Abstract
Introduction
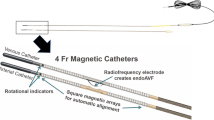
Dysfunctional or infected hemodialysis polyester-cuffed catheters often require removal and are dissected out. The DermaPort™, percutaneous vascular access system (PVAS) permanently integrates a titanium mesh with the skin forming a stable, sterile barrier that allows for catheter placement, adjustment, or catheter exchange. This study aimed to describe the use and clinical outcomes of the DermaPort PVAS.
Methods
Thirty-eight patients who were receiving hemodialysis via a tunneled catheter were enrolled in this prospective open-label study. Assessments were performed biweekly for the first month and monthly thereafter, which included physical examination of the site of implantation for infection, catheter blood flow, and need for interventions to maintain catheter patency. Patient satisfaction was assessed with a visual analog score.
Results
Implantation of technical success was 100% with the implantation site demonstrating early tissue incorporation after 2 weeks and full incorporation within 4 weeks. The DermaPort™ successfully enabled 31 catheter exchanges and 10 repositions thru the port without dissection in 18 patients with nine repositions (90%) performed at bedside. The mean primary patency of the DermaPort™ was 172 ± 150 days, and mean secondary patency was 430 ± 203 days. There were no reportable serious adverse events in 12,100 catheter days of use and zero explantations of the device attributed to infection. The observed catheter infection rate was 0.33/1000 days.
Conclusions
The DermaPort™ system can be effectively implanted and facilitates catheter interventions in hemodialysis patients requiring long-term catheter use and has a lower infection rate than historical catheter infection rates.
Clinical Trial Protocol Number DermaPort-001 (no clinicaltrials.gov number as study was performed 9 years ago).
Health Canada Reference Application Number: 118393.




Similar content being viewed by others
Abbreviations
- CRI:
-
Catheter-related infection
- PVAS:
-
Percutaneous vascular access system
- SD:
-
Standard deviation
- SQ:
-
Subcutaneous
- QB:
-
Blood flow rate
- TDC:
-
Tunneled dialysis catheters
- VAS:
-
Visual analog scales
References
Clinical Practice Guidelines for Vascular Access. Am J Kidney Dis. 2006;48:S176–247. https://doi.org/10.1053/j.ajkd.2006.04.029.
Santoro A, Canova C, Freyrie A, Mancini E. Vascular access for hemodialysis. J Nephrol. 2006;19(3):259–64.
Mickley V. Central venous catheters: many questions, few answers. Nephrol Dial Transpl. 2002;17(8):1368–73.
Trerotola SO. Hemodialysis catheter placement and management. Radiology. 2000;215(3):651–8.
Kohli MD, Trerotola SO, Namyslowski J, Stecker MS, McLennan G, Patel NH, et al. Outcome of polyester cuff retention following traction removal of tunneled central venous catheters. Radiology. 2001;219(3):651–4.
Janne d’Othee B, Tham JC, Sheiman RG. Restoration of patency in failing tunneled hemodialysis catheters: a comparison of catheter exchange, exchange and balloon disruption of the fibrin sheath, and femoral stripping. J Vasc Interv Radiol. 2006;17(6):1011–5.
Janis AD, Kunz LL, Porter C, Moran B, Mayton C, Richmond KN. Biomaterial prevents epidermal downgrowth along a percutaneous implant in rabbits. In: BioMedical engineering society annual fall meeting. Los Angeles (2007).
Janis AD, Kunz LL, Porter C, Moran B, Mayton C, Richmond KN, editors. Percutaneously implanted titanium mesh biomaterial reestablishes an epidermal seal by 3 weeks in rabbits. In: BioMedical engineering society annual fall meeting. Los Angeles (2007).
Grant S, Aitchison T, Henderson E, Christie J, Zare S, McMurray J, et al. A comparison of the reproducibility and the sensitivity to change of visual analogue scales, Borg scales, and Likert scales in normal subjects during submaximal exercise. Chest. 1999;116(5):1208–17. https://doi.org/10.1378/chest.116.5.1208.
