Abstract
Purpose
Evaluation of dual-layer spectral computed tomography (CT) for contrast enhancement during image-guided biopsy of liver lesions using virtual monoenergetic images (VMI) and virtual non-contrast (VNC) images.
Methods
Spectral CT data of 20 patients receiving CT-guided needle biopsy of focal liver lesions were used to generate VMI at energy levels from 40 to 200 keV and VNC images. Images were analyzed objectively regarding contrast-to-noise ratio between lesion center (CNRcent) or periphery (CNRperi) and normal liver parenchyma. Lesion visibility and image quality were evaluated on a 4-point Likert scale by two radiologists.
Results
Using VMI/VNC images, readers reported an increased visibility of the lesion compared to the conventional CT images in 18/20 cases. In 75% of cases, the highest visibility was derived by VMI-40. Showing all reconstructions simultaneously, VMI-40 offered the highest visibility in 75% of cases, followed by VNC in 12.5% of cases. Either CNRcent (17/20) or/and CNRperi (17/20) was higher (CNR increase > 50%) in 19/20 cases for VMI-40 or VNC images compared to conventional CT images. VMI-40 showed the highest CNRcent in 14 cases and the highest CNRperi in 12 cases. High image quality was present for all reconstructions with a minimum median of 3.5 for VMI-40 and VMI-50.
Conclusions
When implemented in the CT scanner software, automated contrast enhancement of liver lesions during image-guided biopsy may facilitate the procedure.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In clinical practice, focal liver lesions are a common finding. In most cases, diagnostic imaging enables the differentiation between benign and malignant focal liver lesions [1, 2]. However, if lesions show atypical features or growth, biopsy may be warranted to perform histological analysis [3]. Biopsies are commonly performed using either ultrasound guidance or computed tomography (CT) imaging. Although ultrasound is the preferred imaging modality for liver biopsy, there are limitations [4]. In comparison, CT images provide a better overview, and the biopsy needle is clearly visible due to its high density [5]. Intravenous contrast is often needed for the detection of liver lesions. However, the visualization of focal liver lesions provided by intravenous contrast can be short-lived due to an increasing equilibrium of the lesion and the liver parenchyma [5]. In these cases, it would be helpful to prolong and enhance the contrast between the lesion and the normal liver tissue to facilitate the biopsy procedure. In recent years, dual-energy CT (DE-CT) has demonstrated that the derived spectral information can improve the detectability of focal liver lesions. DE-CT uses the absorption characteristics for the differentiation and quantification of materials while conventional CT only quantifies the attenuation of the total X-ray spectrum reaching the detector [6]. In dual-layer detector CT (DL-CT), the spectral separation occurs at the detector level offering several advantages compared to source-based approaches [7]. For DL-CT, spectral data are acquired additionally to the conventional images with every scan and retrospective reconstruction of spectral information is possible [8]. Using these spectral data, iodine can be quantified accurately [9]. Virtual non-contrast (VNC) images can be created via detection and quantification of iodine, which is then subtracted, resulting in a calculated unenhanced image without iodine [10, 11]. Furthermore, virtual monoenergetic images (VMIs) can be calculated, simulating monoenergetic X-ray source during the acquisition of the CT scan [7], boosting the iodine signal at low voltages and decreasing it at high voltages [12].
The objective of our retrospective study was to evaluate the potential benefit of VMI and VNC to prolong and improve lesion detectability during liver biopsy following a contrast-enhanced planning CT scan.
Materials and Methods
Patient Population
Institutional review board approval was obtained for this retrospective study. Informed consent was waived by the institutional review board as no additional data besides clinical obtained images were used. All examinations were performed exclusively for clinical use. Patients were referred for biopsy by other departments of the hospital.
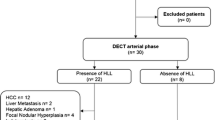
Twenty consecutive patients who were examined with a DL-CT and received a triphasic CT before biopsy were retrospectively included in the current study. Median patient age was 63.9 (36.1–84.7) years, with 13 males and 7 females. A core needle biopsy of a hepatic lesion was performed in all patients. The images obtained during the biopsies were analyzed retrospectively. Biopsies were performed with conventional CT images. Biopsy outcomes are shown in Table 1.
