Abstract
Purpose
Although bone transport is a well-recognised technique to address segmental bone defects, optimal management of docking sites is not absolutely determined. Some surgeons routinely intervene in all cases, and others prefer to observe and intervene only if spontaneous union does not occur. Primary aim of the study was to compare rates of docking site union between patients who underwent routine docking site intervention and those who did not.
Methods
A systematic literature review using the keywords “bone transport”, “docking”, “tibia”, and “femur” was performed in PubMed using PRISMA guidelines. Studies published in English from January 2000 to August 2022 were included and assessed independently by two reviewers. Pooled analysis was undertaken dividing patients into two groups: those managed by routine intervention and those initially observed.
Results
Twenty-three clinical studies met the eligibility criteria for pooled analysis, including 1153 patients, 407 in the routine intervention and 746 in the observed group. The rate of union after initial treatment was 90% in the routine intervention group and 66% in the observed group (p < 0.0001). Overall union rates at the end of treatment were similar at 99% in both groups. Patients in the observed group required an average of 2.2 procedures to achieve union overall compared with 3.8 in the routine intervention group. Time in frame was similar between groups.
Conclusion
Based on the current literature, routine docking site interventions cannot be recommended, since this may lead to unnecessary interventions in two thirds of patients. Timely selective intervention in those at high risk or after a defined period of observation would appear to be a logical approach.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Critical segmental bone defects present one of the most challenging situations faced by orthopaedic surgeons. Although the Masquelet technique has risen in popularity, perhaps related to the familiarity of required implants and techniques [1,2,3,4], distraction osteogenesis remains the most widely utilised approach for bone regeneration [5, 6]. Popularised by Ilizarov, the technique employs callus distraction to form new bone [7]. An osteotomy is undertaken away from the defect, and after a short latent period to allow callus formation to begin, gradual distraction is applied, traditionally by external fixation, at a rate of around 1 mm a day. The main purported advantages of this over other methods include elimination of donor site morbidity from bone graft harvest, avoidance of internal implants (particularly in cases complicated by infection), reduced violation of the soft tissue envelope, early or immediate weight bearing and the creation of a regenerate bone similar in diameter and morphology to healthy long bones [7, 8]. It has also been suggested that the increased limb blood flow generated during distraction may be helpful in eliminating infection [9], making its use in defects resulting from open fractures, fracture-related infections or osteomyelitis particularly attractive [10].
There are a variety of strategies which can be used when treating osseous defects by bone transport. These can be defined based on the initial management of the bone defect and the number of distraction sites. In shorter defects, usually 5 cm or less, the gap can be acutely shortened to achieve immediate contact, and then, the bone lengthened at a distant site. This is termed acute shortening and re-lengthening [11]. Maintaining overall length and moving a segment of bone to close the defect over time are known as bone transport. This can be bifocal, with a single osteotomy site for distraction, or trifocal where a double osteotomy is used to create two distraction sites (Fig. 1) [12, 13].
Distraction osteogenesis can be achieved using circular or monolateral fixators [12, 14, 15] or more recently using magnetic nails for all internal transport [16,17,18]. Combination with internal fixation can be undertaken to reduce external fixator time [19,20,21]. There are also reports of utilising membrane induction as in the Masquelet technique in an attempt to improve healing [22]. Regardless of technique, the result is the apposition of the two opposing surfaces of the bone defect at the “docking site”. Achieving union at the docking site can be challenging. Opinion varies regarding the management of these sites, with some surgeons choosing to simply apply ongoing compression for a period and others undertaking planned surgical interventions at the time of docking to augment healing. Various strategies to enhance union have been described, including open [12, 23], closed [8, 24] and endoscopic techniques[25], the use of bone grafts or growth factors [12, 25,26,27] and the application of additional implants. This does however risk further violation of an already traumatised soft tissue envelope in the presence of external fixation hardware, which makes the maintenance of sterility during the procedure and access more difficult. It therefore potentially places the patients at risk of catastrophic complications which could jeopardise the treatment outcome. There is no generally accepted consensus, and docking site protocols remain a controversial topic [27,28,29]. We therefore undertook a systematic review of the literature regarding this topic with the aim of answering the following questions:
In adult patients undergoing distraction osteogenesis for lower limb bone defects resulting from trauma, osteomyelitis or fracture-related infection, compared to simple compression, is planned operative docking site intervention associated with
-
(1)
Increased union rates without further intervention?
