Abstract
Purpose
To evaluate the effect of peri-tumoral metallic implants (MI) on the safety and efficacy of percutaneous irreversible electroporation (IRE) of colorectal liver metastasis (CRLM).
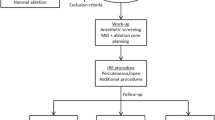
Materials and Methods
In this retrospective study, 25 patients (12 women, 13 men; MI: 13, no MI: 12) were treated for 29 CRLM. Patient characteristics, tumor location and size, treatment parameters and the presence of MI were evaluated as determinants of local tumor progression (LTP) with the competing risks model (univariate and multivariate analyses). Patient-specific computer models were created to examine the effect of the MI on the electric field used to induce IRE, probability of cell kill and potential thermal effects.
Results
Patients had a median follow-up of 25 months, during which no IRE-related major complications were reported. Univariate analysis showed that tumor size (> 2 cm), probe spacing (> 20 mm) and the presence of MI (p < 0.05) were significant predictors of time to LTP, but only the latter was found to be an independent predictor on multivariate analysis (sub-hazard ratio = 6.5; [95% CI 1.99, 21.4]; p = 0.002). The absence of peri-tumoral MI was associated with higher progression-free survival at 12 months (92.3% [56.6, 98.9] vs 12.5% [2.1, 32.8]). Computer simulations indicated significant distortions and reduction in electric field strength near MI, which could have contributed to under-treatment of the tumor.
Conclusions
Peri-tumoral MI increases the risk of treatment failure following IRE of CRLM.






Similar content being viewed by others
References
Kingham TP, Karkar AM, D’Angelica MI, et al. Ablation of perivascular hepatic malignant tumors with irreversible electroporation. J Am Coll Surg. 2012;215(3):379–87.
Cannon R, Ellis S, Hayes D, Narayanan G, Martin RCG. Safety and early efficacy of irreversible electroporation for hepatic tumors in proximity to vital structures. J Surg Oncol. 2013;107(5):544–9.
Niessen C, Igl J, Pregler B, et al. Factors associated with short-term local recurrence of liver cancer after percutaneous ablation using irreversible electroporation: a prospective single-center study. J Vasc Interv Radiol. 2015;26(5):694–702.
Scheffer HJ, Nielsen K, van Tilborg AAJM, et al. Ablation of colorectal liver metastases by irreversible electroporation: results of the COLDFIRE-I ablate-and-resect study. Eur Radiol. 2014;24(10):2467–75.
Schoellhammer HF, Goldner B, Merchant SJ, Kessler J, Fong Y, Gagandeep S. Colorectal liver metastases: making the unresectable resectable using irreversible electroporation for microscopic positive margins—a case report. BMC Cancer. 2015;15(1):271.
Dollinger M, Zeman F, Niessen C, et al. Bile duct injury after irreversible electroporation of hepatic malignancies: evaluation of MR imaging findings and laboratory values. J Vasc Interv Radiol. 2016;27(1):96–103.
Silk MT, Wimmer T, Lee KS, et al. Percutaneous ablation of peribiliary tumors with irreversible electroporation. J Vasc Interv Radiol. 2014;25(1):112–8.
Scheffer HJ, Vogel JA, van den Bos W, et al. The influence of a metal stent on the distribution of thermal energy during irreversible electroporation. PLoS ONE. 2016;11(2):e0148457.
Ben-David E, Ahmed M, Faroja M, et al. Irreversible electroporation: treatment effect is susceptible to local environment and tissue properties. Radiology. 2013;269(3):738–47.
Rems L, Miklavčič D. Tutorial: Electroporation of cells in complex materials and tissue. J Appl Phys. 2016;119(20):201101.
Goldberg SN, Grassi CJ, Cardella JF, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005;235(3):728–39.
Ahmed M, Solbiati L, Brace CL, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria—a 10-year update. Radiology. 2014;273(1):241–60.
Filippiadis DK, Binkert C, Pellerin O, Hoffmann RT, Krajina A, Pereira PL. CIRSE quality assurance document and standards for classification of complications: the CIRSE classfication system. Cardiovasc Intervent Radiol. 2017;40(8):1141–6.
Marčan M, Pavliha D, Kos B, Forjanič T, Miklavčič D. Web-based tool for visualization of electric field distribution in deep-seated body structures and planning of electroporation-based treatments. Biomed Eng Online. 2015;14(Suppl 3):S4.
Kos B, Voigt P, Miklavcic D, Moche M. Careful treatment planning enables safe ablation of liver tumors adjacent to major blood vessels by percutaneous irreversible electroporation (IRE). Radiol Oncol. 2015;49(3):234–41.
Garcia PA, Kos B, Rossmeisl JH, Pavliha D, Miklavčič D, Davalos RV. Predictive therapeutic planning for irreversible electroporation treatment of spontaneous malignant glioma. Med Phys. 2017;44(9):4968–80.
