Abstract
Background
Gynecomastia (GYN) is the most common benign disease in males. A vacuum-assisted biopsy is a minimally invasive surgical technique for GYN treatment that achieves satisfactory aesthetic results. However, due to the operation under non-direct vision, it is difficult to localize the bleeding points and assess the residual glandular tissue. Endoscopy was applied to observe the operative field after subcutaneous mastectomy. The present study aimed to recommend our initial experience in glandular GYN with endoscope-assisted minimally invasive subcutaneous mastectomy.
Methods
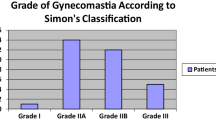
A total of 34 patients diagnosed with glandular GYN (50 breasts), treated with endoscope-assisted minimally invasive surgery at The First Affiliated Hospital with Nanjing Medical University between June 2018 and June 2020, were enrolled in this study. According to Simon’s classification of the breast, 10 was grade I, 25 was grade IIA, and 15 was grade IIB. The characteristics of patients, operative data, postoperative complications, cosmetic outcome, and patient satisfaction were recorded.
Results
Endoscope-assisted minimally invasive mastectomy was performed successfully in all cases. The operative duration of the operation was 55–120 min/side. The total weight of the resected tissue of the 50 breasts was 55–350 g, and the blood loss was 10–105 mL/breast. Endoscopy detected five breasts with bleeding and three with residual glandular during the operation. Postoperative bleeding occurred in 1 breast, subcutaneous seroma in 3 breasts, dysesthesia of the nipple–areolar complex in 2 breasts, and skin redundancy in a bilateral patient. None of the patients experienced severe pain, infection, nipple necrosis, and nipple retraction, a saucer-like deformity. With a median follow-up of 21 months, all patients were satisfied with their cosmetic outcome (100%), and no recurrence occurred.
Conclusion
Endoscope-assisted minimally invasive mastectomy could be used as a feasible technique for the treatment of glandular GYN.
Level of Evidence IV
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online. Instructions to Authors www.springer.com/00266.





Similar content being viewed by others
Change history
21 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s00266-022-02862-2
References
Rahmani S, Turton P, Shaaban A, Dall B (2011) Overview of gynecomastia in the modern era and the leeds gynaecomastia investigation algorithm. Breast J 17(3):246–255
Klang E, Kanana N, Grossman A, Raskin S, Pikovsky J, Sklair M, Heller L, Soffer S, Marom EM, Konen E, Amitai MM (2018) Quantitative CT assessment of gynecomastia in the general population and in dialysis, cirrhotic, and obese patients. Acad Radiol 25(5):626–635
Wang Y, Wang J, Liu L, Liang W, Qin Y, Zheng Z, Zou S, Xu Y, Chen C, Feng Z, Zhang J, Tao L, Chen X (2019) Comparison of curative effects between mammotome-assisted minimally invasive resection (MAMIR) and traditional open surgery for gynecomastia in Chinese patients: a prospective clinical study. Breast J 25(6):1084–1089
Nuttall FQ, Warrier RS, Gannon MC (2015) Gynecomastia and drugs: a critical evaluation of the literature. Eur J Clin Pharmacol 71(5):569–578
Narula HS, Carlson HE (2014) Gynaecomastia-pathophysiology, diagnosis and treatment. Nat Rev Endocrinol 10(11):684–698
Leung AKC, Leung AAC (2017) Gynecomastia in infants, children, and adolescents. Recent Pat Endocr Metab Immune Drug Discov 10(2):127–137
Abdelrahman I, Steinvall I, Mossaad B, Sjoberg F, Elmasry M (2018) Evaluation of glandular liposculpture as a single treatment for grades I and II gynaecomastia. Aesthet Plast Surg 42(5):1222–1230
Caridi RC (2018) Defining the aesthetic units of the male chest and how they relate to gynecomastia based on 635 patients. Plast Reconstr Surg 142(4):904–907
Waltho D, Hatchell A, Thoma A (2017) Gynecomastia classification for surgical management. Plast Reconstr Surg 139(3):638e–648e
Liu J, Han Y, Cheng K, Wang XH, Guo F, Yang ZL (2018) Single-incision surgery for gynecomastia using TriPort: a case report. Exp Ther Med 16(2):797–801
Simon BE, Hoffman S, Kahn S (1973) Classification and surgical correction of gynecomastia. Plast Reconstr Surg 51(1):48–52
Webster DJ (1989) Benign disorders of the male breast. World J Surg 13(6):726–730
El Sabbagh AH (2016) Combined approach for gynecomastia. GMS Interdiscip plast reconst surg DGPW 5:c10
Fricke A, Lehner GM, Stark GB, Penna V (2017) Long-term follow-up of recurrence and patient satisfaction after surgical treatment of gynecomastia. Aesthet Plast Surg 41(3):491–498
