Abstract
Background
Pre-clinical data have revealed that viral infection, such as Hepatitis B virus (HBV), Hepatitis C virus (HCV), and Human Papilloma virus (HPV), may lead to the development of “hot” or “immune-sensitive” tumors, which may impact the efficacy of immune checkpoint inhibitor (ICIs). Therefore, This study aimed to investigate the impact of viral status on the efficacy of ICIs.
Methods
Electronic databases were searched to identify relevant trials. The primary endpoints were overall survival (OS) and progression-free survival (PFS) measured by hazard ratio (HR). Stratified analyses were accomplished based on viral types, treatment regimens, and patient locations.
Results
A total of 3255 participants were recruited, including 252 cases of gastric cancer, 156 cases of nasopharyngeal carcinoma, 1603 cases of hepatocellular carcinoma, and 1244 cases of head and neck squamous cell carcinoma. Pooled results demonstrated a significant association between viral infection and favorable outcomes in patients receiving ICIs, including improved OS [HR = 0.67, 95%CI (0.57–0.79), P < 0.0001], increased ORR [OR = 1.43, 95%CI (1.14–1.80), P = 0.0018], and a trend toward enhanced PFS [HR = 0.75, 95%CI (0.56–1.00), P = 0.05]. In subgroup analyses, patients treated with ICIs who were exposed to HBV/HCV or HPV infection exhibited an evidently superior OS without heterogeneity, compared to those without infection.
Conclusions
This study indicated that the presence of viral infection was evidently associated with improved outcomes in cancer patients undergoing ICIs, particularly in cases of HBV/HCV and HPV infections.
Similar content being viewed by others
Introduction
Immune checkpoint inhibitors (ICIs) have revolutionized the field of cancer treatment [1,2,3,4]. This groundbreaking approach has shifted the focus from indiscriminate targeting of cancer cells by traditional chemotherapy to enhancing the immune system's ability to selectively attack tumor cells. However, the efficacy of ICIs is still far from satisfactory due to resistance [5, 6], and the distinction of biomarkers of response is an intense area of research [7]. This could potentially be linked to the variability observed in the tumor microenvironment (TME) across different types of tumors [8, 9]. Thus, it is crucial to identify the populations that benefit from ICIs treatment.
Based on the infiltration of T cells, Chen and Mellman have classified the tumor immune microenvironment into three different phenotypes: immune-desert, immune-excluded, and immune-inflamed. Among them, the immune-desert and immune-excluded phenotypes, also known as “cold tumors”, were non-inflamed tumors that were typically insensitive to ICIs. In contrast, the immune-inflamed phenotype, referred to as "hot tumors", exhibited a significantly stronger response to ICIs [8, 10]. Studies demonstrated that tumors associated viral infection often exhibit an “hot tumor” [11, 12]. However, the impact of viral infection in tumors on the efficacy of ICIs remains a topic of debate in clinical practice, with no established consensus. While some researchers supported a positive impact [13, 14], others advocated for non-inferior survival outcome [15, 16]. Additionally, the types of tumors, viruses and ICIs were various. Therefore, it remains to be fully illuminated that the impact of viral status on the efficacy of ICIs in cancer patients.
Previous studies had preliminarily explored the effect of human papilloma virus (HPV) on ICIs through meta-analysis [17], but they focused on single type of tumor and lack of subgroup analyses. Here, we conducted a comprehensive survey based on a large sample size (29 cohorts incorporating 3,255 individuals), multiple types of viruses and tumors to evaluate the impact of viral status on ICIs efficacy for malignancies.
Materials and methods
Literature searches
PubMed, Cochrane Library, and EMBASE were systematically searched to identify relevant studies up until December 15th, 2023 by entering the following keywords: “immune checkpoint inhibitors”, “ICI”, “immunotherapy”, “PD-1”, “PD-L1”, “CTLA-4”, “programmed cell death protein 1”, “programmed cell death protein ligand 1”, “cytotoxic T lymphocyte-associated protein 4”, “pembrolizumab”, “nivolumab”, “atezolizumab”, “ipilimumab”, “tremelimumab”, “avelumab”, “durvalumab”, “carelizumab”, “tislelizumab”, “cemiplimab”, “toripalimab”, “penpulimab”, “cemiplimab”, “adebrelimab”, “sugemalimab”, “Epstein Barr virus”, “EBV”, “Hepatitis B virus”, “HBV”, “Human Papilloma virus”, “HPV”, “hepatitis C virus”, “HCV”, “gastric cancer”, “GC”, “stomach Cancer”, “hepatic cancer”, “liver cancer”, “HCC”, “nasopharyngeal carcinoma”, “NPC”, “head and neck cancer”, “HNSCC”, “lymphoma”, “cancer”, “neoplasm”, “tumor”, “carcinoma”, and “malignancy”. Moreover, the reference lists of related articles were scrutinized for additional studies.