Image Acquisition
All examinations were performed using a DL-CT (IQon; Philips Healthcare). Patients underwent a triphasic CT scan of the abdomen that included a non-enhanced scan, an arterial phase and a venous phase (75 s after contrast injection) at 120 kVp and 64 × 0.625 mm detector configuration. An adjustment of the tube current based on the scout view (z-axis modulation) is included by default. Iodinated contrast media was injected for the arterial phase (1.2 ml/kg with a maximum of 120 ml) followed by a 50-ml saline chaser. After the triphasic CT scan, the core needle biopsy was planned based on the acquired data. The scanner couch was centered in the chosen position, the image acquisition during the biopsy included three slices (head-mid-foot) with a slice thickness of 3 mm. Following the biopsy, a delayed phase without intravenous contrast was performed to rule out hemorrhage. If a substantial hemorrhage was seen, additional scans with intravenous contrast would have been added, however, this was not the case in the study population. All data sets were reconstructed in axial view with slice thickness of 3 mm and a 512 × 512 image matrix.
For each phase as well as for the images during biopsy, spectral data were acquired. Using these data, virtual monoenergetic images (VMIs) at tube currents of 40–200 keV with steps of 10 keV (VMI40–VMI200) as well as virtual non-contrast images (VNC) were calculated using the commercially available spectral workstation (IntelliSpace Portal (v. 8.0.2), Philips Healthcare). Additionally, conventional images (CIs), which are used in clinical routine, were saved. Hereby, CIs are the images of the respective phase, which are acquired without using image modification via spectral information.
Objective Image Analysis
For each patient, one hepatic lesion was chosen for biopsy. This lesion was analyzed in all phases (unenhanced, arterial, venous and delayed) as well as in the biopsy images. Regions of interests (ROIs) were defined in the center of the lesion, in the periphery of the lesion as well as in normal hepatic parenchyma. Hereby, the ROIs were drawn as large as possible. For every ROI, the mean Hounsfield units (HU) and the corresponding standard deviation (SD) were measured. For the center and the periphery of each measured lesion, the contrast-to-noise ratio (CNR) were calculated using the formula:
CNR = (HUlesion-HUliver)/SDliver.
where HUlesion is the HU-value of the lesion (center or periphery), HUliver is the HU-value of the normal liver parenchyma and SDliver is the standard deviation in the normal liver parenchyma, representing noise.
Reader Study
To evaluate the subjective image quality as well as the visibility of the focal lesion, two radiologists with 3 and 7 years of experience in CT-guided interventions were asked to analyze the biopsy images in all reconstructions (VMI40-VMI200, VNC, CI). Readers were allowed to change window leveling at their preference to prevent an influence of a predefined window level.
First, each reconstruction was shown separately. Here, the subjective image quality (1-very low; 2-poor; 3-good; 4-very good) and the visibility of the focal lesion (1-not visible; 2-poor; 3-good; 4-very good) were rated on a 4-point Likert scale.
Afterward, all reconstructions were shown simultaneously, and the readers were asked to rate the top 3 reconstructions enabling the best visibility of the focal lesion. Here, the total number of ratings is shown, so a maximum of 120 ratings (20 cases, 2 readers, 3 ratings per reader and case) are possible. Thus, 40 ratings were given for top-1, top-2 and top-3, respectively.
Statistical Analysis
Statistical analysis was performed by dedicated software packages (SPSS, IBM; Excel 2016, Microsoft). CNR is given in mean ± (SD), these data were tested for Gaussian distributions via D'Agostino-Pearson omnibus test. As Gaussian distribution was present, differences were tested using a paired t-test. For the reader study, the median of both readers was calculated for each subset. Then, differences between the different reconstructions were tested using the Wilcoxon signed-rank test. For each test, p value < 0.05 indicated statistical significance.
Results
Reader Study
Analyzing individual biopsy images (showing one reconstruction at a time), the highest visibility was found for VMI-40 in 75% of cases (Table 2). This results in a median visibility of 3 for VMI-40 over all cases. Hereby, the difference between VMI-40 and all other reconstructions (apart from VMI-50) as well as between VMI-50 and all other reconstructions (apart from VMI-40 and VMI-60) was significant (p < 0.05).
Median image quality was 3.5 for VMI-40 and VMI-50. For all other reconstructions, median image quality was 4. This results in a significant difference (p < 0.05) of VMI-40 as well as VMI-50 compared to all other reconstructions.
Rating the best three reconstructions regarding visibility when all reconstructions were shown simultaneously, VMI-40 was rated as top-one 30 times, VMI-50 two times and VNC five times. VMI-70 and VMI-140 were rated top-one once, respectively. One case (patient 19) could not be rated by one reader as all reconstructions appeared similar to him.
