Abstract
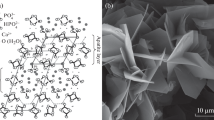
This study aims to evaluate in detail the biological osteoconductive properties of the low-temperature synthetic porous calcium-deficient hydroxyapatite and to compare it with the biological apatite. Bone reactions to granules of similar sizes of the low-temperature hydroxyapatite and commercially available non-sintered deproteinized bovine bone were compared. Two different temperatures were used to fabricate two batches of newly developed porous hydroxyapatite with different carbonate groups content and specific surface area. The histological analysis of specimens with histomorphometry was performed at different time after in vivo implantation. Based on histological analysis, the level of bone formation in the spaces between the implanted granules and through the interconnected pores of all implanted materials within a cortical region (bone area ingrowth 72–85 %) was several-fold higher than within a cancellous bone site (bone area ingrowth 16–28 %) at three and six months after implantation. Within the cancellous bone site, bone coverage of the implanted material at six months was significantly higher in hydroxyapatite material fabricated using low-temperature synthesis and subsequent processing at 150°C than in hydroxyapatite scaffold developed using low-temperature synthesis with subsequent processing at 700°C or deproteinized bovine bone. According to our study, the bioactive properties of the low-temperature calcium-deficient hydroxyapatite are comparable with the biological apatite. The favourable influence of a high specific surface area of a low-temperature calcium-deficient hydroxyapatite on in vivo bone formation was emphasized.





Similar content being viewed by others
References
Hirn M, de Silva U, Sidharthan S, Grimer RJ, Abudu A, Tillman RM, Carter SR (2009) Bone defects following curettage do not necessarily need augmentation. A retrospective study of 146 patients. Acta Orthop 80:4–8
Sponer P, Urban K, Urbanova E, Karpas K, Mathew PG (2009) Behavior of nonresorbable bioactive glass-ceramic implanted into long bone defects: comparison with cancellous allografts. Arch Orthop Trauma Surg 129:1353–1360
Pecina M, Vukicevic S (2007) Biological aspects of bone, cartilage and tendon regeneration. Int Orthop 31:719–720
McKay WF, Peckham SM, Badura JM (2007) A comprehensive clinical review of recombinant human bone morphogenetic protein-2 (INFUSE® Bone Graft). Int Orthop 31:729–734
White AP, Vaccaro AR, Hall JA, Whang PG, Friel BC, McKee MD (2007) Clinical applications of BMP-7/OP-1 in fractures, nonunions and spinal vision. Int Orthop 31:735–741
Bishop GB, Einhorn TA (2007) Current and future clinical applications of bone morphogenetic proteins in orthopaedic trauma surgery. Int Orthop 31:721–727
Wopenka B, Pasteris JD (2005) A mineralogical perspective on the apatite in bone. Mater Sci Eng C Biomim Mater Sens Syst 25:131–143
Honig JF, Merten HA, Heinemann DE (1999) Risk of transmission of agents associated with Creutzfeldt-Jakob disease and bovine spongiform encephalopathy. Plast Reconstr Surg 103:1324–1325
Donath K, Breuner GA (1982) A method for the study of undecalcified bones and teeth with attached soft tissues—the sage-schliff (sawing and grinding) technique. J Oral Pathol 11:318–326
Hench LL, Polak JM (2002) Third-generation biomedical materials. Science 295:1014–1017
Wetzel AC, Stich H, Caffesse RG (1995) Bone apposition onto oral implants in the sinus area filled with different grafting materials. A histological study in beagle dogs. Clin Oral Implants Res 6:155–163
Hartl A, Bitzan P, Wanivenhaus A, Kotz R (2004) Faster integration of human allograft bone than of the bovine substitute Lubboc. Non-randomized evaluation of 20 cases with benign tumors or tumor-like conditions. Acta Orthop Scand 75:217–220
Briem D, Linhart W, Lehmann W, Meenen NM, Rueger JM (2002) Long-term results after application of a porous hydroxyapatite ceramic (Endobon) in proximal tibia fractures. Unfallchirurg 105:128–133