Selection of studies
Two investigators respectively performed an initial screening of titles and abstracts, and then scrutinized the full texts to identify eligible studies.
Inclusion criteria
Inclusion criteria were included: (1) individuals were pathologically confirmed as malignancies; (2) therapeutic outcomes were analyzed on the efficacy of ICIs according to viral status (including Epstein Barr virus (EBV), hepatitis B virus (HBV), hepatitis C virus (HCV), and HPV; (3) A hazard ratio (HR) accompanied by a 95% confidence interval (CI) for progression-free survival (PFS) and/or overall survival (OS) and/or odds ratios (OR) with 95% CI for objective response rate (ORR) could be obtained or calculated from the original literature.
Data extraction
Data from all enrolled studies were independently collected by two investigators. The data was collected from each publication as follow: publication year, first author, number of patients, primary tumor, immunotherapy agents, viral types, HR for OS and/or PFS, and OR for ORR between the viral infection group and viral uninfection group.
Quality assessment
The quality of studies was assessed using the Newcastle–Ottawa quality assessment scale (NOS), with scores of more than six indicating medium to high quality [18]. Discrepancies were settled through a consensus reached among all investigators.
Statistical methods
The primary endpoints of the study were OS and PFS. The association between viral status (infection vs uninfection) and the efficacy ICIs was measured applying HR with the corresponding 95% CI. Subgroup analyses were accomplished based on the viral types, treatment regimen, patient locations, and ICI agents. Statistical analysis was performed by R 4.2.2 statistical software. Heterogeneity was evaluated through the I-square tests and Cochran’s Q test. if P < 0.05 or I2 > 50%, it indicated remarkable heterogeneity, and a random effect model was employed. Otherwise, a fixed effect model was adopted. Publication bias was assessed using funnel plot, Egger’s test, and trim-and-fill method [19].
Results
Study selection and characteristics of trials
A total of 18,347 potentially relevant articles were intensively scrutinized. Among them, 1,658 were removed for duplication, while 16,689 were filtered out for digressing from the subject after screening the titles and abstracts. Subsequently, the full texts of 163 articles were thoroughly reviewed, of which 134 were excluded for the following reasons: repeated study cohort (n = 23), unavailable data to evaluate the efficacy of ICIs (n = 47), non-human research (n = 22), reviews or meta-analysis (n = 42). Finally, a total of 29 studies incorporating 3,255 participants were identified (The links of original article and details were shown in Supplementary 1). The elaborate procedure is displayed in Fig. 1.
A total of 3255 individuals in 13 retrospective studies and 16 prospective studies were recruited. All 29 adopted studies were rated as moderate or high quality. Furthermore, the sample size ranged from 12 to 421. Of these studies, 3 focused on gastric cancer (GC), 1 on nasopharyngeal carcinoma (NPC), 14 on hepatocellular carcinoma (HCC), 11 on headneck squamous cell carcinoma (HNSCC). Principal traits and details were presented in Table 1.
Main results
The impact of viral status on malignancy patients treated with ICIs
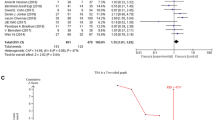
Pooled results showed that tumor patients with viral infection who received ICI agents had a significantly favorable OS [HR = 0.67, 95%CI (0.57–0.79), P < 0.0001] by a random-effect model (I2 = 42%, P = 0.02) (Fig. 2a), and a trend towards improved PFS [HR = 0.75, 95%CI (0.56–1.00), P = 0.05] based on a random-effect model (I2 = 58%, P < 0.01)(Fig. 2b). Furthermore, There was an increased ORR [OR = 1.43, 95%CI (1.14–1.80), P = 0.0018] in viral positive group according to a fixed-effect model (I2 = 12%, P = 0.31) (Fig. 2c).