The biopsy images of three patients are shown in Figs. 1, 2, 3. Figure 1 shows the example of a lesion with the best visibility in VMI-40 images due to hyperdensity. Figure 2 shows a lesion with best visibility in VMI-40 images, and Fig. 3 shows a lesion with best visibility in VNC images. In all examples, the lesion is clearly better visible in spectral images than in conventional images.
Patient #20 with a primary intrahepatic cholangiocarcinoma. Shown are the diagnostic CT in the venous phase (top left), as well as the corresponding biopsy images. The lesion is best visible in VMI-40 image (bottom left) due to hyperdensity but also well visible in the VNC image (bottom right) due to subtraction of iodine (hypodensity). The conventional reconstruction (top right) shows the worst visibility
Patient #10, the shown lesion was histopathologically identified as necrosis. Shown are the diagnostic CT in the venous phase (top left), as well as the corresponding biopsy images. The lesion is best visible in the VMI-40 image (bottom left) due to the missing iodine uptake and thus hypodensity compared to the remaining liver parenchyma. It is also visibility in the conventional reconstruction (top right) and worst visible in the VNC image (bottom right)
Patient #7, the shown lesion was histopathologically identified as a breast cancer metastasis. Shown are the diagnostic CT in the venous phase (top left), as well as the corresponding biopsy images. The lesion is best visible in the VNC image (bottom right) due to hypodensity compared to the remaining liver parenchyma. It is also visibility in the conventional reconstruction (top right) and worst visible in the VMI-40 image (bottom left)
Objective Image Analysis
The healthy liver parenchyma was then compared to the center (Table 3) and to the periphery (Table 4) of the selected lesion. The comparison of the CNR values of the lesion and the healthy parenchyma showed ratios of 1–62 (periphery of the lesion) and 1–136 (center of the lesion). Over all cases, VMI-40 showed the highest mean contrast for center (3.40) and periphery (2.53), whereas the contrast in CI was 1.68 and 1.03, respectively. The difference between VMI-40 and any other reconstruction was significant for the center and the periphery of the lesion (p < 0.05). For the center of the lesion, VMI-40 showed the highest ratio in 14 cases and for the periphery in 12 cases, respectively. VMI-40 showed the highest ratio in either the center or the periphery in all but one case. VNC showed the highest ratio for the center in three cases and for the periphery in four cases, respectively.
Discussion
In this study, the value of virtual monoenergetic and virtual non-contrast imaging derived from spectral data of a DL-CT was evaluated for the visibility of liver lesions during CT-guided biopsy.
In clinical routine, the decreasing visibility of liver lesions over time after application of contrast medium can make CT-guides biopsies more difficult. Even though one can use anatomical landmarks for the navigation during biopsy, false-negative results or repeated biopsies are possible. It seems likely that an increased visibility of the lesion during biopsy makes the procedure easier, accelerates the process, prevents complications and increases the success rate.
In the reader study, an increased visibility via spectral imaging was reported in 16/20 cases. Hereby, VMI-40 (increasing the signal of iodine) was the preferred reconstruction and conventional images were rated worse in all cases. VNC (subtracting the iodine signal) generated the second highest visibility. In four cases, none of the spectral reconstructions was clearly superior to the others or to the conventional images. In accordance with the reader study, the ratio of the CNR between the hepatic lesion and healthy liver could be increased using VMI-40 images in most cases. However, a general recommendation for one reconstruction type cannot be given as there are cases favoring VMI-40 and others in favor of VNC. However, spectral data generate increased visibility in the majority of cases, potentially facilitating CT-guided biopsies.
As either VMI-40 or VNC was the preferred reconstruction in most cases, those reconstructions could be preferably used in the setting of a biopsy. There are different options for the selection of the best reconstruction in the biopsy protocol: first, one could place a ROI in the lesion and in normal liver parenchyma. During the further biopsy, the VMI with the highest CNR should then be automatically selected by the software and the respective image shown during the intervention. Another possibility is to show all VMI levels in the beginning of the biopsy followed by manual selection of the best reconstruction. The latter possibility seems more reasonable until automatic selection is evaluated in a larger study to prevent incorrect selection by the automatic system.
