikos I, Lazarus HM, Saber W, Sandmaier BM, De Lima M, Litzow M, Bachanova V, Weisdorf D, Acute Leukemia Committee of the C (2020) Impact of cytogenetic abnormalities on outcomes of adult Philadelphia-negative acute lymphoblastic leukemia after allogeneic hematopoietic stem cell transplantation: a study by the Acute Leukemia Working Committee of the Center for International Blood and Marrow Transplant Research. Haematologica 105:1329-1338
Tekgunduz E, Kaynar L, Goker H, Kaya AH, Turak EE, Eliacik E, Kayikci O, Cetin M, Buyukasik Y, Eser B, Altuntas F (2016) Retrospective analysis of adult patients with acute lymphoblastic leukemia undergoing allogeneic hematopoietic cell transplantation: A multicenter experience of daily practice. Transfus Apher Sci 54:41–47
Eom KS, Shin SH, Yoon JH, Yahng SA, Lee SE, Cho BS, Kim YJ, Kim HJ, Min CK, Kim DW, Lee JW, Min WS, Park CW, Lee S (2013) Comparable long-term outcomes after reduced-intensity conditioning versus myeloablative conditioning allogeneic stem cell transplantation for adult high-risk acute lymphoblastic leukemia in complete remission. Am J Hematol 88:634–641
Kantarjian HM, DeAngelo DJ, Stelljes M, Martinelli G, Liedtke M, Stock W, Gokbuget N, O’Brien S, Wang K, Wang T, Paccagnella ML, Sleight B, Vandendries E, Advani AS (2016) Inotuzumab Ozogamicin versus Standard Therapy for Acute Lymphoblastic Leukemia. N Engl J Med 375:740–753
Kantarjian H, Stein A, Gokbuget N, Fielding AK, Schuh AC, Ribera JM, Wei A, Dombret H, Foa R, Bassan R, Arslan O, Sanz MA, Bergeron J, Demirkan F, Lech-Maranda E, Rambaldi A, Thomas X, Horst HA, Bruggemann M, Klapper W, Wood BL, Fleishman A, Nagorsen D, Holland C, Zimmerman Z, Topp MS (2017) Blinatumomab versus chemotherapy for advanced acute lymphoblastic leukemia. N Engl J Med 376:836–847
Mohty M, Labopin M, Volin L, Gratwohl A, Socie G, Esteve J, Tabrizi R, Nagler A, Rocha V, Acute Leukemia Working Party of E (2010) Reduced-intensity versus conventional myeloablative conditioning allogeneic stem cell transplantation for patients with acute lymphoblastic leukemia: a retrospective study from the European Group for Blood and Marrow Transplantation. Blood 116:4439-4443
Marks DI, Wang T, Perez WS, Antin JH, Copelan E, Gale RP, George B, Gupta V, Halter J, Khoury HJ, Klumpp TR, Lazarus HM, Lewis VA, McCarthy P, Rizzieri DA, Sabloff M, Szer J, Tallman MS, Weisdorf DJ (2010) The outcome of full-intensity and reduced-intensity conditioning matched sibling or unrelated donor transplantation in adults with Philadelphia chromosome-negative acute lymphoblastic leukemia in first and second complete remission. Blood 116:366–374
Araki D, Wood BL, Othus M, Radich JP, Halpern AB, Zhou Y, Mielcarek M, Estey EH, Appelbaum FR, Walter RB (2016) Allogeneic hematopoietic cell transplantation for acute myeloid leukemia: time to move toward a minimal residual disease-based definition of complete remission? J Clin Oncol 34:329–336
Oran B, Jorgensen JL, Marin D, Wang S, Ahmed S, Alousi AM, Andersson BS, Bashir Q, Bassett R, Lyons G, Chen J, Rezvani K, Popat U, Kebriaei P, Patel K, Rondon G, Shpall EJ, Champlin RE (2017) Pre-transplantation minimal residual disease with cytogenetic and molecular diagnostic features improves risk stratification in acute myeloid leukemia. Haematologica 102:110–117
Dillon R, Hills R, Freeman S, Potter N, Jovanovic J, Ivey A, Kanda AS, Runglall M, Foot N, Valganon M, Khwaja A, Cavenagh J, Smith M, Ommen HB, Overgaard UM, Dennis M, Knapper S, Kaur H, Taussig D, Mehta P, Raj K, Novitzky-Basso I, Nikolousis E, Danby R, Krishnamurthy P, Hill K, Finnegan D, Alimam S, Hurst E, Johnson P, Khan A, Salim R, Craddock C, Spearing R, Gilkes A, Gale R, Burnett A, Russell NH, Grimwade D (2020) Molecular MRD status and outcome after transplantation in NPM1-mutated AML. Blood 135:680–688
Sanchez-Garcia J, Serrano J, Serrano-Lopez J, Gomez-Garcia P, Martinez F, Garcia-Castellano JM, Rojas R, Martin C, Rodriguez-Villa A, Molina-Hurtado JR, Alvarez MA, Casano J, Torres-Gomez A (2013) Quantification of minimal residual disease levels by flow cytometry at time of transplant predicts outcome after myeloablative allogeneic transplantation in ALL. Bone Marrow Transplant 48:396–402
Nishiwaki S, Imai K, Mizuta S, Kanamori H, Ohashi K, Fukuda T, Onishi Y, Takahashi S, Uchida N, Eto T, Nakamae H, Yujiri T, Mori S, Nagamura-Inoue T, Suzuki R, Atsuta Y, Tanaka J (2016) Impact of MRD and TKI on allogeneic hematopoietic cell transplantation for Ph+ALL: a study from the adult ALL WG of the JSHCT. Bone Marrow Transplant 51:43–50