Subgroup analysis for the impact of viral status
We performed subgroup based on the viral types, treatment regimen, and patient locations (Fig. 3a–i). The result showed that patients treated with ICIs who were exposed to HBV/HCV or HPV infection exhibited an evidently superior OS without heterogeneity, compared to those without HBV/HCV [HR = 0.79, 95%CI (0.65–0.96)] and HPV [HR = 0.64, 95%CI (0.53–0.76)]. While the OS was similar between the EBV-positive group and the EBV-negative group [HR = 0.58, 95%CI (0.21–1.63)] (Fig. 3a). Furthermore, we found that patients with viral infection who received ICIs had a significantly better OS, in contrast to those without infection, regardless of the treatment types (monotherapy or combined therapy) [HR = 0.64, 95%CI (0.54–0.75) and HR = 0.78, 95%CI (0.64–0.94), respectively] (Fig. 3b) and patient locations (eastern countries or western countries) [HR = 0.68, 95%CI (0.55–0.84) and HR = 0.57, 95%CI (0.45–0.71), respectively] (Fig. 3c). Additionally, the groups with HBV/HCV or HPV infection achieved a higher ORR compared to the groups without HBV/HCV or HPV infection)[OR = 1.58, 95%CI (1.19–2.10) and OR = 1.57, 95%CI (1.0–2.47), respectively] (Fig. 3g).
a The pooled HRs for overall survival (OS) stratified on viral types (EBV, HBV/HCV, and HPV); b treatment regions (monotherapy or combined therapy); c patients locations (western countries and eastern countries); d the pooled HRs for progression-free survival (PFS) stratified on viral types; e treatment regions; f patients locations; g the pooled ORs for objective response rate (ORR) stratified on viral types; h treatment regions; i patients locations
Publication bias
The shape of the funnel plot suggested no publication bias for recruited studies on PFS (Egger: P = 0.11) (Fig. 4a) and ORR (Egger: P = 0.98) (Fig. 4b). However, there was a publication bias for OS (Egger: P = 0.02) (Fig. 4c). Nevertheless, in the results of the trim and fill method, the publication bias corrected overall effect size was 0.76 (95% CI: 0.62–0.93) (Fig. 4d), even though the effect size increased compared to the original ones. This implied that the results obtained for this study were reliable and consistent.
The sensitivity analysis
Sensitivity analyses were performed by excluding one single study from the primary analyses. The results showed that no single study significantly influenced the pooled HRs or ORs, suggesting that the data of this meta-analysis were relatively credible and stable (Fig. 5).
Discussion
Recently, increasing evidences highlighted the importance of viral infection in influencing the efficacy of immunotherapy. Pre-clinical and clinical evidences have recognized that the viral infection may play a crucial role in boosting the immune response and improve prognosis of cancer patients undergoing ICIs treatment [11,12,13,14]. To the best of our knowledge, this study was firstly investigated the impact of viral infection on outcomes of cancer patients treated with ICIs based on a comprehensive survey (29 cohorts incorporating 3,255 individuals), multiple viruses types (EBV, HBV, HCV, and HPV) and multiple tumor types (including GC, NPC, HCC and HNSCC). The result demonstrated a significant association between viral infection and improved outcomes for cancer patients receiving ICIs treatment.
Mechanically, PD-1 and its ligands played a crucial role in enabling tumor cells to evade the anti-tumor response of immune system [20]. Less widely recognized was that the PD-1/PD-L1 axis also played a role in regulating immune responses against viral infection and can be influenced by various viruses [21, 22]. Upregulation of PD-1 and its ligands PD-L1 were observed during acute viral infection and after infection with persistent viruses including important human pathogens such as HBV, HCV, and EBV [23,24,25,26]. Moreover, viral infection associated carcinomas were typically characterized by abundant immune cell infiltration [11, 12], which might further positively affect the efficacy of ICIs.
Notably, our study exhibited that EBV infection did not impact the efficacy of ICI treatment, despite the frequent association of EBV infection with high PD-L1 expression in tumors was discovered [25, 26]. The reason remains to be elucidated. However, it should be noted this study comprising EBV associated tumors was only included 4 cohorts with a total of 408 participants. Therefore, caution should be advised when interpreting the result.
However, this study encountered two flaws: firstly, some of recruited studies were retrospective, although we had comprehensively analyzed the articles; secondly, due to the limited availability of comprehensive data, subgroup analysis based on specific ICI agents could not be conducted.