The current study has some limitations, which must be addressed. A relatively small number of patients were included, as the aim of the current study was to evaluate the general feasibility of spectral data in images derived from biopsies. Additionally, only a small number of patients received triphasic CT before biopsy or for staging, which made patient inclusion difficult. Given the promising results of the current study, additional studies with a greater number of patients will be performed. Images were analyzed retrospectively, thus the effect of VMI on the current biopsy procedures could not be evaluated. Due to patient safety, we did not perform a prospective study before proving the potential benefit of the system in a retrospective analysis. Here, further prospective studies with larger patient numbers are needed to evaluate the influence on the outcome of biopsies. Finally, we only used a DL-CT system. We believe that the results of the current study are transferable to other dual-energy systems, but this should be evaluated before application in clinical routine.
Conclusion
In conclusion, the current study shows a benefit for dual-energy derived virtual monoenergetic and virtual non-contrast images in the setting of CT-guided biopsies. A clear advantage of spectral data for the subjective visibility and objective contrast of liver lesions during biopsy could be shown in the majority of cases. Thus, this system must be further evaluated and then eventually implemented in clinical routine.
Abbreviations
- CI:
-
Conventional images
- CNR:
-
Contrast-to-noise ratio
- CT:
-
Computed tomography
- DE-CT:
-
Dual-energy CT
- DL-CT:
-
Dual-layer CT
- HU:
-
Hounsfield Units
- MRI:
-
Magnetic resonance imaging
- ROI:
-
Region of interest
- SD:
-
Standard deviation
- VNC:
-
Virtual non-contrast images
- VMI:
-
Virtual monoenergetic images
References
Leeuwen MSv, Noordzij J, Feldberg MA, Hennipman AH, Doornewaard H,. Focal liver lesions: characterization with triphasic spiral CT. Radiology. 1996;201:327–36.
Albiin N. MRI of focal liver lesions. Curr Med Imaging. 2012;8:107–16.
Marrero JA, Ahn J, Reddy RK, Gastroenterology obotPPCotACo. ACG clinical guideline: the diagnosis and management of focal liver lesions. Official J Am College Gastroenterol ACG. 2014;109:1328–47.
Francque SM, De Pauw FF, Van den Steen GH, Van Marck EA, Pelckmans PA, Michielsen PP. Biopsy of focal liver lesions: guidelines, comparison of techniques and cost-analysis. Acta Gastro-Enterol Belg. 2003;66:160–5.
Sainani NI, Schlett CL, Hahn PF, Gervais DA, Mueller PR, Arellano RS. Computed tomography-guided percutaneous biopsy of isoattenuating focal liver lesions. Abdom Imaging. 2014;39:633–44.
Sellerer T, Noel PB, Patino M, et al. Dual-energy CT: a phantom comparison of different platforms for abdominal imaging. Eur Radiol. 2018;28:2745–55.
Johnson TR. Dual-energy CT: general principles. AJR Am J Roentgenol. 2012;199:S3-8.
Ehn S, Sellerer T, Muenzel D, et al. Assessment of quantification accuracy and image quality of a full-body dual-layer spectral CT system. J Appl Clin Med Phys. 2018;19:204–17.
Sauter AP, Kopp FK, Munzel D, et al. Accuracy of iodine quantification in dual-layer spectral CT: influence of iterative reconstruction, patient habitus and tube parameters. Eur J Radiol. 2018;102:83–8.
Sauter AP, Muenzel D, Dangelmaier J, et al. Dual-layer spectral computed tomography: Virtual non-contrast in comparison to true non-contrast images. Eur J Radiol. 2018;104:108–14.
D’Angelo T, Cicero G, Mazziotti S, et al. Dual energy computed tomography virtual monoenergetic imaging: technique and clinical applications. Br J Radiol. 2019;92:20180546.
McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology. 2015;276:637–53.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was not supported by any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Roland Proksa is an employee of Philips Research Hamburg. He had no influence on the collection, analysis or interpretation of the data. All other authors declare no potential conflict of interest.
Ethical Approval
For this type of study formal consent is not required.
The institutional ethics committee approved this retrospective study.
Informed Consent
Informed consent was waived by the institutional review board (ethics committee) due to the retrospective image analysis.
Consent for Publication
For this type of study consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sauter, A.P., Proksa, R., Knipfer, A. et al. CT-Guided Liver Biopsy: Evaluation of Spectral Data From Dual-Layer Detector CT for Improved Lesion Detection. Cardiovasc Intervent Radiol 46, 1621–1631 (2023). https://doi.org/10.1007/s00270-023-03550-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-023-03550-7