Meyer S, Floerkemeier T, Windhagen H (2008) Histological osseointegration of Tutobone®: First results in human. Arch Orthop Trauma Surg 128:539–544
Traini T, Valentini P, Iezzi G, Piattelli A (2007) A histologic and histomorphometric evaluation of anorganic bovine bone retrieved 9 years after a sinus augmentation procedure. J Periodontol 78:955–961
Ramaswamy Y, Haynes DR, Berger G et al (2005) Bioceramics composition modulate resorption of human osteoclasts. J Mater Sci Mater Med 16:1199–1205
Flautre B, Descamps M, Delecourt C, Blary MC, Hardouin P (2001) Porous HA ceramic for bone replacement: role of the pores and interconnections—experimental study in the rabbit. J Mater Sci Mater Med 12:679–682
Itala AI, Ylanen HO, Ekholm C, Karlsson KH, Aro HT (2001) Pore diameter of more than 100 mm is not requisite for bone ingrowth in rabbits. J Biomed Mater Res 58:679–683
Pilliar RM, Filiaggi MJ, Wells JD, Grynpas MD, Kandel RA (2001) Porous calcium polyphosphate scaffolds for bone substitute applications—in vitro characterization. Biomaterials 22:963–972
Tamai N, Myoui A, Tomita T, Nakase T, Tanaka J, Ochi T et al (2002) Novel hydroxyapatite ceramics with an interconnective porous structure exhibit superior osteoconduction in vivo. J Biomed Mater Res 59:110–117
Kuroda T (1995) Bone formation and mechanical properties of the cancellous bone defect site filled with hydroxyapatite granules. Nippon Seikeigeka Gakkai Zasshi 69:1037–1049
Lu JX, Gallur A, Flautre B, Anselme K, Deschamps M, Thierry B, Hardouin P (1998) Comparative study of tissue reactions to calcium phosphate ceramics among cancellous, cortical, and medullar bone sites in rabbits. J Biomed Mater Res 42:357–367
Hench LL (2000) Bioactive glasses and ceramics. In: Yamamuro T, Hench LL, Wilson J (eds) Handbook of bioactive ceramics. Boca Raton, CRC Press
Afonso A, Santos JD, Vasconcelos M, Branco R, Cavalheiro J (1996) Granules of osteopatite and glass-reinforced hydroxyapatite implanted in rabbit tibiae. J Mater Sci Mater Med 7:507–510
Bostrom MPG, Seigerman DA (2005) The clinical use of allografts, demineralized bone matrice, synthetic bone graft substitutes and osteoinductive growth factors: A survey study. HSS J 1:9–18
Ogose A, Hotta T, Kawashima H, Kondo N, Gu W, Kamura T, Endo N (2005) Comparison of hydroxyapatite and beta tricalcium phosphate as bone substitutes after excision of bone tumors. J Biomed Mater Res B Appl Biomater 72B:94–101
Schwarz C, Bornei CR (2005) Biphasic phospho-calcium ceramics used as bone substitutes are efficient in the management of severe acetabular bone loss in revision total hip arthroplasties. Eur J Orthop Surg Traumatol 15:191–196
Mankani MH, Kuznetsov SA, Fowler B, Kingman A, Gehron Robey P (2001) In vivo bone formation by human bone marrow stromal cells: effect of carrier particle size and shape. Biotechnol Bioeng 72:96–107
Cordonnier T, Layrolle P, Gaillard J, Langonne A, Sensebe L, Rosset P, Sohier J (2010) 3D environment on human mesenchymal stem cells differentiation for bone tissue engineering. J Mater Sci Mater Med 21:981–987
Kasten P, Beyen I, Niemeyer P, Luginbühl R, Bohner M, Richter W (2008) Porosity and pore size of β-tricalcium phosphate scaffold can influence protein production and osteogenic differentiation of human mesenchymal stem cells: An in vitro and in vivo study. Acta Biomater 4:1904–1915
Kasten P, Vogel J, Luginbühl R, Niemeyer P, Tonak M, Lorenz H, Helbig L, Weiss S, Fellenberg J, Leo A, Simank HG, Richter W (2005) Ectopic bone formation associated with mesenchymal stem cells in a resorbable calcium deficient hydroxyapatite carrier. Biomaterials 26:5879–5889
Conflict of interest statement
None of the authors have a conflict of interest in relation to the content of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Šponer, P., Strnadová, M. & Urban, K. In vivo behaviour of low-temperature calcium-deficient hydroxyapatite: comparison with deproteinised bovine bone. International Orthopaedics (SICOT) 35, 1553–1560 (2011). https://doi.org/10.1007/s00264-010-1113-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-010-1113-6