In conclusion, this study demonstrated that the presence of viral infection was positively associated with better outcomes, with improved OS, increased ORR, and potential benefits in PFS in cancer patients undergoing ICIs therapy. And subgroup analyses on therapy regimen and patient locations exhibited similar results, indicating the positive impact of viral infection on ICIs therapy in clinical practice.
Data availability
All data and material analyzed during this study are included in the published article.
References
Atkins MB, Plimack ER, Puzanov I, Fishman MN, McDermott DF, Cho DC et al (2018) Axitinib in combination with pembrolizumab in patients with advanced renal cell cancer: a non-randomised, open-label, dose-finding, and dose-expansion phase 1b trial. Lancet Oncol 19(3):405–415. https://doi.org/10.1016/s1470-2045(18)30081-0
Kudo M, Finn RS, Edeline J, Cattan S, Ogasawara S, Palmer DH et al (2022) Updated efficacy and safety of KEYNOTE-224: a phase II study of pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib. Eur J Cancer 167:1–12. https://doi.org/10.1016/j.ejca.2022.02.009
Ribas A, Hamid O, Daud A, Hodi FS, Wolchok JD, Kefford R et al (2016) Association of pembrolizumab with tumor response and survival among patients with advanced melanoma. JAMA 315(15):1600–1609. https://doi.org/10.1001/jama.2016.4059
Burtness B, Harrington KJ, Greil R, Soulières D, Tahara M, de Castro G, Jr. et al (2019) Pembrolizumab alone or with chemotherapy versus cetuximab with chemotherapy for recurrent or metastatic squamous cell carcinoma of the head and neck (KEYNOTE-048): a randomised, open-label, phase 3 study. Lancet 394(10212):1915–1928. https://doi.org/10.1016/s0140-6736(19)32591-7
Larkin J, Chiarion-Sileni V, Gonzalez R, Grob JJ, Rutkowski P, Lao CD et al (2019) Five-year survival with combined Nivolumab and Ipilimumab in advanced melanoma. N Engl J Med 381(16):1535–1546. https://doi.org/10.1056/NEJMoa1910836
Garon EB, Hellmann MD, Rizvi NA, Carcereny E, Leighl NB, Ahn MJ et al (2019) Five-year overall survival for patients with advanced non-small-cell lung cancer treated with pembrolizumab: results from the phase I KEYNOTE-001 study. J Clin Oncol 37(28):2518–2527. https://doi.org/10.1200/jco.19.00934
Darvin P, Toor SM, Sasidharan Nair V, Elkord E (2018) Immune checkpoint inhibitors: recent progress and potential biomarkers. Exp Mol Med 50(12):1–11. https://doi.org/10.1038/s12276-018-0191-1
Rizvi NA, Hellmann MD, Snyder A, Kvistborg P, Makarov V, Havel JJ et al (2015) Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 348(6230):124–128. https://doi.org/10.1126/science.aaa1348
El Sayed R, Haibe Y, Amhaz G, Bouferraa Y, Shamseddine A (2021) Metabolic factors affecting tumor immunogenicity: what is happening at the cellular level? Int J Mol Sci 22(4):2142. https://doi.org/10.3390/ijms22042142
Chen PL, Roh W, Reuben A, Cooper ZA, Spencer CN, Prieto PA et al (2016) Analysis of immune signatures in longitudinal tumor samples yields insight into biomarkers of response and mechanisms of resistance to immune checkpoint blockade. Cancer Discov 6(8):827–837. https://doi.org/10.1158/2159-8290.Cd-15-1545
Lei Y, Cao P, Zheng X, Wei J, Cheng M, Liu M (2023) Perspectives for immunotherapy of EBV-associated GLELC: a relatively “hot” tumor microenvironment. Cancer Med 12(19):19838–19849. https://doi.org/10.1002/cam4.6555
Gameiro SF, Evans AM, Mymryk JS (2022) The tumor immune microenvironments of HPV(+) and HPV(−) head and neck cancers. WIREs Mech Dis 14(2):e1539. https://doi.org/10.1002/wsbm.1539
Bai Y, Xie T, Wang Z, Tong S, Zhao X, Zhao F et al (2022) Efficacy and predictive biomarkers of immunotherapy in Epstein-Barr virus-associated gastric cancer. J Immunother Cancer 10(3):e004080. https://doi.org/10.1136/jitc-2021-004080