-
(2)
Increased overall treatment failure?
As a secondary aim, we planned to examine the literature in an attempt to determine which bone transport strategies/locations were associated with increased docking site union.
Methods
Literature search strategy
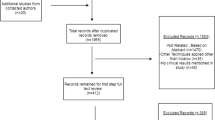
A systematic search according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) statement [30] using the search terms “((bone transport) OR (docking)) AND ((tibia) OR (femur))” was performed. The search was limited to the database Medline. During initial screening, articles, titles and abstracts were reviewed by the first and second authors for relevance. Relevant full-text articles were then obtained and evaluated according to the eligibility criteria of the study and relevant data extracted (Fig. 2). Any disagreement between the two reviewers was resolved by consensus following the discussion with the senior author. The reviewers were not blinded to the names of authors, institutions or journals.
Eligibility criteria
Studies were included if they met the following criteria:
-
(1)
Bone transport is performed by external fixation for bone defects resulting from trauma, osteomyelitis or fracture-related infections of the lower extremity
-
(2)
Reported outcomes regarding the healing of the docking site
-
(3)
Clinical studies in humans with the full-text paper published between January 2000 and August 2022
Studies were excluded if they met the following criteria:
-
(1)
Reviews, conference abstracts, animal studies, letters or comments
-
(2)
Full-text paper written in English was not available
-
(3)
Studies which routinely combined internal with external fixation
-
(4)
Studies where the reporting precluded accurate data extraction for the main review outcomes
-
(5)
Studies including less than 10 patients
Assimilation of data
Studies were divided into groups depending on whether docking sites underwent planned operative intervention (planned intervention) of any nature or were observed initially (observed), and intervention is undertaken only if union did not occur. Where studies included patients managed by both approaches, these were reported in each group as appropriate. The main study outcomes were the number of patients in whom uncomplicated docking site union occurred (no further interventions to union, no docking site refracture after frame removal), the mean number of procedures to achieve union and the number of patients in whom union was ultimately achieved. Other data extracted from the manuscripts included the author’s details, sample size, location of bone defect, specific inclusion/exclusion criteria, fixation device, type of osteotomy, soft tissue coverage requirements, docking procedures, size of defect, healing index, external fixator time and mean bone transport time. A narrative literature review summarising relevant findings from individual papers, particularly focused on risk factors for docking site non-union, is presented alongside the pooled analysis. Studies excluded from the pooled analysis were still included in the narrative review where relevant.
Statistical analysis
Insufficient prospective comparative studies were identified to allow formal meta-analysis of randomised controlled trials. Extracted data were therefore described as in the original manuscripts, and pooled analysis of extracted data from observational studies was undertaken to answer the 2 main research questions. A chi-squared or Fisher’s exact test was used as appropriate to compare nominal results. Statistical analysis was undertaken using GraphPad computer software (Version 6.04).
Results
Does routine docking site intervention improve outcomes?
The initial search identified 1251 publications. Twenty-three of these met the eligibility criteria for the pooled analysis, including 1153 patients treated by distraction osteogenesis [8, 12, 14, 15, 22,23,24,25,26,27,28, 31,32,33,34,35,36,37,38,39,40,41,42]. Details of each study are shown in Table 1. Extracted data from each study and pooled analysis are shown in by docking site intervention group in Table 2 (planned intervention) [12, 14, 15, 23, 25,26,27,28, 31,32,33] and Table 3 (observed) [8, 24, 33, 38,39,40,41,42]. Where patients from a single study had different docking site protocols, these were included in the relevant group. In total, there were 407 patients in the planned intervention group and 746 in the observed group. In the planned intervention group, 368 of 407 (90%) docking sites went on to union without further intervention, compared to 497 of 746 (66%) in the observed group. This result was statistically significant (chi-squared p < 0.0001). Included within these failures at the docking site were 7 refractures in the planned intervention group [12, 28, 32, 33] compared with 21 in the observation group [23, 24, 27, 32,33,34, 41] (not significant, p = 0.28). For those studies reporting the outcome, more surgical procedures overall (including planned and unplanned) were required to achieve union in the planned intervention group than the observation group (mean 3.8 in 160 patients from four studies vs. mean 2.2 in 333 patients from 10 studies). The proportion of patients in whom union was ultimately achieved was similar between the two groups, being 402 of 407 (99%) in the planned procedure group vs. 737 of 746 (99%) in the observed group (chi-squared p =0.612). Overall treatment time is difficult to estimate between groups without access to the raw data. Calculating an average based upon the data as reported in each paper, where this was available, and the number of patients treated reveals that this is similar at 383 days (275 patients) in the planned intervention group and 393 days (642 patients) in the observed group. These results were highly variable between studies due to their heterogenous nature, and the methodology of pooled analysis is weak; these results should be viewed with caution.