Lok CE, Foley R. Vascular access morbidity and mortality: trends of the last decade. Clin J Am Soc Nephrol. 2013;8(7):1213–9. https://doi.org/10.2215/CJN.01690213.
Griffiths RI, Newsome BB, Block GA, Herbert RJ, Danese MD. Patterns of hemodialysis catheter dysfunction defined according to national kidney foundation guidelines as blood flow < 300 mL/min. Int J Nephrol. 2011;2011:891259. https://doi.org/10.4061/2011/891259.
Kowalski CM, Kaufman JA, Rivitz SM, Geller SC, Waltman AC. Migration of central venous catheters: implications for initial catheter tip positioning. J Vasc Interv Radiol. 1997;8(3):443–7.
Timsit JF, Sebille V, Farkas JC, Misset B, Martin JB, Chevret S, et al. Effect of subcutaneous tunneling on internal jugular catheter-related sepsis in critically ill patients: a prospective randomized multicenter study. JAMA. 1996;276(17):1416–20.
Allon M. Treatment guidelines for dialysis catheter-related bacteremia: an update. Am J Kidney Dis. 2009;54(1):13–7. https://doi.org/10.1053/j.ajkd.2009.04.006.
Hemmelgarn BR, Moist L, Pilkey RM, Lok C, Dorval M, Tam PY, et al. Prevention of catheter lumen occlusion with rT-PA versus heparin (pre-CLOT): study protocol of a randomized trial [ISRCTN35253449]. BMC Nephrol. 2006;7:8. https://doi.org/10.1186/1471-2369-7-8.
Ravani P, Gillespie BW, Quinn RR, MacRae J, Manns B, Mendelssohn D, et al. Temporal risk profile for infectious and noninfectious complications of hemodialysis access. J Am Soc Nephrol. 2013;24(10):1668–77. https://doi.org/10.1681/ASN.2012121234.
Ravani P, Palmer SC, Oliver MJ, Quinn RR, MacRae JM, Tai DJ, et al. Associations between hemodialysis access type and clinical outcomes: a systematic review. J Am Soc Nephrol. 2013;24(3):465–73. https://doi.org/10.1681/ASN.2012070643.
Ravani P, Quinn R, Oliver M, Robinson B, Pisoni R, Pannu N, et al. Examining the association between hemodialysis access type and mortality: the role of access complications. Clin J Am Soc Nephrol. 2017;12(6):955–64. https://doi.org/10.2215/CJN.12181116.
Foley RN, Guo H, Snyder JJ, Gilbertson DT, Collins AJ. Septicemia in the United States dialysis population, 1991 to 1999. J Am Soc Nephrol. 2004;15(4):1038–45.
Ramanathan V, Chiu EJ, Thomas JT, Khan A, Dolson GM, Darouiche RO. Healthcare costs associated with hemodialysis catheter-related infections: a single-center experience. Infect Control Hosp Epidemiol. 2007;28(5):606–9. https://doi.org/10.1086/513617.
Shingarev R, Barker-Finkel J, Allon M. Natural history of tunneled dialysis catheters placed for hemodialysis initiation. J Vasc Interv Radiol. 2013;24(9):1289–94. https://doi.org/10.1016/j.jvir.2013.05.034.
Acknowledgements
The authors acknowledge the following people for their help in this study: Anna-Marie Sutherland (Former Clinical Coordinator, Lakeridge Health); Abe Janis (Former Technical Liaison for Scientific Development, DermaPort, Inc.). We thank Richard Holcomb for statistical support of this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
All authors declare that they have no conflict of interest.
Ethical Standards
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committees and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Financial Support
We acknowledge DermaPort, Inc. for funding this clinical trial. We also thank the Alfred Mann Institute for Biomedical Research at the University of Southern California for support of this paper. Dheeraj K. Rajan, Murray Asch, and Andrew Steele were paid consultants to DermaPort, Inc.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Rajan, D.K., Moran, B., Lobl, T.J. et al. A Prospective Clinical Study of a Percutaneous Vascular Access System for Hemodialysis Catheters. Cardiovasc Intervent Radiol 41, 1513–1519 (2018). https://doi.org/10.1007/s00270-018-2031-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-018-2031-z