Dermol J, Miklavčič D. Mathematical models describing chinese hamster ovary cell death due to electroporation in vitro. J Membr Biol. 2015;248(5):865–81.
Garcia PA, Davalos RV, Miklavcic D. A numerical investigation of the electric and thermal cell kill distributions in electroporation-based therapies in tissue. PLoS ONE. 2014;9(8):e103083.
Donoghoe MW, Gebski V. The importance of censoring in competing risks analysis of the subdistribution hazard. BMC Med Res Methodol. 2017;17(1):52.
Gallinato O, de Senneville BD, Seror O, Poignard C. Numerical workflow of irreversible electroporation for deep-seated tumor. Phys. Med. Biol. 2019;64(5):055016.
Margonis GA, Sasaki K, Andreatos N, et al. KRAS mutation status dictates optimal surgical margin width in patients undergoing resection of colorectal liver metastases. Ann Surg Oncol. 2017;24(1):264–71.
Akyuz M, Aucejo F, Quintini C, Miller C, Fung J, Berber E. Factors affecting surgical margin recurrence after hepatectomy for colorectal liver metastases. Gland Surg. 2016;5(3):263–9.
Vroomen LGPH, Petre EN, Cornelis FH, Solomon SB, Srimathveeravalli G. Irreversible electroporation and thermal ablation of tumors in the liver, lung, kidney and bone: What are the differences? Diagn Interv Imaging. 2017;98(9):609–17.
Neal RE, Smith RL, Kavnoudias H, et al. The effects of metallic implants on electroporation therapies: feasibility of irreversible electroporation for brachytherapy salvage. Cardiovasc Intervent Radiol. 2013;36(6):1638–45.
Dunki-Jacobs EM, Philips P, Martin RCG. Evaluation of thermal injury to liver, pancreas and kidney during irreversible electroporation in an in vivo experimental model. Br J Surg. 2014;101(9):1113–21.
Månsson C, Nilsson A, Karlson B-M. Severe complications with irreversible electroporation of the pancreas in the presence of a metallic stent: a warning of a procedure that never should be performed. Acta Radiol Short Rep. 2014. https://doi.org/10.1177/2047981614556409.
Yarmush ML, Golberg A, Serša G, Kotnik T, Miklavčič D. Electroporation-based technologies for medicine: principles, applications, and challenges. Annu Rev Biomed Eng. 2014;16:295–32020.
O’Brien TJ, Bonakdar M, Bhonsle S, et al. Effects of internal electrode cooling on irreversible electroporation using a perfused organ model. Int J Hyperthermia. 2018;35:44–55.
Faroja M, Ahmed M, Appelbaum L, et al. Irreversible electroporation ablation: is all the damage nonthermal? Radiology. 2013;266(2):462–70.
Edhemović I, Brecelj E, Gasljevic G, et al. Intraoperative electrochemotherapy of colorectal liver metastases. J Surg Oncol. 2014;110(3):320–7.
Edhemovic I, Gadzijev EM, Brecelj E, et al. Electrochemotherapy: a new technological approach in treatment of metastases in the liver. Technol Cancer Res Treat. 2011;10(5):475–85.
Djokic M, Cemazar M, Popovic P, et al. Electrochemotherapy as treatment option for hepatocellular carcinoma, a prospective pilot study. Eur J Surg Oncol. 2018;44(5):651–7.
Acknowledgements
The authors acknowledge the support of NIH Cancer Center Support Grant (P30 CA008748) for core laboratory services that were used for the presented work. The authors acknowledge the support of the National Cancer Institute of the National Institutes of Health under Award Numbers U54CA137788/U54CA132378, and the Slovenian Research Agency (ARRS), Slovenia Program P2-0249, Grant Z3-7126 and Bilateral Slovenian-USA project BI-US/18-19-002. SBS is a consultant to BTG, Johnson & Johnson, XACT, Adegro and Medtronic. SBS is a consultant to BTG, Johnson & Johnson, XACT, Adgero, Innobaltive, and Medtronic. SBS has funding support from GE Healthcare, Ethicon, Elesta and Angiodynamics, and holds stock in Aperture Medical.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interests.
Ethical Approval
All procedures were performed in accordance with the ethical standards of the institutional or national research committee, and with the Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
For this type of study, informed consent is not required.
Consent for Publication
For this type of study, consent for publication is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Cornelis, F.H., Cindrič, H., Kos, B. et al. Peri-tumoral Metallic Implants Reduce the Efficacy of Irreversible Electroporation for the Ablation of Colorectal Liver Metastases. Cardiovasc Intervent Radiol 43, 84–93 (2020). https://doi.org/10.1007/s00270-019-02300-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-019-02300-y