Other factors associated with docking site outcome
The heterogenous nature of the studies and problems with reporting made it difficult to draw conclusions regarding what type of docking procedure is most effective. All studies in the planned procedure group included refreshing the bone ends in their operative protocol for the docking site intervention, though some undertook this using minimally invasive techniques [25, 27]. Many used autologous bone graft, though this was used selectively within studies, making any attempt to understand the effectiveness of this intervention compared to others prone to selection bias. In several studies, it was not possible to determine the outcome of different patients based upon which intervention was applied, as this was not part of the main research question and therefore not reported. Considering studies where it was possible to reliably extract relevant data, in patients where the bone graft was applied, union occurred without further intervention in 90 of 105 cases (86%) compared with 58 of 59 cases (98%) where this was not used (Fisher’s exact test p < 0.01). For the reasons stated above, this should be interpreted with caution. We present a case of docking site non-union in a patient treated for infected non-union of the femur managed by bone grafting in Fig. 3.
Docking site non-union in patient treated for infected non-union of femur managed by bone grafting. A Initial radiographs following removal of femoral nail and debridement (left). A monolateral external fixator is applied for bifocal bone transport with partial shortening (right). B Standing alignment films show transport and re-lengthening is complete. C Distraction segment has consolidated but docking site appears to only have tenuous union at best. Simple compression has been applied follow by compression and distraction (accordian technique). CT confirms docking site non-union. D Patient undergoes docking site procedure with freshening of the bone ends and application of autologous bone graft along with bone marrow aspirate concentrate and bioactive glass graft expander. E At 4 months post grafting, the docking site appears to have united, and the fixator is removed. F Radiographs at 12 months post fixator removal show union and remodelling of the docking site
Due to the nature of the intervention, all patients in the planned intervention group were treated by bone transport, whereas some in the observed group underwent acute shortening and re-lengthening (ASR) [33, 35, 37, 38, 41]. Outcomes were therefore compared only for those patients treated without routine docking site intervention (observed group) between those managed by ASR or bone transport. In papers, where it was possible to reliably extract data, the uncomplicated docking site union rate in patients treated with ASR was 96 of 128 (75%) compared to 420 of 618 (68%) managed by bone transport. This difference was not statistically significant (chi-squared p = 0.11).
Some studies managed patients by bifocal and some by trifocal bone transport. In several studies, a mix of these techniques was used, and in several, it was not possible to determine outcomes by this factor due to the nature of reporting. In the remaining papers, docking site union was compared by this factor in the observed group, where it likely has the most impact. The rate of uncomplicated docking site union was 209 of 280 in those managed by bifocal transport (75%) compared to 31 of 37 managed by trifocal transport (84%). This result was not statistically significant (Fisher’s exact p = 0.31), though due to the issues stated this is difficult to interpret and the numbers small.
Two studies in the observed group reported the use of either poly-methyl methacrylate or calcium sulphate bone cement within the defect (54 patients) [22, 37]. The rationale for this is to induce a biologically active membrane to assist union and regenerate formation. These patients had a higher spontaneous docking site union rate when compared with the remaining 692 patients from the observed group (45 of 54 (83%) vs. 420 of 692 (61%), chi-squared test p = 0.0009). Again, given the heterogenous nature of the studies, this result should be viewed with caution.
Results of narrative review
Docking site union is likely to occur by a combination of endochondral and intramembranous ossification, and the exact mechanism remains unclear [7]. As for bone healing in other situations, the interaction of host biology, local and systemic and mechanics will influence this. The following factors, relevant to the surgical technique, are thought likely to be particularly important in docking site union [7, 9, 24, 29].
