Abstract
Purposes
The aim of this study was to evaluate: 1. the outcome of pelvic ring fractures treated by closed reduction and percutaneous fixation, 2. the prognostic factors associated with a poor quality reduction, 3. the prognostic factors associated with ilio-sacral screws misplacement and 4. the prognostic factors associated with nonunion.
Methods
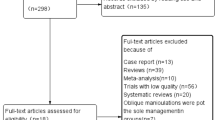
Data from medical charts for all patients admitted with unstable posterior pelvic ring injuries from 2009 to 2013 were extracted. A total of 165 patients with a mean age of 40 years were included. One hundred and five patients were reviewed at a mean of 32 months of follow-up. The prognostic factors analyzed were clinical and radiological factors. Tile B and Tile C pelvic ring fractures were compared and analyzed separately. Then specific statistical analysis was performed using a logistic regression model to eliminate confusion factors.
Results
An excellent or good clinical result was achieved for 94 patients (90%). An excellent or good reduction was achieved for 141 patients (85%). Nonunion rate, smoking patients, bad reductions, age of patients and ISS score were significantly higher in Tile C group. To eliminate confusion factors we used a multivariate analysis logistic regression model. Only unstable vertical bilateral posterior injuries (Tile C2 and C3) were independent prognostic factors for unsatisfactory reduction (p = 0.001; OR = 4.72; CI 95% [2.08–16.72]). Screw misplacement was recorded for 30 patients (16%) and sacral dysmorphia was an associated prognostic factor (p = 0.0001; OR = 15.6; CI95% [3.41–98.11]). Nonunion was recorded for ten patients (6%) and smoking was an associated prognostic factor (p = 0.01, OR = 5.12; CI95% [1.1–24.1]).
Conclusions
Posterior pelvic ring fractures treated by closed reduction and percutaneous fixation are associated with excellent/good clinical results if excellent/good reduction and bone healing are achieved without screw misplacement. Bilateral unstable vertical posterior pelvic ring injuries, and sacral dysmorphia are risk factors for bad quality reduction and screw misplacement respectively.


Similar content being viewed by others
References
Pennal GF, Tile M, Waddell JP, Garside H (1980) Pelvic disruption: assessment and classification. Clin Orthop Relat Res 151:12–21
Ruatti S, Guillot S, Brun J, Thony F, Bouzat P, Payen JF, Tonetti J (2015) Which pelvic ring fractures are potentially lethal? Injury 46:1059–1063
Gänsslen A, Pohlemann T, Paul C, Lobenhoffer P, Tscherne H (1996) Epidemiology of pelvic ring injuries. Injury 27(Suppl 1):S-A13-20
Papakostidis C, Kanakaris NK, Kontakis G, Giannoudis PV (2009) Pelvic ring disruptions: treatment modalities and analysis of outcomes. Int Orthop 33:329–338
Routt ML Jr, Kregor PJ, Simonian PT, Mayo KA (1995) Early results of percutaneous iliosacral screws placed with the patient in the supine position. J Orthop Trauma 9:207–214
Goldstein A, Phillips T, Sclafani SJ, Scalea T, Duncan A, Goldstein J, Panetta T, Shaftan G (1986) Early open reduction and internal fixation of the disrupted pelvic ring. J Trauma 26:325–333
Lindsay A, Tornetta P 3rd, Diwan A, Templeman D (2016) Is closed reduction and percutaneous fixation of unstable posterior ring injuries as accurate as open reduction and internal fixation? J Orthop Trauma 30:29–33
Wang H, Wang F, Leong AP, Xu L, Chen X, Wang Q (2016) Precision insertion of percutaneous sacroiliac screws using a novel augmented reality-based navigation system: a pilot study. Int Orthop 40:1941–1947
Majeed SA (1989) Grading the outcome of pelvic fractures. J Bone Joint Surg Br 71:304–306
Denis F, Davis S, Comfort T (1988) Sacral fractures: an important problem. Retrospective analysis of 236 cases. Clin Orthop Relat Res 227:67–81
Tornetta P 3rd, Matta JM (1996) Outcome of operatively treated unstable posterior pelvic ring disruptions. Clin Orthop Relat Res 329:186–193
Lefaivre KA, Starr AJ, Barker BP, Overturf S, Reinert CM (2009) Early experience with reduction of displaced disruption of the pelvic ring using a pelvic reduction frame. The Journal of bone and joint surgery British 91:1201–1207
Thaunat M, Laude F, Paillard P, Saillant G, Catonné Y (2008) Transcondylar traction as a closed reduction technique in vertically unstable pelvic ring disruption. Int Orthop 32:7–12
Oliver CW, Twaddle B, Agel J, Routt ML Jr (1996) Outcome after pelvic ring fractures: evaluation using the medical outcomes short form SF-36. Injury 27:635–641
Boyoud-Garnier L, Boudissa M, Ruatti S, Kerschbaumer G, Grobost P, Tonetti J (2017) Chronic low back pain after lumbosacral fracture due to sagittal and frontal vertebral imbalance. Orthop Traumatol Surg Res 103:523–526
Grossterlinden L, Rueger J, Catala-Lehnen P, Rupprecht M, Lehmann W, Rücker A, Briem D (2011) Factors influencing the accuracy of iliosacral screw placement in trauma patients. Int Orthop 35:1391–1396
Pishnamaz M, Dienstknecht T, Hoppe B, Garving C, Lange H, Hildebrand F, Kobbe P, Pape HC (2016) Assessment of pelvic injuries treated with Ilio-sacral screws: injury severity and accuracy of screw positioning. Int Orthop 40:1495–1501
Mears DC, Velyvis J (2003) Surgical reconstruction of late pelvic post-traumatic nonunion and malalignment. J Bone Joint Surg Br 85:21–30
Tripathy SK, Goyal T, Sen RK (2015) Nonunions and malunions of the pelvis. Eur J Trauma Emerg Surg 41:335–342
Wright JL, Nathens AB, Rivara FP, MacKenzie EJ, Wessells H (2006) Specific fracture configurations predict sexual and excretory dysfunction in men and women 1 year after pelvic fracture. J Urol 176:1540–1545
Lindahl J, Hirvensalo E (2005) Outcome of operatively treated type-C injuries of the pelvic ring. Acta Orthop 76:667–678
Reilly MC, Zinar DM, Matta JM (1996) Neurologic injuries in pelvic ring fractures. Clin Orthop Relat Res 329:28–36
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest concerning this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of Evidence: Level 4, retrospective study
Rights and permissions
About this article
Cite this article
Boudissa, M., Roudet, A., Fumat, V. et al. Part 1: Outcome of Posterior Pelvic Ring Injuries and Associated Prognostic Factors – A Five-Year Retrospective Study of One Hundred and Sixty Five Operated Cases with Closed Reduction and Percutaneous Fixation. International Orthopaedics (SICOT) 44, 1209–1215 (2020). https://doi.org/10.1007/s00264-020-04574-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-020-04574-1