Powell SF, Gold KA, Gitau MM, Sumey CJ, Lohr MM, McGraw SC et al (2020) Safety and Efficacy of pembrolizumab with chemoradiotherapy in locally advanced head and neck squamous cell carcinoma: a phase IB study. J Clin Oncol 38(21):2427–2437. https://doi.org/10.1200/jco.19.03156
Bauml J, Seiwert TY, Pfister DG, Worden F, Liu SV, Gilbert J et al (2017) Pembrolizumab for platinum- and cetuximab-refractory head and neck cancer: results from a single-arm. Phase II Study J Clin Oncol 35(14):1542–1549. https://doi.org/10.1200/jco.2016.70.1524
Tada T, Kumada T, Hiraoka A, Kariyama K, Tani J, Hirooka M et al (2023) New prognostic system based on inflammation and liver function predicts prognosis in patients with advanced unresectable hepatocellular carcinoma treated with atezolizumab plus bevacizumab: a validation study. Cancer Med 12(6):6980–6993. https://doi.org/10.1002/cam4.5495
Xu Y, Zhu G, Maroun CA, Wu IXY, Huang D, Seiwert TY et al (2021) Programmed death-1/programmed death-ligand 1-axis blockade in recurrent or metastatic head and neck squamous cell carcinoma stratified by human papillomavirus status: a systematic review and meta-analysis. Front Immunol 12:645170. https://doi.org/10.3389/fimmu.2021.645170
Stang A (2010) Critical evaluation of the Newcastle–Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 25(9):603–605. https://doi.org/10.1007/s10654-010-9491-z
Duval S, Tweedie R (2000) Trim and fill: a simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics 56(2):455–463. https://doi.org/10.1111/j.0006-341x.2000.00455.x
Jiang X, Wang J, Deng X, Xiong F, Ge J, Xiang B et al (2019) Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Mol Cancer 18(1):10. https://doi.org/10.1186/s12943-018-0928-4
Attanasio J, Wherry EJ (2016) Costimulatory and coinhibitory receptor pathways in infectious disease. Immunity 44(5):1052–1068. https://doi.org/10.1016/j.immuni.2016.04.022
Schönrich G, Raftery MJ (2019) The PD-1/PD-L1 axis and virus infections: a delicate balance. Front Cell Infect Microbiol 9:207. https://doi.org/10.3389/fcimb.2019.00207
Huang ZY, Xu P, Li JH, Zeng CH, Song HF, Chen H et al (2017) Clinical significance of dynamics of programmed death ligand-1 expression on circulating CD14(+) monocytes and CD19(+) B cells with the progression of hepatitis B virus infection. Viral Immunol 30(3):224–231. https://doi.org/10.1089/vim.2016.0122
Zhai N, Li H, Song H, Yang Y, Cui A, Li T et al (2017) Hepatitis C virus induces MDSCs-like monocytes through TLR2/PI3K/AKT/STAT3 signaling. PLoS ONE 12(1):e0170516. https://doi.org/10.1371/journal.pone.0170516
Ge J, Wang J, Xiong F, Jiang X, Zhu K, Wang Y et al (2021) Epstein-barr virus-encoded circular RNA CircBART2.2 promotes immune escape of nasopharyngeal carcinoma by regulating PD-L1. Cancer Res 81(19):5074–5088. https://doi.org/10.1158/0008-5472.Can-20-4321
Li X, Zhang W (2021) Expression of PD-L1 in EBV-associated malignancies. Int Immunopharmacol 95:107553. https://doi.org/10.1016/j.intimp.2021.107553
Funding
This research was supported by the Education Research Fund for Young and Middle-aged Teachers of Fujian Province (Numbers JAT231028).
Author information
Authors and Affiliations
Contributions
XX, CW, LW and YK: Conceptualization, Methodology. CW and YK: Data curation, Software, Validation, Writing—Original draft preparation. CW and LW: Visualization, Investigation. XX: Supervision. XX, CW, YK and LW: Writing—Reviewing and Editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wu, C., Ke, Y., Wan, L. et al. Efficacy of immune checkpoint inhibitors differs in various status of carcinoma: a study based on 29 cohorts with 3255 participants. Cancer Immunol Immunother 73, 79 (2024). https://doi.org/10.1007/s00262-024-03663-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00262-024-03663-z