-
(1)
Bone contact: Greater contact area between bone surfaces will increase the probability of union and decrease rates of refracture. Bone contact is influenced by the geometry of the bone cuts at debridement and the accuracy of the bone transport device in maintaining alignment. We present a case of docking site refracture managed non-operatively in Fig. 4.
-
(2)
Infection: Unresolved infection at a docking site will affect local biology and is likely to be detrimental to union. Appropriate debridement and antimicrobial strategies likely influence this.
-
(3)
Vascularity: Sufficient blood supply is critical to bone healing. Thorough debridement of necrotic bone is likely to be important in achieving vascularized bony surfaces to facilitate healing.
-
(4)
Mechanics: Alignment and stability are important in generating appropriate mechanical environments for bony healing. This factor is affected by the stabilisation technique employed for the docking site and will also be influenced by the degree of contact.
Docking site refracture managed non-operatively. A Patient has apparently successfully completed treatment for a Gustilo and Anderson IIIB open tibial fracture with bone loss. Note consolidated proximal transport segment and mid-diaphyseal docking site which appears united after simple compression. B Radiographs early after frame removal appear to show a united tibia. C Patient stumbles and suffers a low energy fracture. Radiographs reveal a minimally displaced refracture at the docking site. D A plaster cast is applied and wedged to restore alignment. E Spontaneous union of the refracture occurs over 4 months. Note that the docking site has better union than prior to the refracture
Docking site healing is substantially different from fracture healing. In all circumstances, the local biology at the docking site will have been significantly damaged by trauma, surgery and in some cases infection. This will result in decreased local blood supply, deleterious to healing. The haematoma and inflammation, which constitute the first stage of secondary bone healing, are missing in cases of bone transport because docking occurs several weeks after the injury [43]. This results in the formation of a fibrous connective cap, again believed to have an adverse effect on bone healing. Though the bone ends are fashioned so that there should be good coaptation on contact, this is difficult to achieve, and during the transport process, bone resorption often occurs, worsening contact further [17]. The lack of fracture haematoma at docking will exacerbate this problem, potentially making gap healing less likely to occur. Even in cases of acute shortening, surgical intervention removes this haematoma to a significant extent, and the damage to the local blood supply may still result in bone resorption and problems with bone contact, with similar results [44].
Docking site operations are not without the potential for complication. The most commonly reported are local infections, soft tissue problems, and donor site morbidity [15, 25, 26]. Undertaking open surgical procedures within the confines of a circular frame can be challenging and raises issues around the maintenance of a sterile field. This leads to concerns over deep infection threatening the ultimate outcome. Docking procedures also do not guarantee union. The studies considered in the pooled analysis report rates of further docking site problems requiring intervention 0 to 32% (10% overall) in the routine intervention group. This should be considered when consenting patients for these procedures.
Location of the defect
The majority of included studies deal with tibial bone loss [8, 12, 14, 15, 22,23,24,25,26,27,28, 31,32,33,34,35, 37,38,39,40]. This is unsurprising since the tibia is a subcutaneous bone, prone to open injuries, with a tenuous blood supply particularly in the distal third [45]. Although many studies subdivide tibial defects into defects of the proximal, middle, and distal third, no data were identified regarding an association between docking site union rate and location within the bone. In addition, insufficient data was available to assess if the location of the corticotomy and therefore direction of the transport (antegrade/retrograde) have an influence on docking site union. Studies reporting outcomes following distraction osteogenesis in the femur are less common [41, 42]. The femur is surrounded by muscle and has a better blood supply than the tibia, meaning post-traumatic bone loss and fracture-related infections are less common. Femoral cases are more usually undertaken using monolateral fixators, due to the impracticalities of using circular fixation in the thigh. There may also be a propensity to use other approaches in the femur, such as the induced membrane technique with internal fixation, for the same reasons. Indeed, the use of magnetic lengthening nails is increasing in the femur, particularly for lengthening in cases of congenital shortening, which is not considered here. One might expect a higher docking site union rate in the femur than the tibia due to the better blood supply, but this could not be demonstrated by the data presented here.
Due to perceived differences in the relevant pathologies and outcomes, upper limb defects were not considered in the pooled data analysis.