Stone RM, Mandrekar SJ, Sanford BL, Laumann K, Geyer S, Bloomfield CD, Thiede C, Prior TW, Dohner K, Marcucci G, Lo-Coco F, Klisovic RB, Wei A, Sierra J, Sanz MA, Brandwein JM, de Witte T, Niederwieser D, Appelbaum FR, Medeiros BC, Tallman MS, Krauter J, Schlenk RF, Ganser A, Serve H, Ehninger G, Amadori S, Larson RA, Dohner H (2017) Midostaurin plus chemotherapy for acute myeloid leukemia with a FLT3 mutation. N Engl J Med 377:454–464
Cortes J, Perl AE, Dohner H, Kantarjian H, Martinelli G, Kovacsovics T, Rousselot P, Steffen B, Dombret H, Estey E, Strickland S, Altman JK, Baldus CD, Burnett A, Kramer A, Russell N, Shah NP, Smith CC, Wang ES, Ifrah N, Gammon G, Trone D, Lazzaretto D, Levis M (2018) Quizartinib, an FLT3 inhibitor, as monotherapy in patients with relapsed or refractory acute myeloid leukaemia: an open-label, multicentre, single-arm, phase 2 trial. Lancet Oncol 19:889–903
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, Montesinos P, Baer MR, Larson RA, Ustun C, Fabbiano F, Erba HP, Di Stasi A, Stuart R, Olin R, Kasner M, Ciceri F, Chou WC, Podoltsev N, Recher C, Yokoyama H, Hosono N, Yoon SS, Lee JH, Pardee T, Fathi AT, Liu C, Hasabou N, Liu X, Bahceci E, Levis MJ (2019) Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med 381:1728–1740
Stein EM, DiNardo CD, Pollyea DA, Fathi AT, Roboz GJ, Altman JK, Stone RM, DeAngelo DJ, Levine RL, Flinn IW, Kantarjian HM, Collins R, Patel MR, Frankel AE, Stein A, Sekeres MA, Swords RT, Medeiros BC, Willekens C, Vyas P, Tosolini A, Xu Q, Knight RD, Yen KE, Agresta S, de Botton S, Tallman MS (2017) Enasidenib in mutant IDH2 relapsed or refractory acute myeloid leukemia. Blood 130:722–731
DiNardo CD, Stein EM, de Botton S, Roboz GJ, Altman JK, Mims AS, Swords R, Collins RH, Mannis GN, Pollyea DA, Donnellan W, Fathi AT, Pigneux A, Erba HP, Prince GT, Stein AS, Uy GL, Foran JM, Traer E, Stuart RK, Arellano ML, Slack JL, Sekeres MA, Willekens C, Choe S, Wang H, Zhang V, Yen KE, Kapsalis SM, Yang H, Dai D, Fan B, Goldwasser M, Liu H, Agresta S, Wu B, Attar EC, Tallman MS, Stone RM, Kantarjian HM (2018) Durable remissions with ivosidenib in IDH1-mutated relapsed or refractory AML. N Engl J Med 378:2386–2398
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, Konopleva M, Döhner H, Letai A, Fenaux P, Koller E, Havelange V, Leber B, Esteve J, Wang J, Pejsa V, Hájek R, Porkka K, Illés Á, Lavie D, Lemoli RM, Yamamoto K, Yoon SS, Jang JH, Yeh SP, Turgut M, Hong WJ, Zhou Y, Potluri J, Pratz KW (2020) Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med 383:617–629
Wei AH, Montesinos P, Ivanov V, DiNardo CD, Novak J, Laribi K, Kim I, Stevens DA, Fiedler W, Pagoni M, Samoilova O, Hu Y, Anagnostopoulos A, Bergeron J, Hou JZ, Murthy V, Yamauchi T, McDonald A, Chyla B, Gopalakrishnan S, Jiang Q, Mendes W, Hayslip J, Panayiotidis P (2020) Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood 135:2137–2145
Maude SL, Laetsch TW, Buechner J, Rives S, Boyer M, Bittencourt H, Bader P, Verneris MR, Stefanski HE, Myers GD, Qayed M, De Moerloose B, Hiramatsu H, Schlis K, Davis KL, Martin PL, Nemecek ER, Yanik GA, Peters C, Baruchel A, Boissel N, Mechinaud F, Balduzzi A, Krueger J, June CH, Levine BL, Wood P, Taran T, Leung M, Mueller KT, Zhang Y, Sen K, Lebwohl D, Pulsipher MA, Grupp SA (2018) Tisagenlecleucel in children and young adults with B-cell lymphoblastic leukemia. N Engl J Med 378:439–448
Funding
This work was supported in part by a grant from the Practical Research Project for Allergic Diseases and Immunology (Research Technology of Medical Transplantation) from the Japan Agency for Medical Research and Development (AMED), grant number: 19ek0510023h0002, and a grant from the Aichi Cancer Research Foundation, grant number: 2021–1-9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the institutional review board of the Aichi Cancer Center, and was conducted in accordance with the Declaration of Helsinki. Informed consent was obtained from each patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Yanada, M., Konuma, T., Yamasaki, S. et al. The differential effect of disease status at allogeneic hematopoietic cell transplantation on outcomes in acute myeloid and lymphoblastic leukemia. Ann Hematol 100, 3017–3027 (2021). https://doi.org/10.1007/s00277-021-04661-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-021-04661-2