Wyrick DL, Roberts M, Young ZT, Mancino AT (2018) Changing practices: the addition of a novel surgical approach to gynecomastia. Am J Surg 216(3):547–550
Kim DH, Byun IH, Lee WJ, Rah DK, Kim JY, Lee DW (2016) Surgical management of gynecomastia: subcutaneous mastectomy and liposuction. Aesthet Plast Surg 40(6):877–884
Longheu A, Medas F, Corrias F, Farris S, Tatti A, Pisano G, Erdas E, Calò PG (2016) Surgical management of gynecomastia: experience of a general surgery center. II Giornale di Chirurgia 37(4):150–154
Rohrich RJ, Ha RY, Kenkel JM, Adams WP Jr (2003) Classification and management of gynecomastia: defining the role of ultrasound-assisted liposuction. Plast Reconstr Surg 111(2):909–923
Benito-Ruiz J, Raigosa M, Manzano M, Salvador L (2009) Assessment of a suction-assisted cartilage shaver plus liposuction for the treatment of gynecomastia. Aesthetic Surg J 29(4):302–309
Goh T, Tan BK, Song C (2010) Use of the microdebrider for treatment of fibrous gynaecomastia. J Plast Reconstr Aesthet Surg 63(3):506–510
Cao H, Yang ZX, Sun YH, Wu HR, Jiang GQ (2013) Endoscopic subcutaneous mastectomy: a novel and effective treatment for gynecomastia. Exp Ther Med 5(6):1683–1686
Qutob O, Elahi B, Garimella V, Ihsan N, Drew PJ (2010) Minimally invasive excision of gynaecomastia—a novel and effective surgical technique. Ann R Coll Surg Engl 92(3):198–200
Park HL, Kim KY, Park JS, Shin JE, Kim HR, Yang B, Kim JY, Shim JY, Shin EA, Noh SM (2018) Clinicopathological analysis of ultrasound-guided vacuum-assisted breast biopsy for the diagnosis and treatment of breast disease. Anticancer Res 38(4):2455–2462
Bennett I, de Viana D, Law M, Saboo A (2020) Surgeon-performed vacuum-assisted biopsy of the breast: results from a multicentre australian study. World J Surg 44(3):819–824
Iwuagwu OC, Calvey TA, Ilsley D, Drew PJ (2004) Ultrasound guided minimally invasive breast surgery (UMIBS): a superior technique for gynecomastia. Ann Plast Surg 52(2):131–133
Yao Y, Yang Y, Liu J, Wang Y, Zhao Y (2019) Vacuum-assisted minimally invasive surgery—an innovative method for the operative treatment of gynecomastia. Surgery 166(5):934–939
Yi JG, Kim SJ, Marom EM, Park JH, Jung SI, Lee MW (2008) Chest CT of incidental breast lesions. J Thorac Imaging 23(2):148–155
Fan L, Yang X, Zhang Y, Jiang J (2009) Endoscopic subcutaneous mastectomy for the treatment of gynecomastia: a report of 65 cases. Surg Laparosc Endosc Percutaneous Tech 19(3):e85–e90
Blau M, Hazani R (2015) Correction of gynecomastia in body builders and patients with good physique. Plast Reconstr Surg 135(2):425–432
Kasielska A, Antoszewski B (2013) Surgical management of gynecomastia: an outcome analysis. Ann Plast Surg 71(5):471–475
Ridha H, Colville RJ, Vesely MJ (2009) How happy are patients with their gynaecomastia reduction surgery? J Plast Reconstr Aesthet Surg 62(11):1473–1478
Jian C, Wu L, Lin L, Liu W, Zheng Z, Yang C (2020) Single-port endoscopic mastectomy via the lateral chest approach for the treatment of grade II gynecomastia. Medicine 99(22):e20100
Zannis VJ, Aliano KM (1998) The evolving practice pattern of the breast surgeon with disappearance of open biopsy for nonpalpable lesions. Am J Surg 176(6):525–528
Murugesan L, Karidis A (2020) External quilting: new technique to avoid haematoma in gynaecomastia surgery. Aesthet Plast Surg 44(1):45–51
Acknowledgments
The authors would like to thank all the patients who participated in this study and those who helped during the writing of this manuscript.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no proprietary or commercial interest in any product mentioned or concept discussed in this article.
Ethical Approval
The principles outlined in the Declaration of Helsinki have been followed, and this study was approved by the Ethics Committee of the First Affiliated Hospital with Nanjing Medical University.
Informed Consent
Written informed consent was obtained from all participants before the operation.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Congcong Liu, Ying Tong, and Feixiang Sun contributed equally to this work.
This article was updated to add the equal contribution note to the PDF.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file1 (WMV 244493 KB)
Rights and permissions
About this article
Cite this article
Liu, C., Tong, Y., Sun, F. et al. Endoscope-Assisted Minimally Invasive Surgery for the Treatment of Glandular Gynecomastia. Aesth Plast Surg 46, 2655–2664 (2022). https://doi.org/10.1007/s00266-022-02807-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-022-02807-9