Bone transport over internal implants/all-inside bone transports
In an attempt to reduce fixator time, or avoid external fixation at all, various studies have investigated a combination of internal fixation with either distraction osteogenesis by external fixation or using a motorised transport nail [19, 21]. The combination of prolonged external fixation with internal fixation in the same segment raises significant concerns about deep infection, which is potentially devastating, particularly in this context [8, 19]. The complexity and variety of the techniques employed make the impact on docking site union difficult to interpret, with some protocols including routine plating or grafting of the docking site. Studies utilising internal fixation implants routinely as part of their surgical protocol were excluded from the pooled analysis.
Discussion
This review demonstrates that the management of docking sites remains a contentious issue, with a wide divergence of opinion on treatment protocols and ongoing research activity. Pooled analysis revealed an association in the literature between routine docking site intervention of any type and uneventful union. In those patients treated in this manner, 90% went on to union without further intervention, compared to 66% in patients where docking site procedures were only undertaken if spontaneous union did not occur.
Concerns regarding the risk of catastrophic complications, such as deep infection, threatening final treatment outcome following docking site exploration appear unfounded. Similar proportions of patients in each group went on to achieve union at the end of treatment in each group (99% in both). By the same logic, concerns that union may not be achieved as readily where docking site interventions are only undertaken when union does not arise spontaneously following simple compression are not supported by this data.
Whilst these findings initially appear to support the view that routine docking site intervention results in improved outcomes, one should consider that the mean number of procedures to attain union in the planned intervention group was higher than in the observed group (3.8 procedures per patient compared with 2.2), and this has implications for resource use and patient experience. The overall treatment time between the groups was similar. If we consider that 66% of patients in the observed group went on to spontaneous union without intervention at a similar time, then subjecting these patients to routine docking site procedures appears unnecessary. Adopting a watchful waiting approach might therefore be reasonable, carefully counselling the patient that around 1/3 of patients require further surgery to achieve union and undertaking this in a timely manner when required. Identifying patients at higher risk of non-union early for intervention would be helpful, and therefore, developing a protocol with evidence-based triggers for intervention would be a logical step. The most frequently reported risk factors for docking site non-union in the literature are shown in Table 4. Further research to explore these and develop a system to identify those at risk of non-union for planned intervention appears warranted.
This study is subject to limitations which should be considered when interpreting the results and applying them to clinical practice. The quality of reporting in the included studies was variable, and in a small number, it was not possible to extract sufficient data pertaining to the main outcome for inclusion. The proportion where this was not possible for secondary outcomes such as the number of procedures undertaken to union increased, resulting in missing data and smaller numbers of patients being considered. Where interventions of interest were included in a study, this was often in combination with others, making the effect of specific treatment strategies difficult to differentiate. The results of the pooled analysis are subject to all the shortcomings of the individual papers and therefore should be interpreted with caution. Though all the papers included segmental bone defects in the lower limb, these resulted from different pathologies. The treatment protocols were highly divergent between studies particularly with regard to the type of docking site intervention. Few studies were randomised, and particular cases will have been selected for different interventions for specific reasons, leading to potential selection bias. Furthermore, the outcome considered is subjective in that the decision to intervene due to the lack of progress at the docking site is taken by the treating surgeon usually without specific criteria. This means that patients in one group or the other may be managed differently, leading to these observed differences in outcome. As for the data as a whole, analysis of this nature is prone to significant confounding given the differences in patient groups from the different studies and differences in their management. It is not possible to undertake rigorous statistical analysis of the pooled continuous data, such as time to union and number of procedures, as presented in these papers. The results as presented here should therefore be taken at face value and interpreted with caution.
Conclusions
Based on the current literature, routine intervention at docking sites may be unwarranted, potentially leading to unnecessary intervention in two thirds of patients. Regardless of the location and the bone transport technique used, a timely selective intervention in those at high risk or after a defined period of observation would appear to be a logical approach. Patient preference should also be considered. Due to the heterogeneous nature of the studies, further research is needed to better understand risk factors for non-union.
References
Morwood MP, Streufert BD, Bauer A, Olinger C, Tobey D, Beebe M, Avilucea F, Buitrago AR, Collinge C, Sanders R, Mir H (2019) Intramedullary nails yield superior results compared with plate fixation when using the masquelet technique in the femur and tibia. J Orthop Trauma 33(11):547–552. https://doi.org/10.1097/BOT.0000000000001579
Stafford PR, Norris BL (2010) Reamer-irrigator-aspirator bone graft and bi Masquelet technique for segmental bone defect nonunions: a review of 25 cases. Injury 41(Suppl 2):S72–S77. https://doi.org/10.1016/S0020-1383(10)70014-0
Masquelet AC (2017) Induced membrane technique: pearls and pitfalls. J Orthop Trauma 31(Suppl 5):S36–S38. https://doi.org/10.1097/BOT.0000000000000979
Giannoudis PV, Faour O, Goff T, Kanakaris N, Dimitriou R (2011) Masquelet technique for the treatment of bone defects: tips-tricks and future directions. Injury 42(6):591–598. https://doi.org/10.1016/j.injury.2011.03.036
Dendrinos GK, Kontos S, Lyritsis E (1995) Use of the Ilizarov technique for treatment of non-union of the tibia associated with infection. J Bone Joint Surg Am 77(6):835–846. https://doi.org/10.2106/00004623-199506000-00004
Yin P, Ji Q, Li T, Li J, Li Z, Liu J, Wang G, Wang S, Zhang L, Mao Z, Tang P (2015) A systematic review and meta-analysis of Ilizarov methods in the treatment of infected nonunion of tibia and femur. PloS One 10(11):e0141973. https://doi.org/10.1371/journal.pone.0141973
Spiegelberg B, Parratt T, Dheerendra SK, Khan WS, Jennings R, Marsh DR (2010) Ilizarov principles of deformity correction. Ann R Coll Surg Engl 92(2):101–105. https://doi.org/10.1308/003588410X12518836439326
Liodakis E, Kenawey M, Krettek C, Wiebking U, Hankemeier S (2011) Comparison of 39 post-traumatic tibia bone transports performed with and without the use of an intramedullary rod: the long-term outcomes. Int Orthop 35(9):1397–1402. https://doi.org/10.1007/s00264-010-1094-5
Ilizarov GA (1989) The tension-stress effect on the genesis and growth of tissues: part II. The influence of the rate and frequency of distraction. Clin Orthop Relat Res 239:263–285
Kanellopoulos AD, Soucacos PN (2006) Management of nonunion with distraction osteogenesis. Injury 37(Suppl 1):S51–S55. https://doi.org/10.1016/j.injury.2006.02.041
El-Rosasy MA (2007) Acute shortening and re-lengthening in the management of bone and soft-tissue loss in complicated fractures of the tibia. J Bone Joint Surg Br 89(1):80–88. https://doi.org/10.1302/0301-620X.89B1.17595
Catagni MA, Azzam W, Guerreschi F, Lovisetti L, Poli P, Khan MS, Di Giacomo LM (2019) Trifocal versus bifocal bone transport in treatment of long segmental tibial bone defects. Bone Joint J 101-B(2):162–169. https://doi.org/10.1302/0301-620X.101B2.BJJ-2018-0340.R2
Yushan M, Ren P, Abula A, Alike Y, Abulaiti A, Ma C, Yusufu A (2020) Bifocal or trifocal (double-level) bone transport using unilateral rail system in the treatment of large tibial defects caused by infection: a retrospective study. Orthop Surg 12(1):184–193. https://doi.org/10.1111/os.12604
El-Alfy BS (2017) Unhappy triad in limb reconstruction: management by Ilizarov method. World J Orthop 8(1):42–48. https://doi.org/10.5312/wjo.v8.i1.42
Iacobellis C, Berizzi A, Aldegheri R (2010) Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strategies Trauma Limb Reconstr 5(1):17–22. https://doi.org/10.1007/s11751-010-0085-9
Krettek C, El Naga A (2017) All internal segmental bone transport and optional lengthening with a newly developed universal Cylinder-Kombi-Tube Module for motorized nails-description of a surgical technique. J Orthop Trauma 31(Suppl 5):S39–S41. https://doi.org/10.1097/BOT.0000000000000986
Barinaga G, Beason AM, Gardner MP (2018) Novel surgical approach to segmental bone transport using a magnetic intramedullary limb lengthening system. J Am Acad Orthop Surg 26(22):e477–e482. https://doi.org/10.5435/JAAOS-D-17-00487
Summers S, Krkovic M (2021) Bone transport with magnetic intramedullary nails in long bone defects. Eur J Orthop Surg Traumatol 31(6):1243–1252. https://doi.org/10.1007/s00590-020-02854-5
Park KH, Oh CW, Kim JW, Oh JK, Yoon YC, Seo I, Ha SS, Chung SH (2021) Matched comparison of bone transport using external fixator over a nail versus external fixator over a plate for segmental tibial bone defects. J Orthop Trauma 35(11):e397–e404. https://doi.org/10.1097/BOT.0000000000002084
Bas A, Daldal F, Eralp L, Kocaoglu M, Uludag S, Sari S (2020) Treatment of tibial and femoral bone defects with bone transport over an intramedullary nail. J Orthop Trauma 34(10):e353–e359. https://doi.org/10.1097/BOT.0000000000001780
Olesen UK, Nygaard T, Prince DE, Gardner MP, Singh UM, McNally MA, Green CJ, Herzenberg JE (2019) Plate-assisted bone segment transport with motorized lengthening nails and locking plates: a technique to treat femoral and tibial bone defects. J Am Acad Orthop Surg Glob Res Rev 3(8):e064. https://doi.org/10.5435/JAAOSGlobal-D-19-00064
Hamiti Y, Yushan M, Lu C, Yusufu A (2021) Reconstruction of massive tibial defect caused by osteomyelitis using induced membrane followed by trifocal bone transport technique: a retrospective study and our experience. BMC Surg 21(1):419. https://doi.org/10.1186/s12893-021-01421-x
Lovisetti G, Sala F, Miller AN, Thabet AM, Zottola V, Capitani D (2012) Clinical reliability of closed techniques and comparison with open strategies to achieve union at the docking site. Int Orthop 36(4):817–825. https://doi.org/10.1007/s00264-011-1260-4
Paley D, Maar DC (2000) Ilizarov bone transport treatment for tibial defects. J Orthop Trauma 14(2):76–85. https://doi.org/10.1097/00005131-200002000-00002
Sala F, Marinoni E, Miller AN, Pesenti G, Castelli F, Alati S, Coppadoro A, Capitani D (2013) Evaluation of an endoscopic procedure for the treatment of docking site nonunion. J Orthop Trauma 27(10):569–575. https://doi.org/10.1097/BOT.0b013e31829484f6
Spiegl U, Patzold R, Friederichs J, Hungerer S, Militz M, Buhren V (2013) Clinical course, complication rate and outcome of segmental resection and distraction osteogenesis after chronic tibial osteitis. Injury 44(8):1049–1056. https://doi.org/10.1016/j.injury.2013.05.003
Lovisetti G, Sala F (2013) Clinical strategies at the docking site of distraction osteogenesis: are open procedures superior to the simple compression of Ilizarov? Injury 44(Suppl 1):S58–S62. https://doi.org/10.1016/S0020-1383(13)70014-7
Kinik H, Kalem M (2021) Ilizarov segmental bone transport of infected tibial nonunions requiring extensive debridement with an average distraction length of 9,5 centimetres. Is it safe? Injury 52(8):2425–2433. https://doi.org/10.1016/j.injury.2019.12.025
Giotakis N, Narayan B, Nayagam S (2007) Distraction osteogenesis and nonunion of the docking site: is there an ideal treatment option? Injury 38(Suppl 1):S100–S107. https://doi.org/10.1016/j.injury.2007.02.015
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P (2010) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Int J Surg 8(5):336–341. https://doi.org/10.1016/j.ijsu.2010.02.007
Miraj F, Nugroho A, Dalitan IM, Setyarani M (2021) The efficacy of ilizarov method for management of long tibial bone and soft tissue defect. Ann Med Surg (Lond) 68:102645. https://doi.org/10.1016/j.amsu.2021.102645
Hatzokos I, Stavridis SI, Iosifidou E, Karataglis D, Christodoulou A (2011) Autologous bone marrow grafting combined with demineralized bone matrix improves consolidation of docking site after distraction osteogenesis. J Bone Joint Surg Am 93(7):671–678. https://doi.org/10.2106/JBJS.J.00514
Tetsworth K, Paley D, Sen C, Jaffe M, Maar DC, Glatt V, Hohmann E, Herzenberg JE (2017) Bone transport versus acute shortening for the management of infected tibial non-unions with bone defects. Injury 48(10):2276–2284. https://doi.org/10.1016/j.injury.2017.07.018
Liu Y, Yushan M, Liu Z, Liu J, Ma C, Yusufu A (2020) Complications of bone transport technique using the Ilizarov method in the lower extremity: a retrospective analysis of 282 consecutive cases over 10 years. BMC Musculoskelet Disord 21(1):354. https://doi.org/10.1186/s12891-020-03335-w
Sigmund IK, Ferguson J, Govaert GAM, Stubbs D, McNally MA (2020) Comparison of Ilizarov bifocal, acute shortening and relengthening with bone transport in the treatment of infected, segmental defects of the tibia. J Clin Med 9(2). https://doi.org/10.3390/jcm9020279
Huang Q, Ren C, Li M, Xu Y, Li Z, Lin H, Zhang K, Ma T (2021) Antibiotic calcium sulfate-loaded hybrid transport versus traditional Ilizarov bone transport in the treatment of large tibial defects after trauma. J Orthop Surg Res 16(1):568. https://doi.org/10.1186/s13018-021-02723-9
Huang Q, Xu Y, Lu Y, Ren C, Liu L, Li M, Wang Q, Li Z, Xue H, Zhang K, Ma T (2022) Acute shortening and re-lengthening versus antibiotic calcium sulfate-loaded bone transport for the management of large segmental tibial defects after trauma. J Orthop Surg Res 17(1):219. https://doi.org/10.1186/s13018-022-03109-1
Eralp L, Kocaoglu M, Celiktas M, Gulsen M (2016) Is acute compression and distraction superior to segmental bone transport techniques in chronic tibial osteomyelitis ? Comparison of distraction osteogenesis techniques. Acta Orthop Belg 82(3):599–609
Li Y, Shen S, Xiao Q, Wang G, Yang H, Zhao H, Shu B, Zhuo N (2020) Efficacy comparison of double-level and single-level bone transport with Orthofix fixator for treatment of tibia fracture with massive bone defects. Int Orthop 44(5):957–963. https://doi.org/10.1007/s00264-020-04503-2
Aktuglu K, Gunay H, Alakbarov J (2016) Monofocal bone transport technique for bone defects greater than 5 cm in tibia: our experience in a case series of 24 patients. Injury 47(Suppl 6):S40–S46. https://doi.org/10.1016/S0020-1383(16)30838-5
Saridis A, Panagiotopoulos E, Tyllianakis M, Matzaroglou C, Vandoros N, Lambiris E (2006) The use of the Ilizarov method as a salvage procedure in infected nonunion of the distal femur with bone loss. J Bone Joint Surg Br 88(2):232–237. https://doi.org/10.1302/0301-620X.88B2.16976
Blum AL, BongioVanni JC, Morgan SJ, Flierl MA, dos Reis FB (2010) Complications associated with distraction osteogenesis for infected nonunion of the femoral shaft in the presence of a bone defect: a retrospective series. J Bone Joint Surg Br 92(4):565–570. https://doi.org/10.1302/0301-620X.92B4.23475
Garcia FL, Picado CH, Garcia SB (2009) Histology of the regenerate and docking site in bone transport. Arch Orthop Trauma Surg 129(4):549–558. https://doi.org/10.1007/s00402-008-0587-9
Schell H, Duda GN, Peters A, Tsitsilonis S, Johnson KA, Schmidt-Bleek K (2017) The haematoma and its role in bone healing. J Exp Orthop 4(1):5. https://doi.org/10.1186/s40634-017-0079-3
Rhinelander FW (1974) Tibial blood supply in relation to fracture healing. Clin Orthop Relat Res 105:34–81
Data availability
Data and materials are available in the article.
Code availability
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by EL, VG and PH. The first draft of the manuscript was written by EL, and all authors commented on previous versions of the manuscript. PG supervised this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable. This is a review article.
Informed consent
Not applicable.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liodakis, E., Giannoudis, V.P., Harwood, P. et al. Docking site interventions following bone transport using external fixation: a systematic review of the literature. International Orthopaedics (SICOT) 48, 365–388 (2024). https://doi.org/10.1007/s00264-023-06062-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-023-06062-8